Abstract
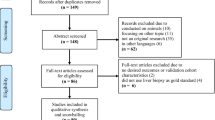
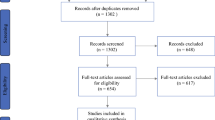
Due to the increasing interest in the use of artificial intelligence (AI) algorithms in hepatocellular carcinoma detection, we performed a systematic review and meta-analysis to pool the data on diagnostic performance metrics of AI and to compare them with clinicians’ performance. A search in PubMed and Scopus was performed in January 2024 to find studies that evaluated and/or validated an AI algorithm for the detection of HCC. We performed a meta-analysis to pool the data on the metrics of diagnostic performance. Subgroup analysis based on the modality of imaging and meta-regression based on multiple parameters were performed to find potential sources of heterogeneity. The risk of bias was assessed using Multivariable Prediction Model for Individual Prognosis or Diagnosis (TRIPOD) and Prediction Model Study Risk of Bias Assessment Tool (PROBAST) reporting guidelines. Out of 3177 studies screened, 44 eligible studies were included. The pooled sensitivity and specificity for internally validated AI algorithms were 84% (95% CI: 81,87) and 92% (95% CI: 90,94), respectively. Externally validated AI algorithms had a pooled sensitivity of 85% (95% CI: 78,89) and specificity of 84% (95% CI: 72,91). When clinicians were internally validated, their pooled sensitivity was 70% (95% CI: 60,78), while their pooled specificity was 85% (95% CI: 77,90). This study implies that AI can perform as a diagnostic supplement for clinicians and radiologists by screening images and highlighting regions of interest, thus improving workflow.





Similar content being viewed by others
Data Availability
The data that support the findings of this study are available from the authors upon reasonable request.
References
Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J Clin. 2021;71(3):209-49.
Ferlay J, Colombet M, Soerjomataram I, Mathers C, Parkin DM, Pineros M, et al. Estimating the global cancer incidence and mortality in 2018: GLOBOCAN sources and methods. Int J Cancer. 2019;144(8):1941-53.
McGlynn KA, Petrick JL, London WT. Global epidemiology of hepatocellular carcinoma: an emphasis on demographic and regional variability. Clin Liver Dis. 2015;19(2):223-38.
Vogel A, Meyer T, Sapisochin G, Salem R, Saborowski A. Hepatocellular carcinoma. Lancet. 2022;400(10360):1345-62.
Ding J, Wen Z. Survival improvement and prognosis for hepatocellular carcinoma: analysis of the SEER database. BMC Cancer. 2021;21(1):1157.
Njei B, Rotman Y, Ditah I, Lim JK. Emerging trends in hepatocellular carcinoma incidence and mortality. Hepatology. 2015;61(1):191-9.
Mittal S, Kanwal F, Ying J, Chung R, Sada YH, Temple S, et al. Effectiveness of surveillance for hepatocellular carcinoma in clinical practice: A United States cohort. J Hepatol. 2016;65(6):1148-54.
Collier J, Sherman M. Screening for hepatocellular carcinoma. Hepatology. 1998;27(1):273-8.
Liang Y, Xu F, Guo Y, Lai L, Jiang X, Wei X, et al. Diagnostic performance of LI-RADS for MRI and CT detection of HCC: A systematic review and diagnostic meta-analysis. Eur J Radiol. 2021;134:109404.
Kuo RYL, Harrison C, Curran TA, Jones B, Freethy A, Cussons D, et al. Artificial Intelligence in Fracture Detection: A Systematic Review and Meta-Analysis. Radiology. 2022;304(1):50-62.
Han SH, Kim KW, Kim S, Youn YC. Artificial Neural Network: Understanding the Basic Concepts without Mathematics. Dement Neurocogn Disord. 2018;17(3):83-9.
IBM. What is deep learning? [Available from: https://tinyurl.com/2p8drtfk.
Richardson ML, Garwood ER, Lee Y, Li MD, Lo HS, Nagaraju A, et al. Noninterpretive Uses of Artificial Intelligence in Radiology. Acad Radiol. 2021;28(9):1225-35.
Goldberg JE, Rosenkrantz AB. Artificial Intelligence and Radiology: A Social Media Perspective. Curr Probl Diagn Radiol. 2019;48(4):308-11.
Baltzer PA, Dietzel M, Kaiser WA. A simple and robust classification tree for differentiation between benign and malignant lesions in MR-mammography. Eur Radiol. 2013;23(8):2051-60.
