Abstract
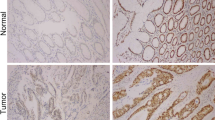
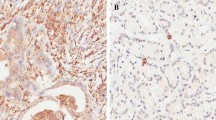
Forkhead Box M1 (FOXM1)—a key cell cycle regulator is a member of the Forkhead transcription factor family. It plays a key role in embryogenesis and cell proliferation and has been strongly linked to various solid tumors. We sought to understand the regulation of FOXM1 in colorectal cancer (CRC), as well as if and to what extent other clinicopathological characteristics are associated with FOXM1. The investigation comprised 98 CRC samples and normal tissues (controls). All colon cancer patients had a colonoscopy and targeted biopsy. All rectal cancer patients had a CT and MRI. Real-time PCR, Immunohistochemistry, and Western blotting were used to evaluate FOXM1 expression, and the findings were analyzed using SPSS (v.26). FOXM1 mRNA and protein expression were substantially upregulated in tumor tissues, with the majority of these proteins localized in nucleo-cytoplasm. Elevated protein levels of FOXM1 were strongly correlated with lower education level, larger tumor size, lymph node status, lymphovascular invasion (LVI), perineural invasion (PNI), lymph node metastasis (LNM), tumor invasion depth (subserosal and serosal invasion), late stage (III and IV), localization (nucleo-cytoplasmic), intensity (strong) and recurrence. Based on survival analysis, FOXM1 overexpression and nucleo-cytoplasmic localization were associated with shorter disease-free survival while stage and PNI were linked to poorer overall and disease-free survival. According to the results of the Cox regression analysis, stage and PNI were significant predictors of prognosis in CRC patients. FOXM1 expression was elevated in CRC and was linked to reduced disease-free survival. These findings support prior reports and hence FOXM1 can be an important prognostic marker for CRC and a promising therapeutic target. Additionally, we found a link between poor disease-free survival and FOXM1's nucleo-cytoplasmic localization. However, since the sample size of this study was small, further research is needed to validate our findings.







Similar content being viewed by others
Change history
20 December 2022
A Correction to this paper has been published: https://doi.org/10.1007/s10238-022-00956-4
References
Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, Bray F. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71(3):209–49. https://doi.org/10.3322/caac.21660.
Bray F, Stewart B, Wild C. World cancer report 2014. Transitions in human development and the global cancer burden: International Agency for Research on Cancer Lyon, 2014
Fidler MM, Soerjomataram I, Bray F. A global view on cancer incidence and national levels of the human development index. Int J Cancer. 2016;139(11):2436–46. https://doi.org/10.1002/ijc.30382.
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68(6):394–424. https://doi.org/10.3322/caac.21492.
Edwards BK, Ward E, Kohler BA, Eheman C, Zauber AG, Anderson RN, Jemal A, Schymura MJ, Lansdorp-Vogelaar I, Seeff LC, van Ballegooijen M, Goede SL, Ries LA. Annual report to the nation on the status of cancer, 1975–2006, featuring colorectal cancer trends and impact of interventions (risk factors, screening, and treatment) to reduce future rates. Cancer. 2010;116(3):544–73. https://doi.org/10.1002/cncr.24760.
De Rosa M, Pace U, Rega D, Costabile V, Duraturo F, Izzo P, Delrio P. Genetics, diagnosis and management of colorectal cancer (Review). Oncol Rep. 2015;34(3):1087–96. https://doi.org/10.3892/or.2015.4108.
Karahalios A, Simpson JA, Baglietto L, MacInnis RJ, Hodge AM, Giles GG, English DR. Change in weight and waist circumference and risk of colorectal cancer: results from the Melbourne Collaborative Cohort Study. BMC Cancer. 2016;16:157. https://doi.org/10.1186/s12885-016-2144-1.
Chan DS, Lau R, Aune D, Vieira R, Greenwood DC, Kampman E, Norat T. Red and processed meat and colorectal cancer incidence: meta-analysis of prospective studies. PLoS ONE. 2011;6(6): e20456. https://doi.org/10.1371/journal.pone.0020456.
Botteri E, Iodice S, Bagnardi V, Raimondi S, Lowenfels AB, Maisonneuve P. Smoking and colorectal cancer: a meta-analysis. JAMA. 2008;300(23):2765–78. https://doi.org/10.1001/jama.2008.839.
