Abstract
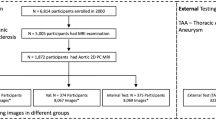
Feasibility assessment and planning of thoracic endovascular aortic repair (TEVAR) require computed tomography (CT)-based analysis of geometric aortic features to identify adequate landing zones (LZs) for endograft deployment. However, no consensus exists on how to take the necessary measurements from CT image data. We trained and applied a fully automated pipeline embedding a convolutional neural network (CNN), which feeds on 3D CT images to automatically segment the thoracic aorta, detects proximal landing zones (PLZs), and quantifies geometric features that are relevant for TEVAR planning. For 465 CT scans, the thoracic aorta and pulmonary arteries were manually segmented; 395 randomly selected scans with the corresponding ground truth segmentations were used to train a CNN with a 3D U-Net architecture. The remaining 70 scans were used for testing. The trained CNN was embedded within computational geometry processing pipeline which provides aortic metrics of interest for TEVAR planning. The resulting metrics included aortic arch centerline radius of curvature, proximal landing zones (PLZs) maximum diameters, angulation, and tortuosity. These parameters were statistically analyzed to compare standard arches vs. arches with a common origin of the innominate and left carotid artery (CILCA). The trained CNN yielded a mean Dice score of 0.95 and was able to generalize to 9 pathological cases of thoracic aortic aneurysm, providing accurate segmentations. CILCA arches were characterized by significantly greater angulation (p = 0.015) and tortuosity (p = 0.048) in PLZ 3 vs. standard arches. For both arch configurations, comparisons among PLZs revealed statistically significant differences in maximum zone diameters (p < 0.0001), angulation (p < 0.0001), and tortuosity (p < 0.0001). Our tool allows clinicians to obtain objective and repeatable PLZs mapping, and a range of automatically derived complex aortic metrics.






Similar content being viewed by others
References
Rimbau V, Böckler D, Brunkwall J. Management of descending thoracic aorta diseases. Clinical practice guidelines of the European Society for Vascular Surgery (ESVS). Eur J Vasc Endovasc Surg. 2017;53:4–52.
Bellamkonda KS, Yousef S, Nassiri N, Dardik A, Guzman RJ, Geirsson A, et al. Trends and outcomes of thoracic endovascular aortic repair with open concomitant cervical debranching. Journal of Vascular Surgery. 2021;73(4):1205–12. e3.
Marrocco-Trischitta MM, de Beaufort HW, Piffaretti G, Bonardelli S, Gargiulo M, Antonello M, et al. The Modified Arch Landing Areas Nomenclature predicts proximal endograft failure after thoracic endovascular aortic repair. European Journal of Cardio-Thoracic Surgery. 2020;58(2):309-18.
Figueroa CA, Taylor CA, Chiou AJ, Yeh V, Zarins CK. Magnitude and direction of pulsatile displacement forces acting on thoracic aortic endografts. Journal of Endovascular Therapy. 2009;16(3):350-8.
members ATF, Erbel R, Aboyans V, Boileau C, Bossone E, Bartolomeo RD, et al. 2014 ESC Guidelines on the diagnosis and treatment of aortic diseases: document covering acute and chronic aortic diseases of the thoracic and abdominal aorta of the adult The Task Force for the Diagnosis and Treatment of Aortic Diseases of the European Society of Cardiology (ESC). European heart journal. 2014;35(41):2873–926.
Grabenwöger M, Alfonso F, Bachet J, Bonser R, Czerny M, Eggebrecht H, et al. Thoracic Endovascular Aortic Repair (TEVAR) for the treatment of aortic diseases: a position statement from the European Association for Cardio-Thoracic Surgery (EACTS) and the European Society of Cardiology (ESC), in collaboration with the European Association of Percutaneous Cardiovascular Interventions (EAPCI). European heart journal. 2012;33(13):1558-63.
Matsumura JS, Cambria RP, Dake MD, Moore RD, Svensson LG, Snyder S, et al. International controlled clinical trial of thoracic endovascular aneurysm repair with the Zenith TX2 endovascular graft: 1-year results. Journal of vascular surgery. 2008;47(2):247–57. e3.
Ishimaru S. Endografting of the aortic arch. Journal of endovascular therapy. 2004;11(6_suppl):II-62-II-71.
Altnji H-E, Bou-Saïd B, Walter-Le Berre H. Morphological and stent design risk factors to prevent migration phenomena for a thoracic aneurysm: a numerical analysis. Medical engineering & physics. 2015;37(1):23-33.
