Abstract
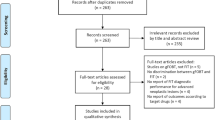
This study aims to investigate the impact of antithrombotic agents and proton-pump inhibitors (PPIs) on fecal immunochemical test (FIT). PubMed, EMBASE, Web of Science, Cochrane Central, and Google Scholar were searched from inception until September 3, 2023. Studies comparing the diagnostic performance of FIT between medicine users and non-users in average-risk colorectal cancer screening populations were included. Pooled sensitivity, specificity, and positive predictive values (PPVs) for advanced neoplasia (AN) of FIT were compared by reporting pooled odds ratios (ORs) with 95% confidence intervals (CIs) using a random-effects model. Twenty-two studies enrolling 5,572,367 individuals were included. For aspirin, pooled sensitivity and specificity for AN were 57.2% and 88.4% in users versus 60.2% and 93.2% in non-users; while pooled ORs were 1.49 (95% CI 0.89–2.48, P = 0.13) and 0.72 (95% CI 0.62–0.83, P < 0.001), respectively. In subgroup analysis, there was no difference in sensitivity and specificity between the two groups at the cutoff of 20 μg Hb/g (P = 0.57 and 0.29, respectively) but a significantly lower specificity in users compared with non-users at lower cutoffs (P < 0.001). Moreover, a significantly lower PPVAN in users compared with non-users was observed after matching age and sex confounders (P = 0.001). Warfarin had no significant influence on PPVAN of FIT (P = 0.43). PPIs were associated with a significantly lower PPVAN in users (P < 0.001). Aspirin use was associated with lower specificity and PPV of FIT. Aspirin discontinuation before FIT to reduce false-positive results should be interpreted with caution given concerns about cardiovascular events. Increasing cutoff values of FIT in aspirin users may be another possible approach. Additionally, warfarin withdrawal before FIT is unnecessary but PPIs withdrawal before FIT is recommended to reduce false-positive results.





Similar content being viewed by others
References
Siegel RL, Miller KD, Fuchs HE, Jemal A. Cancer Statistics, 2021. CA Cancer J Clin. 2021;71:7–33.
Arnold M, Abnet CC, Neale RE, et al. Global burden of 5 major types of gastrointestinal cancer. Gastroenterology. 2020;159:335-49.e15.
Chiu HM, Chen SL, Yen AM, et al. Effectiveness of fecal immunochemical testing in reducing colorectal cancer mortality from the One Million Taiwanese Screening Program. Cancer. 2015;121:3221–9.
Chiu HM, Jen GH, Wang YW, et al. Long-term effectiveness of faecal immunochemical test screening for proximal and distal colorectal cancers. Gut. 2021;70:2321–9.
Zorzi M, Fedeli U, Schievano E, et al. Impact on colorectal cancer mortality of screening programmes based on the faecal immunochemical test. Gut. 2015;64:784–90.
Emile SH, Barsom SH, Wexner SD. An updated review of the methods, guidelines of, and controversies on screening for colorectal cancer. Am J Surg. 2022;224:339–47.
Wolf AMD, Fontham ETH, Church TR, et al. Colorectal cancer screening for average-risk adults: 2018 guideline update from the American Cancer Society. CA Cancer J Clin. 2018;68:250–81.
Abdelaziz HK, Saad M, Pothineni NVK, et al. Aspirin for primary prevention of cardiovascular events. J Am Coll Cardiol. 2019;73:2915–29.
Brenner H, Tao S, Haug U. Low-dose aspirin use and performance of immunochemical fecal occult blood tests. JAMA. 2010;304:2513–20.
Amitay EL, Cuk K, Niedermaier T, Weigl K, Brenner H. Factors associated with false-positive fecal immunochemical tests in a large German colorectal cancer screening study. Int J Cancer. 2019;144:2419–27.
