Abstract
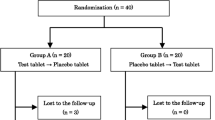
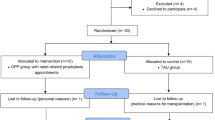
The objectives are to identify volatile sulphur compounds (VSCs) in individuals with Chronic Kidney Disease (CKD) and to relate quality of life and oral health. A case–control study with 32 individuals with CKD in haemodialysis in the study group (SG) and 32 healthy individuals in the control group (CG) was performed. The VSCs were identified by gas chromatograph before (BC) and after cysteine (AC) mouthwash and an organoleptic test. For oral health assessment, oral health index was used. For quality of life, the Oral Health Impact Profile (OHIP-14) and Medical Outcomes Study 36-Item Short Form Health Survery (SF-36) were used. The hydrogen sulphide AC, methyl mercaptan AC, tongue coating, dry mouth, plaque index, and DMFT were significantly higher in the SG. VSCs did not negatively affected the impact of oral health on the quality of life in the SG but did in the CG. As for the impact of general health on quality of life, methyl mercaptan BC and AC worsened overall health in vitality and mental health, respectively. Individuals with CKD have more halitosis than healthy individuals, and it is more related to methyl mercaptan. The halitosis worsened the general quality of life of individuals with CKD. The diagnosis and identification of the origin of halitosis is important to prevent one more factor that it worsened the global quality of life of patients with CKD.
Similar content being viewed by others
References
Aydin M, Harvey-Woodworth CN. Halitosis: a new definition and classification. Br Dent J. 2014;217:E1. https://doi.org/10.1038/sj.bdj.2014.552.
Tangerman A, Winkel EG. Extra-oral halitosis: an overview. J Breath Res. 2010;4:017003. https://doi.org/10.1088/1752-7155/4/1/017003.
Bollen CML, Bleikler T. Halitosis: the multidisciplary approach. Int J Oral Sci. 2012;4:55–63. https://doi.org/10.1038/ijos.2012.39.
van den Broek AM, Feenstra L, de Baat C. A review of the current literature on aetiology and measurement methods of halitosis. J Dent. 2007;35:327–35. https://doi.org/10.1016/j.jdent.2007.04.009.
Gulsahi A, Evirgen S, Öztaş B, et al. Volatile súlfur compunds levels and related factors in patients with chronic renal failure. J Clin Periodontol. 2014;41:814–9. https://doi.org/10.1111/jcpe.
Quirynen M, Zhao H, Avontroodt P, et al. A salivary incubation test for evaluation of oral malodor: a pilot study. J Periodontol. 2003;74:937–44. https://doi.org/10.1902/jop.2003.74.7.937.
Tarzia O. Halitose: um desafio que tem cura. Rio de Janeiro: EPUB; 2003.
World Health Organization (2013). Oral Health Surveys Basic Methods. 5th editon. https://www.who.int/oral_health/publications/9789241548649/en/
Löe H. The Gingival Index, the Plaque Index and the Retention Index Systems. J Periodontol. 1967;38(Suppl):610–6. https://doi.org/10.1902/jop.1967.38.6.610.
Silness J, LöeH H. Periodontal disease in pregnancy II. Correlation between oral hygiene and periodontal condition. Acta Odontol Scand. 1964;22:121–35. https://doi.org/10.3109/00016356408993968.
Winkel EG, Roldán S, Van Winkelhoff AJ, et al. Clinical effects of a new mouthrinse containing chlorhexidine, cetylpyridinium chloride and zinc-lactate on oral halitosis: a dual-center, double-blind placebo-controlled study. J Clin Periodontol. 2003;30:300–6. https://doi.org/10.1034/j.1600-051x.2003.00342.x.
Flink H, Bergdahl M, Tegelberg A, et al. Prevalence of hyposalivation in relation to general health, body mass index and remaining teeth in diferente age groups of adults. Community Dent Oral Epidemiol. 2008;36:523–31. https://doi.org/10.1111/j.1600-0528.2008.00432.x.
Albuquerque DF, de Souza TE, Amado FM, et al. Evaluation of halitosis and sialometry in patients submitted to head and neck radiotherapy. Med Oral Patol Oral Cir Bucal. 2010;15:e850–4. https://doi.org/10.4317/medoral.15.e850.
Kleinberg I, Codipilly D. H(2)S generation and E(h) reduction in cysteine challenge testing as a means of determining the potential of test products and treatments for inhibiting oral malodor. J Breath Res. 2008;2:017018. https://doi.org/10.1088/1752-7155/2/1/017018.