Ueda T, Takaoka H, Raman B, Rosenberg J, Rubin GD. Impact of quantitatively determined native thoracic aortic tortuosity on endoleak development after thoracic endovascular aortic repair. American Journal of Roentgenology. 2011;197(6):W1140-W6.
Marrocco-Trischitta MM, Alaidroos M, Romarowski RM, Milani V, Ambrogi F, Secchi F, et al. Aortic arch variant with a common origin of the innominate and left carotid artery as a determinant of thoracic aortic disease: a systematic review and meta-analysis. European Journal of Cardio-Thoracic Surgery. 2020;57(3):422-7.
Mylonas SN, Barkans A, Ante M, Wippermann J, Böckler D, Brunkwall JS. Prevalence of bovine aortic arch variant in patients with aortic dissection and its implications in the outcome of patients with acute type B aortic dissection. European Journal of Vascular and Endovascular Surgery. 2018;55(3):385-91.
Marrocco-Trischitta MM, Alaidroos M, Romarowski RM, Secchi F, Righini P, Glauber M, et al. Geometric pattern of proximal landing zones for thoracic endovascular aortic repair in the bovine arch variant. European Journal of Vascular and Endovascular Surgery. 2020;59(5):808-16.
Marrocco-Trischitta MM, Romarowski RM, Alaidroos M, Sturla F, Glauber M, Nano G. Computational Fluid Dynamics Modeling of Proximal Landing Zones for Thoracic Endovascular Aortic Repair in the Bovine Arch Variant. Annals of Vascular Surgery. 2020;69:413-7.
Marrocco-Trischitta MM, de Beaufort HW, Secchi F, van Bakel TM, Ranucci M, Van Herwaarden JA, et al. A geometric reappraisal of proximal landing zones for thoracic endovascular aortic repair according to aortic arch types. Journal of vascular surgery. 2017;65(6):1584-90.
Parodi J, Berguer R, Carrascosa P, Khanafer K, Capunay C, Wizauer E. Sources of error in the measurement of aortic diameter in computed tomography scans. Journal of vascular surgery. 2014;59(1):74-9.
Litjens G, Kooi T, Bejnordi BE, Setio AAA, Ciompi F, Ghafoorian M, et al. A survey on deep learning in medical image analysis. Medical image analysis. 2017;42:60-88.
Bakas S, Reyes M, Jakab A, Bauer S, Rempfler M, Crimi A, et al. Identifying the best machine learning algorithms for brain tumor segmentation, progression assessment, and overall survival prediction in the BRATS challenge. arXiv preprint arXiv:181102629. 2018.
Tobon-Gomez C, Geers AJ, Peters J, Weese J, Pinto K, Karim R, et al. Benchmark for algorithms segmenting the left atrium from 3D CT and MRI datasets. IEEE transactions on medical imaging. 2015;34(7):1460-73.
Bilic P, Christ PF, Vorontsov E, Chlebus G, Chen H, Dou Q, et al. The liver tumor segmentation benchmark (lits). arXiv preprint arXiv:190104056. 2019.
Simpson AL, Antonelli M, Bakas S, Bilello M, Farahani K, Van Ginneken B, et al. A large annotated medical image dataset for the development and evaluation of segmentation algorithms. arXiv preprint arXiv:190209063. 2019.
Yushkevich PA, Gerig G. ITK-SNAP: an intractive medical image segmentation tool to meet the need for expert-guided segmentation of complex medical images. IEEE pulse. 2017;8(4):54-7.
Kikinis R, Pieper SD, Vosburgh KG. 3D Slicer: a platform for subject-specific image analysis, visualization, and clinical support. Intraoperative imaging and image-guided therapy: Springer; 2014. p. 277-89.
Shen D, Liu T, Peters TM, Staib LH, Essert C, Zhou S, et al. Medical Image Computing and Computer Assisted Intervention–MICCAI 2019: 22nd International Conference, Shenzhen, China, October 13–17, 2019, Proceedings, Part IV: Springer Nature; 2019.
Isensee F, Petersen J, Klein A, Zimmerer D, Jaeger PF, Kohl S, et al. nnu-net: Self-adapting framework for u-net-based medical image segmentation. arXiv preprint arXiv:180910486. 2018.