Zsoter N, Bandi P, Szabo G, Toth Z, Bundschuh RA, Dinges J, et al. PET-CT based automated lung nodule detection. Annu Int Conf IEEE Eng Med Biol Soc. 2012;2012:4974-7.
Huang W, Tan ZM, Lin Z, Huang GB, Zhou J, Chui CK, et al. A semi-automatic approach to the segmentation of liver parenchyma from 3D CT images with Extreme Learning Machine. Annu Int Conf IEEE Eng Med Biol Soc. 2012;2012:3752-5.
Mewes A, Hensen B, Wacker F, Hansen C. Touchless interaction with software in interventional radiology and surgery: a systematic literature review. Int J Comput Assist Radiol Surg. 2017;12(2):291-305.
Mitrea D, Badea R, Mitrea P, Brad S, Nedevschi S. Hepatocellular Carcinoma Automatic Diagnosis within CEUS and B-Mode Ultrasound Images Using Advanced Machine Learning Methods. Sensors (Basel). 2021;21(6).
Ding Y, Ruan S, Wang Y, Shao J, Sun R, Tian W, et al. Novel deep learning radiomics model for preoperative evaluation of hepatocellular carcinoma differentiation based on computed tomography data. Clin Transl Med. 2021;11(11):e570.
Administration TUFaD. Artificial Intelligence and Machine Learning (AI/ML)-Enabled Medical Devices fda.gov2022 [Available from: shorturl.at/lmX29.
Sanmarchi F, Fanconi C, Golinelli D, Gori D, Hernandez-Boussard T, Capodici A. Predict, diagnose, and treat chronic kidney disease with machine learning: a systematic literature review. J Nephrol. 2023.
Ghozy S, Azzam AY, Kallmes KM, Matsoukas S, Fifi JT, Luijten SPR, et al. The diagnostic performance of artificial intelligence algorithms for identifying M2 segment middle cerebral artery occlusions: A systematic review and meta-analysis. J Neuroradiol. 2023.
Widaatalla Y, Wolswijk T, Adan F, Hillen LM, Woodruff HC, Halilaj I, et al. The application of artificial intelligence in the detection of basal cell carcinoma: A systematic review. J Eur Acad Dermatol Venereol. 2023.
Almasan O, Leucuta DC, Hedesiu M, Muresanu S, Popa SL. Temporomandibular Joint Osteoarthritis Diagnosis Employing Artificial Intelligence: Systematic Review and Meta-Analysis. J Clin Med. 2023;12(3).
Patil S, Albogami S, Hosmani J, Mujoo S, Kamil MA, Mansour MA, et al. Artificial Intelligence in the Diagnosis of Oral Diseases: Applications and Pitfalls. Diagnostics (Basel). 2022;12(5).
Krittanawong C, Johnson KW, Rosenson RS, Wang Z, Aydar M, Baber U, et al. Deep learning for cardiovascular medicine: a practical primer. Eur Heart J. 2019;40(25):2058-73.
Thrall JH, Li X, Li Q, Cruz C, Do S, Dreyer K, et al. Artificial Intelligence and Machine Learning in Radiology: Opportunities, Challenges, Pitfalls, and Criteria for Success. J Am Coll Radiol. 2018;15(3 Pt B):504–8.
Higgins JPT TJ, Chandler J, Cumpston M, Li T, Page MJ, Welch VA (editors). Cochrane Handbook for Systematic Reviews of Interventions version 6.3 (updated February 2022). Cochrane, 2022.
Dwamena B. MIDAS: Stata module for meta-analytical integration of diagnostic test accuracy studies. 2009.
Harbord RM, Whiting P. Metandi: meta-analysis of diagnostic accuracy using hierarchical logistic regression. The Stata Journal. 2009;9(2):211-29.
Collins GS, Reitsma JB, Altman DG, Moons KG. Transparent reporting of a multivariable prediction model for individual prognosis or diagnosis (TRIPOD): the TRIPOD Statement. BMC Med. 2015;13:1.
Wolff RF, Moons KGM, Riley RD, Whiting PF, Westwood M, Collins GS, et al. PROBAST: A Tool to Assess the Risk of Bias and Applicability of Prediction Model Studies. Ann Intern Med. 2019;170(1):51-8.
Deeks JJ, Macaskill P, Irwig L. The performance of tests of publication bias and other sample size effects in systematic reviews of diagnostic test accuracy was assessed. J Clin Epidemiol. 2005;58(9):882-93.