Kekelidze M, D’Errico L, Pansini M, Tyndall A, Hohmann J. Colorectal cancer: current imaging methods and future perspectives for the diagnosis, staging and therapeutic response evaluation. World J Gastroenterol. 2013;19(46):8502–14. https://doi.org/10.3748/wjg.v19.i46.8502.
Laoukili J, Stahl M, Medema RH. FoxM1: at the crossroads of ageing and cancer. Biochem Biophys Acta. 2007;1775(1):92–102. https://doi.org/10.1016/j.bbcan.2006.08.006.
Kalin TV, Ustiyan V, Kalinichenko VV. Multiple faces of FoxM1 transcription factor: lessons from transgenic mouse models. Cell cycle (Georgetown, Tex). 2011;10(3):396–405. https://doi.org/10.4161/cc.10.3.14709.
Laoukili J, Alvarez-Fernandez M, Stahl M, Medema RH. FoxM1 is degraded at mitotic exit in a Cdh1-dependent manner. Cell Cycle (Georgetown, Tex). 2008;7(17):2720–6. https://doi.org/10.4161/cc.7.17.6580.
Laoukili J, Kooistra MR, Brás A, Kauw J, Kerkhoven RM, Morrison A, Clevers H, Medema RH. FoxM1 is required for execution of the mitotic programme and chromosome stability. Nat Cell Biol. 2005;7(2):126–36. https://doi.org/10.1038/ncb1217.
Bella L, Zona S, de Moraes GN, Lam EW-F. FOXM1: A key oncofoetal transcription factor in health and disease. Proceedings of the Seminars in cancer biology; 2014. Elsevier: 32–39
Bella L, Zona S, Nestal de Moraes G, Lam EW. FOXM1: a key oncofoetal transcription factor in health and disease. Semin Cancer Biol. 2014;29:32–9. https://doi.org/10.1016/j.semcancer.2014.07.008.
Liao G-B, Li X-Z, Zeng S, Liu C, Yang S-M, Yang L, Hu C-J, Bai J-Y. Regulation of the master regulator FOXM1 in cancer. Cell Commun Signal. 2018;16(1):57. https://doi.org/10.1186/s12964-018-0266-6.
Gonzalez DM, Medici D. Signaling mechanisms of the epithelial-mesenchymal transition. Sci Signal. 2014;7(344):re8. https://doi.org/10.1126/scisignal.2005189.
Grant CM, Kyprianou N. Epithelial mesenchymal transition (EMT) in prostate growth and tumor progression. Transl Androl Urol. 2013;2(3):202–11. https://doi.org/10.3978/j.issn.2223-4683.2013.09.04.
Ombrato L, Malanchi I. The EMT universe: space between cancer cell dissemination and metastasis initiation. Crit Rev Oncog. 2014;19(5):349–61. https://doi.org/10.1615/critrevoncog.2014011802.
Miao L, Xiong X, Lin Y, Cheng Y, Lu J, Zhang J, Cheng N. Down-regulation of FoxM1 leads to the inhibition of the epithelial-mesenchymal transition in gastric cancer cells. Cancer Genet. 2014;207(3):75–82. https://doi.org/10.1016/j.cancergen.2014.02.008.
Kong FF, Qu ZQ, Yuan HH, Wang JY, Zhao M, Guo YH, Shi J, Gong XD, Zhu YL, Liu F, Zhang WY, Jiang B. Overexpression of FOXM1 is associated with EMT and is a predictor of poor prognosis in non-small cell lung cancer. Oncol Rep. 2014;31(6):2660–8. https://doi.org/10.3892/or.2014.3129.
Madureira PA, Varshochi R, Constantinidou D, Francis RE, Coombes RC, Yao KM, Lam EW. The Forkhead box M1 protein regulates the transcription of the estrogen receptor alpha in breast cancer cells. J Biol Chem. 2006;281(35):25167–76. https://doi.org/10.1074/jbc.M603906200.
Kalin TV, Wang IC, Ackerson TJ, Major ML, Detrisac CJ, Kalinichenko VV, Lyubimov A, Costa RH. Increased levels of the FoxM1 transcription factor accelerate development and progression of prostate carcinomas in both TRAMP and LADY transgenic mice. Can Res. 2006;66(3):1712–20. https://doi.org/10.1158/0008-5472.Can-05-3138.
Yoshida Y, Wang IC, Yoder HM, Davidson NO, Costa RH. The Forkhead box M1 transcription factor contributes to the development and growth of mouse colorectal cancer. Gastroenterology. 2007;132(4):1420–31. https://doi.org/10.1053/j.gastro.2007.01.036.