Jung Y, Im E, Lee J, Lee H, Moon C. Use of antiplatelet agents decreases the positive predictive value of fecal immunochemical tests for colorectal cancer but does not affect their sensitivity. J Personal Med. 2021;11:23.
Randel KR, Botteri E, Romstad KMK, et al. Effects of oral anticoagulants and aspirin on performance of fecal immunochemical tests in colorectal cancer screening. Gastroenterology. 2019;156:1642-9.e1.
Chandrapalan S, Hee SW, Widlak MM, et al. Performance of the faecal immunochemical test for the detection of colorectal neoplasms and the role of proton pump inhibitors in their diagnostic accuracy. Colorectal Dis. 2021;23:1649–57.
Rodriguez-Alonso L, Rodriguez-Moranta F, Arajol C, et al. Proton pump inhibitors reduce the accuracy of faecal immunochemical test for detecting advanced colorectal neoplasia in symptomatic patients. PLoS ONE. 2018;13: e0203359.
Gandhi S, Narula N, Gandhi S, Marshall JK, Farkouh ME. Does acetylsalicylic acid or warfarin affect the accuracy of fecal occult blood tests? J Gastroenterol Hepatol. 2013;28:931–6.
Nieuwenburg SAV, Vuik FER, Kruip M, Kuipers EJ, Spaander MCW. Effect of anticoagulants and NSAIDs on accuracy of faecal immunochemical tests (FITs) in colorectal cancer screening: a systematic review and meta-analysis. Gut. 2019;68:866–72.
Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ (Clin Res Ed). 2009;339: b2535.
Wells GA, Bea S. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses; 2009.
Higgins JP, Altman DG, Gøtzsche PC, et al. The Cochrane collaboration’s tool for assessing risk of bias in randomised trials. BMJ (Clin Res Ed). 2011;343: d5928.
Borenstein M, Hedges LV, Higgins JP, Rothstein HR. A basic introduction to fixed-effect and random-effects models for meta-analysis. Res Synth Methods. 2010;1:97–111.
Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ (Clin Res Ed). 2003;327:557–60.
Botteri E, Crosta C, Bagnardi V, et al. Predictors of advanced colorectal neoplasia at initial and surveillance colonoscopy after positive screening immunochemical faecal occult blood test. Digest Liver Dis. 2016;48:321–6.
Brenner H, Calderazzo S, Seufferlein T, et al. Effect of a single aspirin dose prior to fecal immunochemical testing on test sensitivity for detecting advanced colorectal neoplasms: a randomized clinical trial. JAMA. 2019;321:1686–92.
Bujanda L, Lanas Á, Quintero E, et al. Effect of aspirin and antiplatelet drugs on the outcome of the fecal immunochemical test. Mayo Clin Proc. 2013;88:683–9.
Bujanda L, Sarasqueta C, Lanas Á, et al. Effect of oral anticoagulants on the outcome of faecal immunochemical test. Br J Cancer. 2014;110:1334–7.
Denters M, Deutekom M, van Rijn AF, et al. Antithrombotic and/or anticoagulant use is not associated with a higher false positivity rate in CRC screening using FIT. Gastroenterology. 2011;5:413.
Domper Arnal MJ, García Mateo S, Hermoso-Durán S, et al. False-positive fecal immunochemical test results in colorectal cancer screening and gastrointestinal drug use. Int J Colorectal Dis. 2021;36:1861–9.
Ibáñez-Sanz G, Garcia M, Rodríguez-Moranta F, et al. Prescription drugs associated with false-positive results when using faecal immunochemical tests for colorectal cancer screening. Digest Liver Dis. 2016;48:1249–54.
Ibuka T, Adachi S, Horibe Y, et al. Effects of antithrombotic drugs on the results of fecal immunochemical test in colorectal neoplasms screening. Sci Rep. 2021;11:4348.
Niikura R, Yamada A, Fujishiro M, et al. The effects of direct oral anticoagulants, warfarin, aspirin and thienopyridine on the performance of immunochemical, faecal. Occult Blood Tests Digestion. 2019;100:117–26.
Mandelli G, Radaelli F, Paggi S, et al. Anticoagulant or aspirin treatment does not affect the positive predictive value of an immunological fecal occult blood test in patients undergoing colorectal cancer screening: results from a nested in a cohort case-control study. Eur J Gastroenterol Hepatol. 2011;23:323–6.
Ishikawa S, Kato J, Suzuki H, et al. Does low-dose aspirin therapy affect the results of immumochemical fecal occult blood tests? Gastroenterology. 2008;134:626.
Wong MC, Ching JY, Chan VC, et al. Factors associated with false-positive and false-negative fecal immunochemical test results for colorectal cancer screening. Gastrointest Endosc. 2015;81:596–607.
Tsuji Y, Gunji T, Sato H, et al. Antithrombotic drug does not affect the positive predictive value of an immunochemical fecal occult blood test. Digestive Endosc. 2014;26:424–9.
Wauters L, Van der Voort VRH, Dobbels P, et al. Impact of antithrombotics on the fecal immunochemical test for colorectal cancer screening: a multi-center Belgian experience. Acta Gastro-Enterol Belg. 2021;84:19–24.
Ko CW, Riffle S, Michaels L, et al. Serious complications within 30 days of screening and surveillance colonoscopy are uncommon. Clin Gastroenterol Hepatol. 2010;8:166–73.
Rabeneck L, Paszat LF, Hilsden RJ, et al. Bleeding and perforation after outpatient colonoscopy and their risk factors in usual clinical practice. Gastroenterology. 2008;135(1899–906):906.e1.
Rivero-Sánchez L, Grau J, Augé JM, et al. Colorectal cancer after negative colonoscopy in fecal immunochemical test-positive participants from a colorectal cancer screening program. Endosc Int Open. 2018;6:E1140–8.
Luni FK, Riaz H, Khan AR, et al. Clinical outcomes associated with per-operative discontinuation of aspirin in patients with coronary artery disease: a systematic review and meta-analysis. Catheterization Cardiovasc Intervent. 2017;89:1168–75.
Desai J, Granger CB, Weitz JI, Aisenberg J. Novel oral anticoagulants in gastroenterology practice. Gastrointest Endosc. 2013;78:227–39.
Imhann F, Bonder MJ, Vich Vila A, et al. Proton pump inhibitors affect the gut microbiome. Gut. 2016;65:740–8.
Nagata N, Niikura R, Aoki T, et al. Effect of proton-pump inhibitors on the risk of lower gastrointestinal bleeding associated with NSAIDs, aspirin, clopidogrel, and warfarin. J Gastroenterol. 2015;50:1079–86.
Wallace JL, Syer S, Denou E, et al. Proton pump inhibitors exacerbate NSAID-induced small intestinal injury by inducing dysbiosis. Gastroenterology. 2011;141(1314–22):22.e1-5.
Ibáñez-Sanz G, Milà N, de la Peña-Negro LC, et al. Proton-pump inhibitors are associated with a high false-positivity rate in faecal immunochemical testing. J Gastroenterol. 2021;56:42–53.
Acknowledgements
We thank all authors who provided data for this meta-analysis. We would like to thank Editage (www.editage.cn) for English language editing.
Funding
None.
Author information
Authors and Affiliations
Contributions
ZXH and XPN were responsible for design of this research and drafted the manuscript. YYL and MJM collected and analyzed the data. RCZ, JL and PZW provided critical revision of the manuscript. YQL supervised the implementation of the whole process. All authors read and approved the final manuscript. We thank all collaborators who contributed to this study.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Han, Z., Nan, X., Ma, M. et al. Effect of aspirin, warfarin, and proton-pump inhibitors on performance of fecal immunochemical test in colorectal cancer screening: a systematic review and meta-analysis. Clin Exp Med 23, 4355–4368 (2023). https://doi.org/10.1007/s10238-023-01196-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10238-023-01196-w