Shiraishi J, Sugimoto K, Moriyasu F, Kamiyama N, Doi K. Computer-aided diagnosis for the classification of focal liver lesions by use of contrast-enhanced ultrasonography. Medical Physics. 2008;35(5):1734–46.
Sugimoto K, Shiraishi J, Moriyasu F, Doi K. Computer-aided Diagnosis of Focal Liver Lesions by Use of Physicians' Subjective Classification of Echogenic Patterns in Baseline and Contrast-enhanced Ultrasonography. Academic Radiology. 2009;16(4):401–11.
Mittal D, Kumar V, Saxena SC, Khandelwal N, Kalra N. Neural network based focal liver lesion diagnosis using ultrasound images. Computerized Medical Imaging and Graphics. 2011;35(4):315-23.
Streba CT, Ionescu M, Gheonea DI, Sandulescu L, Ciurea T, Saftoiu A, et al. Contrast-enhanced ultrasonography parameters in neural network diagnosis of liver tumors. World Journal of Gastroenterology. 2012;18(32):4427-34.
Virmani J, Kumar V, Kalra N, Khandelwal N. Neural network ensemble based CAD system for focal liver lesions from B-mode ultrasound. Journal of Digital Imaging. 2014;27(4):520-37.
Yamakawa M, Shiina T, Nishida N, Kudo M, editors. Computer aided diagnosis system developed for ultrasound diagnosis of liver lesions using deep learning. IEEE International Ultrasonics Symposium, IUS; 2019.
Brehar R, Mitrea DA, Vancea F, Marita T, Nedevschi S, Lupsor-Platon M, et al. Comparison of Deep-Learning and Conventional Machine-Learning Methods for the Automatic Recognition of the Hepatocellular Carcinoma Areas from Ultrasound Images. Sensors (Basel). 2020;20(11).
Huang Q, Pan F, Li W, Yuan F, Hu H, Huang J, et al. Differential Diagnosis of Atypical Hepatocellular Carcinoma in Contrast-Enhanced Ultrasound Using Spatiooral Diagnostic Semantics. IEEE Journal of Biomedical and Health Informatics. 2020;24(10):2860-9.
Ren S, Li Q, Liu S, Qi Q, Duan S, Mao B, et al. Clinical Value of Machine Learning-Based Ultrasomics in Preoperative Differentiation Between Hepatocellular Carcinoma and Intrahepatic Cholangiocarcinoma: A Multicenter Study. Frontiers in Oncology. 2021;11.
Tiyarattanachai T, Apiparakoon T, Marukatat S, Sukcharoen S, Geratikornsupuk N, Anukulkarnkusol N, et al. Development and validation of artificial intelligence to detect and diagnose liver lesions from ultrasound images. PLoS ONE. 2021;16(6 June).
Ryu H, Shin SY, Lee JY, Lee KM, Kang HJ, Yi J. Joint segmentation and classification of hepatic lesions in ultrasound images using deep learning. European Radiology. 2021;31(11):8733-42.
Nishida N, Yamakawa M, Shiina T, Mekada Y, Nishida M, Sakamoto N, et al. Artificial intelligence (AI) models for the ultrasonographic diagnosis of liver tumors and comparison of diagnostic accuracies between AI and human experts. Journal of Gastroenterology. 2022;57(4):309-21.
Zhang WB, Hou SZ, Chen YL, Mao F, Dong Y, Chen JG, et al. Deep Learning for Approaching Hepatocellular Carcinoma Ultrasound Screening Dilemma: Identification of α-Fetoprotein-Negative Hepatocellular Carcinoma From Focal Liver Lesion Found in High-Risk Patients. Frontiers in Oncology. 2022;12.
Tangruangkiat S, Chaiwongkot N, Pamarapa C, Rawangwong T, Khunnarong A, Chainarong C, et al. Diagnosis of focal liver lesions from ultrasound images using a pretrained residual neural network. J Appl Clin Med Phys. 2024;25(1):e14210.
Urhut MC, Sandulescu LD, Streba CT, Mamuleanu M, Ciocalteu A, Cazacu SM, et al. Diagnostic Performance of an Artificial Intelligence Model Based on Contrast-Enhanced Ultrasound in Patients with Liver Lesions: A Comparative Study with Clinicians. Diagnostics (Basel). 2023;13(21).
Azimi Nanvaee F, Setayeshi S. Hepatocellular Carcinoma Diagnosis Based on Ultrasound Images Using Feature Selection Techniques and K-nearest Neighbor Classifier. Hepat Mon. 2023;23(1):e136213.