Berman M, Triki AR, Blaschko MB, editors. The lovász-softmax loss: A tractable surrogate for the optimization of the intersection-over-union measure in neural networks. Proceedings of the IEEE Conference on Computer Vision and Pattern Recognition; 2018.
Lin T-Y, Goyal P, Girshick R, He K, Dollár P, editors. Focal loss for dense object detection. Proceedings of the IEEE international conference on computer vision; 2017.
Lorensen WE, Cline HE. Marching cubes: A high resolution 3D surface construction algorithm. ACM siggraph computer graphics. 1987;21(4):163-9.
Antiga L, Steinman DA. Robust and objective decomposition and mapping of bifurcating vessels. IEEE transactions on medical imaging. 2004;23(6):704-13.
Izzo R, Steinman D, Manini S, Antiga L. The vascular modeling toolkit: a Python library for the analysis of tubular structures in medical images. Journal of Open Source Software. 2018;3(25):745.
Reuter M, Wolter F-E, Peinecke N. Laplace–Beltrami spectra as ‘Shape-DNA’of surfaces and solids. Computer-Aided Design. 2006;38(4):342-66.
Lévy B, Zhang H. Spectral mesh processing. ACM SIGGRAPH 2010 Courses2010. p. 1–312.
Bône A, Louis M, Martin B, Durrleman S, editors. Deformetrica 4: an open-source software for statistical shape analysis. International Workshop on Shape in Medical Imaging; 2018: Springer.
Sun J, Ovsjanikov M, Guibas L, editors. A concise and provably informative multi‐scale signature based on heat diffusion. Computer graphics forum; 2009: Wiley Online Library.
Cormen TH, Leiserson CE, Rivest RL, Stein C. Introduction to algorithms: MIT press; 2009.
Huttenlocher DP, Klanderman GA, Rucklidge WJ. Comparing images using the Hausdorff distance. IEEE Transactions on pattern analysis and machine intelligence. 1993;15(9):850-63.
Noothout JM, De Vos BD, Wolterink JM, Išgum I, editors. Automatic segmentation of thoracic aorta segments in low-dose chest CT. Medical Imaging 2018: Image Processing; 2018: International Society for Optics and Photonics.
Fantazzini A, Esposito M, Finotello A, Auricchio F, Pane B, Basso C, et al. 3D Automatic Segmentation Of Aortic Computed Tomography Angiography Combining Multi-View 2D Convolutional Neural Networks. Cardiovascular engineering and technology. 2020;11(5):576-86.
Kumar SP, Latte MV, Siri SK. Volumetric lung nodule segmentation in thoracic CT scan using freehand sketch. IET Image Processing. 2020;14(14):3456-62.
Malone C, Urbania T, Crook S, Hope M. Bovine aortic arch: a novel association with thoracic aortic dilation. Clinical radiology. 2012;67(1):28-31.
Marrocco-Trischitta MM, Romarowski RM, De Beaufort HW, Conti M, Vitale R, Secchi F, et al. The Modified Arch Landing Areas Nomenclature identifies hostile zones for endograft deployment: a confirmatory biomechanical study in patients treated by thoracic endovascular aortic repair. European Journal of Cardio-Thoracic Surgery. 2019;55(5):990-7.
Funding
“This work was supported by “Ricerca Corrente” and 5xmille” grants from IRCCS Policlinico San Donato, a clinical research hospital partially funded by the Italian Ministry of Health.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics Approval
The study was approved by the Ethics Committee of reference (i.e., Ethics Committee of IRCCS San Raffaele (Milan, Italy). This study does not include any experiments on human participants but consists in a post hoc analysis of medical images. Patients informed consent was waived by the Ethics Committee because of the retrospective nature of the study, and the analysis of anonymized images. The study was conducted according to the principles outlined in the Declaration of Helsinki.
Consent to Participate
Patients informed consent was waived by the Ethics Committee because of the retrospective nature of the study and the analysis of anonymized images. The study was conducted according to the principles outlined in the Declaration of Helsinki.
Consent for Publication
All authors gave their consent for publication.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Massimiliano M. Marrocco-Trischitta and Alberto Redaelli are equally contributing principal investigators.
Rights and permissions
About this article
Cite this article
Saitta, S., Sturla, F., Caimi, A. et al. A Deep Learning-Based and Fully Automated Pipeline for Thoracic Aorta Geometric Analysis and Planning for Endovascular Repair from Computed Tomography. J Digit Imaging 35, 226–239 (2022). https://doi.org/10.1007/s10278-021-00535-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10278-021-00535-1