Aimetti M, Perotto S, Castiglione A, et al. Prevalence estimation of halitosis and its association with oral health-related parameters in an adult population of a city in North Italy. J Clin Periodontol. 2015;42:1105–14. https://doi.org/10.1111/jcpe.12474.
Shimura M, Yasuno Y, Iwakura M, et al. A new monitor with a zinc-oxide film semiconductor sensor for the measurement of volatile súlfur compounds in mouth air. J Periodontol. 1996;67:396–402. https://doi.org/10.1902/jop.1996.67.4.396.
Thomson WM. Measuring change in dry-mouth symptoms over time using the Xerostomia Inventory. Gerodontology. 2007;24:30–5. https://doi.org/10.1111/j.1741-2358.2007.00137.x.
Slade GD. Derivation and validation of a short-form oral health impact profile. Community Dent Oral Epidemiol. 1997;25:284–90. https://doi.org/10.1111/j.1600-0528.1997.tb00941.x.
Oliveira BH, Nadanovky P. Psychometric properties of the Brazilian version of the Oral Health Impact Profile-short form. Community Dent Oral Epidemiol. 2005;33:307–14. https://doi.org/10.1111/j.1600-0528.2005.00225.x.
Ware JE Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30:473–83.
Ciconelli RM, Ferraz MB, Santos W, et al. Brazilian-Portuguese version of the SF-36. A reliable and valid quality of life outcome measure. Rev Bras Reumatol. 1999;39:143–50.
Talebian A, Tazhibi M, Iranpoor R, et al. Relationship between tonsil odor and oral malodor: a clinical study on 48 Iranian patients. J Breath Res. 2008;2:017016. https://doi.org/10.1088/1752-7155/2/1/017016.
Vandekerckhove B, Van den Velde S, De Smit M, et al. Clinical reliability of non-organoleptic oral malodour measurements. J Clin Periodontol. 2009;36:964–9. https://doi.org/10.1111/j.1600-051X.2009.01473.x.
Oyetola EO, Owotade FJ, Agbelusi GA, et al. Salivary flow rates of Nigerian patients with chronic kidney disease: a case-control study. J Contemp Dent Pract. 2015;16:264–9. https://doi.org/10.5005/jp-journals-10024-1673.
López-Pintor RM, López-Pintor L, Casañas E, et al. Risk factors associated with xerostomia in haemodialysis patients. Med Oral Patol Oral Cir Bucal. 2017;22:e185–92. https://doi.org/10.4317/medoral.21612.
Hajian-Tilaki A, Oliae F, Jenabian N, et al. Oral health-related quality of life and periodontal and dental health status in Iranian hemodialysis patients. J Contemp Dent Pract. 2014;15:482–90. https://doi.org/10.5005/jp-journals-10024-1566.
Lu HX, Chen XL, Wong M, et al. Oral health impact of halitosis in Chinese adults. Int J Dent Hyg. 2017;15:e85–92. https://doi.org/10.1111/idh.12242.
Kizhner V, Xu D, Krespi YP. A new tool measuring oral malodor quality of life. Eur Arch Otorhinolaryngol. 2011;268:1227–32. https://doi.org/10.1007/s00405-011-1518-x.
Durham J, Fraser HM, McCracken GI, et al. Impact of periodontitis on oral health-related quality of life. J Dent. 2013;41:370–6. https://doi.org/10.1016/j.jdent.2013.01.008.
Acknowledgements
We thank the nephrologist Tricya Nunes Vieira Bueloni for her encouragement and availability in this research
Funding
This study was financed by the Coordination for the improvement of Higher Education Personnel-Brasil (CAPES)-Finance Code 001.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Author Natalia Garcia Santaella declares that she has conflict of interest. Author Guilherme Simpione declares that he has conflict of interest. Author Aloizio Premoli Maciel declares that he has conflict of interest. Author José Roberto Lauris declares that he has conflict of interest. Author Paulo Sérgio da Silva Santos declares that he has conflict of interest. The entity with whom they have such a relationship and the nature of them potential conflict is: Odomed.
Ethical approval
All procedures performed in the participants were in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. This research was approved by the Research Ethics Committee under CAEE 71651517.9.000.5417.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Santaella, N.G., Simpione, G., Maciel, A.P. et al. Volatile sulphur compounds in people with chronic kidney disease and the impact on quality of life. Odontology 109, 561–567 (2021). https://doi.org/10.1007/s10266-020-00576-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10266-020-00576-y