Chen EL, Chung PC, Chen CL, Tsai HM, Chang CI. An automatic diagnostic system for CT liver image classification. IEEE Trans Biomed Eng. 1998;45(6):783-94.
Kumar SS, Moni RS. Diagnosis of liver tumour from CT images using contourlet transform. International Journal of Biomedical Engineering and Technology. 2011;7(3):276-90.
Das A, Das P, Panda SS, Sabut S. Adaptive fuzzy clustering-based texture analysis for classifying liver cancer in abdominal CT images. International Journal of Computational Biology and Drug Design. 2018;11(3):192-208.
Nayak A, Baidya Kayal E, Arya M, Culli J, Krishan S, Agarwal S, et al. Computer-aided diagnosis of cirrhosis and hepatocellular carcinoma using multi-phase abdomen CT. International Journal of Computer Assisted Radiology and Surgery. 2019;14(8):1341-52.
Cao SE, Zhang LQ, Kuang SC, Shi WQ, Hu B, Xie SD, et al. Multiphase convolutional dense network for the classification of focal liver lesions on dynamic contrast-enhanced computed tomography. World J Gastroenterol. 2020;26(25):3660-72.
Shi W, Kuang S, Cao S, Hu B, Xie S, Chen S, et al. Deep learning assisted differentiation of hepatocellular carcinoma from focal liver lesions: choice of four-phase and three-phase CT imaging protocol. Abdominal Radiology. 2020;45(9):2688-97.
Nakai H, Fujimoto K, Yamashita R, Sato T, Someya Y, Taura K, et al. Convolutional neural network for classifying primary liver cancer based on triple-phase CT and tumor marker information: a pilot study. Japanese Journal of Radiology. 2021;39(7):690-702.
Wang M, Fu F, Zheng B, Bai Y, Wu Q, Wu J, et al. Development of an AI system for accurately diagnose hepatocellular carcinoma from computed tomography imaging data. British Journal of Cancer. 2021;125(8):1111-21.
Hussain M, Saher N, Qadri S. Computer Vision Approach for Liver Tumor Classification Using CT Dataset. Applied Artificial Intelligence. 2022;36(1).
Cheng CT, Cai J, Teng W, Zheng Y, Huang YT, Wang YC, et al. A flexible three-dimensional heterophase computed tomography hepatocellular carcinoma detection algorithm for generalizable and practical screening. Hepatology Communications. 2022.
Anisha A, Jiji G, Ajith Bosco Raj T. Deep feature fusion and optimized feature selection based ensemble classification of liver lesions. The Imaging Science Journal. 2023;71(6):518–36.
Midya A, Chakraborty J, Srouji R, Narayan RR, Boerner T, Zheng J, et al. Computerized Diagnosis of Liver Tumors From CT Scans Using a Deep Neural Network Approach. IEEE J Biomed Health Inform. 2023;27(5):2456-64.
Guo L, Li X, Zhang C, Xu Y, Han L, Zhang L. Radiomics Based on Dynamic Contrast-Enhanced Magnetic Resonance Imaging in Preoperative Differentiation of Combined Hepatocellular-Cholangiocarcinoma from Hepatocellular Carcinoma: A Multi-Center Study. J Hepatocell Carcinoma. 2023;10:795-806.
Zhang X, Jia N, Wang Y. Multi-input dense convolutional network for classification of hepatocellular carcinoma and intrahepatic cholangiocarcinoma. Biomedical Signal Processing and Control. 2023;80:104226.
Ling Y, Ying S, Xu L, Peng Z, Mao X, Chen Z, et al. Automatic volumetric diagnosis of hepatocellular carcinoma based on four-phase CT scans with minimum extra information. Front Oncol. 2022;12:960178.
Zhang X, Kanematsu M, Fujita H, Zhou X, Hara T, Yokoyama R, et al. Application of an artificial neural network to the computer-aided differentiation of focal liver disease in MR imaging. Radiological Physics and Technology. 2009;2(2):175-82.
Gatos I, Tsantis S, Karamesini M, Spiliopoulos S, Karnabatidis D, Hazle JD, et al. Focal liver lesions segmentation and classification in nonenhanced T2-weighted MRI. Medical Physics. 2017;44(7):3695-705.
Jansen MJA, Kuijf HJ, Veldhuis WB, Wessels FJ, Viergever MA, Pluim JPW. Automatic classification of focal liver lesions based on MRI and risk factors. PLoS ONE. 2019;14(5).
Oyama A, Hiraoka Y, Obayashi I, Saikawa Y, Furui S, Shiraishi K, et al. Hepatic tumor classification using texture and topology analysis of non-contrast-enhanced three-dimensional T1-weighted MR images with a radiomics approach. Scientific Reports. 2019;9(1).
Jiang H, Liu X, Chen J, Wei Y, Lee JM, Cao L, et al. Man or machine? Prospective comparison of the version 2018 EASL, LI-RADS criteria and a radiomics model to diagnose hepatocellular carcinoma. Cancer Imaging. 2019;19(1).
Oestmann PM, Wang CJ, Savic LJ, Hamm CA, Stark S, Schobert I, et al. Deep learning–assisted differentiation of pathologically proven atypical and typical hepatocellular carcinoma (HCC) versus non-HCC on contrast-enhanced MRI of the liver. European Radiology. 2021;31(7):4981-90.
Takenaga T, Hanaoka S, Nomura Y, Nakao T, Shibata H, Miki S, et al. Multichannel three-dimensional fully convolutional residual network-based focal liver lesion detection and classification in Gd-EOB-DTPA-enhanced MRI. International Journal of Computer Assisted Radiology and Surgery. 2021;16(9):1527-36.
Wang SH, Han XJ, Du J, Wang ZC, Yuan C, Chen Y, et al. Saliency-based 3D convolutional neural network for categorising common focal liver lesions on multisequence MRI. Insights into Imaging. 2021;12(1).
Zhang H, Guo D, Liu H, He X, Qiao X, Liu X, et al. MRI-Based Radiomics Models to Discriminate Hepatocellular Carcinoma and Non-Hepatocellular Carcinoma in LR-M According to LI-RADS Version 2018. Diagnostics. 2022;12(5).
Fotouhi M, Samadi Khoshe Mehr F, Delazar S, Shahidi R, Setayeshpour B, Toosi MN, et al. Assessment of LI-RADS efficacy in classification of hepatocellular carcinoma and benign liver nodules using DCE-MRI features and machine learning. Eur J Radiol Open. 2023;11:100535.
Park S, Byun J, Hwang SM. Utilization of a Machine Learning Algorithm for the Application of Ancillary Features to LI-RADS Categories LR3 and LR4 on Gadoxetate Disodium-Enhanced MRI. Cancers (Basel). 2023;15(5).
Naeem S, Ali A, Qadri S, Mashwani WK, Tairan N, Shah H, et al. Machine-learning based hybrid-feature analysis for liver cancer classification using fused (MR and CT) images. Applied Sciences (Switzerland). 2020;10(9).
Murugesan S, Bhuvaneswaran RS, Khanna Nehemiah H, Keerthana Sankari S, Nancy Jane Y. Feature Selection and Classification of Clinical Datasets Using Bioinspired Algorithms and Super Learner. Computational and Mathematical Methods in Medicine. 2021;2021.
Kim J, Min JH, Kim SK, Shin SY, Lee MW. Detection of Hepatocellular Carcinoma in Contrast-Enhanced Magnetic Resonance Imaging Using Deep Learning Classifier: A Multi-Center Retrospective Study. Scientific Reports. 2020;10(1).
Tiyarattanachai T, Apiparakoon T, Marukatat S, Sukcharoen S, Geratikornsupuk N, Anukulkarnkusol N, et al. Development and validation of artificial intelligence to detect and diagnose liver lesions from ultrasound images. PLoS One. 2021;16(6):e0252882.
Ren S, Li Q, Liu S, Qi Q, Duan S, Mao B, et al. Clinical Value of Machine Learning-Based Ultrasomics in Preoperative Differentiation Between Hepatocellular Carcinoma and Intrahepatic Cholangiocarcinoma: A Multicenter Study. Front Oncol. 2021;11:749137.
Bleeker SE, Moll HA, Steyerberg EW, Donders AR, Derksen-Lubsen G, Grobbee DE, et al. External validation is necessary in prediction research: a clinical example. J Clin Epidemiol. 2003;56(9):826-32.
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics Approval
Not applicable.
Competing Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Salehi, M.A., Harandi, H., Mohammadi, S. et al. Diagnostic Performance of Artificial Intelligence in Detection of Hepatocellular Carcinoma: A Meta-analysis. J Digit Imaging. Inform. med. (2024). https://doi.org/10.1007/s10278-024-01058-1
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10278-024-01058-1