Kalinichenko VV, Major ML, Wang X, Petrovic V, Kuechle J, Yoder HM, Dennewitz MB, Shin B, Datta A, Raychaudhuri P, Costa RH. Foxm1b transcription factor is essential for development of hepatocellular carcinomas and is negatively regulated by the p19ARF tumor suppressor. Genes Dev. 2004;18(7):830–50. https://doi.org/10.1101/gad.1200704.
Teh MT, Gemenetzidis E, Chaplin T, Young BD, Philpott MP. Upregulation of FOXM1 induces genomic instability in human epidermal keratinocytes. Mol Cancer. 2010;9:45. https://doi.org/10.1186/1476-4598-9-45.
Chu XY, Zhu ZM, Chen LB, Wang JH, Su QS, Yang JR, Lin Y, Xue LJ, Liu XB, Mo XB. FOXM1 expression correlates with tumor invasion and a poor prognosis of colorectal cancer. Acta Histochem. 2012;114(8):755–62. https://doi.org/10.1016/j.acthis.2012.01.002.
Wang D, Hu G, Du Y, Zhang C, Lu Q, Lv N, Luo S. Aberrant activation of hedgehog signaling promotes cell proliferation via the transcriptional activation of Forkhead Box M1 in colorectal cancer cells. J Exp Clin Cancer Res CR. 2017;36(1):23. https://doi.org/10.1186/s13046-017-0491-7.
Mathew Thomas V, Baby B, Wang K, Lei F, Chen Q, Huang B, Mathew A. Trends in colorectal cancer incidence in India. J Clin Oncol. 2020;38(15_suppl):e16084. https://doi.org/10.1200/JCO.2020.38.15_suppl.e16084.
Bhat S, Chowdri N, Khan M, Parray F, Wani R, Mehraj AJCS. Clinicopathological profile of colorectal cancer in Kashmir. 2019; 2368
Pandith AA, Siddiqi MA. Burden of cancers in the valley of Kashmir: 5 year epidemiological study reveals a different scenario. Tumour Biol. 2012;33(5):1629–37. https://doi.org/10.1007/s13277-012-0418-z.
Khaliq R, Iqbal P, Kuchay S, Pandurangan AK. Strong association and effect of lifestyle and clinicopathological risk factors in colorectal cancer during treatment process: a study based on Kashmiri population. Toxicol Environ Heal Sci. 2021;13(1):73–81. https://doi.org/10.1007/s13530-020-00071-5.
Rasool S, Kadla SA, Rasool V, Ganai BA. A comparative overview of general risk factors associated with the incidence of colorectal cancer. Tumor Biol. 2013;34(5):2469–76. https://doi.org/10.1007/s13277-013-0876-y.
Thiery JP, Acloque H, Huang RY, Nieto MA. Epithelial-mesenchymal transitions in development and disease. Cell. 2009;139(5):871–90. https://doi.org/10.1016/j.cell.2009.11.007.
Vu T, Datta PK. Regulation of EMT in colorectal cancer: a culprit in metastasis. Cancers. 2017;9(12):171.
Fei BY, He X, Ma J, Zhang M, Chai R. FoxM1 is associated with metastasis in colorectal cancer through induction of the epithelial-mesenchymal transition. Oncol Lett. 2017;14(6):6553–61. https://doi.org/10.3892/ol.2017.7022.
Liebig C, Ayala G, Wilks JA, Berger DH, Albo D. Perineural invasion in cancer: a review of the literature. Cancer. 2009;115(15):3379–91. https://doi.org/10.1002/cncr.24396.
Harris EI, Lewin DN, Wang HL, Lauwers GY, Srivastava A, Shyr Y, Shakhtour B, Revetta F, Washington MK. Lymphovascular invasion in colorectal cancer: an interobserver variability study. Am J Surg Pathol. 2008;32(12):1816–21. https://doi.org/10.1097/PAS.0b013e3181816083.
Chatzistefanou I, Lubek J, Markou K, Ord RA. The role of perineural invasion in treatment decisions for oral cancer patients: a review of the literature. J Cranio-maxillo-Fac Surg Off Publ Eur Assoc Cranio-Maxillo-Facial Surg. 2017;45(6):821–5. https://doi.org/10.1016/j.jcms.2017.02.022.
Zhang H, Zhong H, