Abstract
Purpose
Hypotensive bradycardic events (HBEs) occur in 5–28 % of patients undergoing arthroscopic shoulder surgery in the sitting position after an interscalene brachial plexus block (ISBPB). The objective of this study was to investigate the effects of the sitting position following ISBPB on heart rate variability (HRV).
Methods
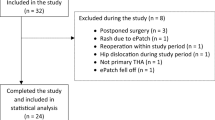
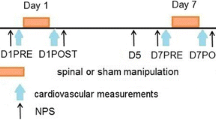
In this prospective case–control study, we evaluated 64 patients undergoing arthroscopic shoulder surgery under ISBPB and 49 nonsurgical control subjects. HRV power spectral analysis parameters were measured (and natural log-transformed) before ISBPB and after changing to the sitting position. The patients experiencing HBEs were assigned to the HBE group, and the remaining patients were assigned to the non-HBE group.
Results
HBEs developed in 18 patients (28.1 %). Changing from the supine position to the sitting position after ISBPB did not induce a significant increase in the natural log-transformed ratio of low-frequency to high-frequency power (lnLF/HF). A significant decrease in natural log-transformed high-frequency power (lnHF) was observed compared to the control group, who presented a significant increase in lnLF/HF and an insignificant change in lnHF. lnHF was found to be significantly higher in the HBE group compared to the non-HBE group.
Conclusions
Sustained vagal activity with a failed shift in the sympathovagal balance toward sympathetic predominance in response to sitting after ISBPB is associated with the development of HBE.


Similar content being viewed by others
References
Ward ME (1974) The interscalene approach to the brachial plexus. Anaesthesia 29:147–157
Seo KC, Park JS, Roh WS (2010) Factors contributing to episodes of bradycardia hypotension during shoulder arthroscopic surgery in the sitting position after interscalene block. Korean J Anesthesiol 58:38–44. doi:10.4097/kjae.2010.58.1.38
D’Alessio JG, Weller RS, Rosenblum M (1995) Activation of the bezold-jarisch reflex in the sitting position for shoulder arthroscopy using interscalene block. Anesth Analg 80:1158–1162
Kahn RL, Hargett MJ (1999) Beta-adrenergic blockers and vasovagal episodes during shoulder surgery in the sitting position under interscalene block. Anesth Analg 88:378–381
Liguori GA, Kahn RL, Gordon J, Gordon MA, Urban MK (1998) The use of metoprolol and glycopyrrolate to prevent hypotensive/bradycardic events during shoulder arthroscopy in the sitting position under interscalene block. Anesth Analg 87:1320–1325
Sia S, Sarro F, Lepri A, Bartoli M (2003) The effect of exogenous epinephrine on the incidence of hypotensive/bradycardic events during shoulder surgery in the sitting position during interscalene block. Anesth Analg 97:583–588
Song SY, Son SH, Kim SO, Roh WS (2011) Intravenous fentanyl during shoulder arthroscopic surgery in the sitting position after interscalene block increases the incidence of episodes of bradycardia hypotension. Korean J Anesthesiol 60:344–350. doi:10.4097/kjae.2011.60.5.344
Frassanito L, Flore V, Messina A, Bronzo V, Gilardi E, Vergari A (2011) Effects of interscalene brachial plexus block on heart rate variability. Eur J Anaesthesiol 28(Supple 48):117
Simeoforidou M, Vretzakis G, Chantzi E, Bareka M, Tsiaka K, Iatrou C, Karachalios T (2013) Effect of interscalene brachial plexus block on heart rate variability. Korean J Anesthesiol 64:432–438. doi:10.4097/kjae.2013.64.5.432
Piccirillo G, Naso C, Moise A, Lionetti M, Nocco M, Di Carlo S, De Laurentis T, Magri D, Cacciafesta M, Marigliano V (2004) Heart rate and blood pressure variability in subjects with vasovagal syncope. Clin Sci (Lond) 107:55–61. doi:10.1042/CS20030327
Lagi A, Tamburini C, Cipriani M, Fattorini L (1997) Vagal control of heart rate variability in vasovagal syncope: studies based on 24-h electrocardiogram recordings. Clin Auton Res 7:127–130
Lagi A, Tamburini C, Fattorini L, Cencetti S (1999) Autonomic control of heart rate variability in vasovagal syncope: a study of the nighttime period in 24-hour recordings. Clin Auton Res 9:179–183
Baharav A, Mimouni M, Lehrman-Sagie T, Izraeli S, Akselrod S (1993) Spectral analysis of heart rate in vasovagal syncope: the autonomic nervous system in vasovagal syncope. Clin Auton Res 3:261–269
Winnie AP (1970) Interscalene brachial plexus block. Anesth Analg 49:455–466
Kapral S, Krafft P, Eibenberger K, Fitzgerald R, Gosch M, Weinstabl C (1994) Ultrasound-guided supraclavicular approach for regional anesthesia of the brachial plexus. Anesth Analg 78:507–513
Fouad FM, Tarazi RC, Ferrario CM, Fighaly S, Alicandri C (1984) Assessment of parasympathetic control of heart rate by a noninvasive method. Am J Physiol 246:H838–H842
Koizumi K, Terui N, Kollai M (1985) Effect of cardiac vagal and sympathetic nerve activity on heart rate in rhythmic fluctuations. J Auton Nerv Syst 12:251–259
Rahman F, Pechnik S, Gross D, Sewell L, Goldstein DS (2011) Low frequency power of heart rate variability reflects baroreflex function, not cardiac sympathetic innervation. Clin Auton Res 21:133–141. doi:10.1007/s10286-010-0098-y
Pagani M, Lombardi F, Guzzetti S, Rimoldi O, Furlan R, Pizzinelli P, Sandrone G, Malfatto G, Dell’Orto S, Piccaluga E (1986) Power spectral analysis of heart rate and arterial pressure variabilities as a marker of sympatho-vagal interaction in man and conscious dog. Circ Res 59:178–193
Vybiral T, Bryg RJ, Maddens ME, Boden WE (1989) Effect of passive tilt on sympathetic and parasympathetic components of heart rate variability in normal subjects. Am J Cardiol 63:1117–1120
Montano N, Ruscone TG, Porta A, Lombardi F, Pagani M, Malliani A (1994) Power spectrum analysis of heart rate variability to assess the changes in sympathovagal balance during graded orthostatic tilt. Circulation 90:1826–1831
Bloomfield DM, Kaufman ES, Bigger JT Jr, Fleiss J, Rolnitzky L, Steinman R (1997) Passive head-up tilt and actively standing up produce similar overall changes in autonomic balance. Am Heart J 134:316–320. doi:10.1016/S0002-8703(97)70140-6
Kinsella SM, Tuckey JP (2001) Perioperative bradycardia and asystole: relationship to vasovagal syncope and the bezold-jarisch reflex. Br J Anaesth 86:859–868
Cacioppo JT, Berntson GG, Binkley PF, Quigley KS, Uchino BN, Fieldstone A (1994) Autonomic cardiac control. II. Noninvasive indices and basal response as revealed by autonomic blockades. Psychophysiology 31:586–598
Song SY, Roh WS (2012) Hypotensive bradycardic events during shoulder arthroscopic surgery under interscalene brachial plexus blocks. Korean J Anesthesiol 62:209–219. doi:10.4097/kjae.2012.62.3.209
Morillo CA, Klein GJ, Jones DL, Yee R (1994) Time and frequency domain analyses of heart rate variability during orthostatic stress in patients with neurally mediated syncope. Am J Cardiol 74:1258–1262
Billman GE (2013) The LF/HF ratio does not accurately measure cardiac sympatho-vagal balance. Front Physiol 4:26. doi:10.3389/fphys.2013.00026
Romme J, Reitsma JB, Black CN, Colman N, Scholten R, Wieling W, Van Dijk N (2011) Drugs and pacemakers for vasovagal, carotid sinus and situational syncope. Cochrane Database Syst Rev. doi:10.1002/14651858.CD004194.pub3
Acknowledgments
This work was supported by a Grant from the Research Institute of Medical Science, Catholic University of Daegu (2013).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Rights and permissions
About this article
Cite this article
Kim, J.H., Song, S.Y., Ryu, T. et al. Changes in heart rate variability after sitting following interscalene block. Clin Auton Res 25, 327–333 (2015). https://doi.org/10.1007/s10286-015-0312-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10286-015-0312-z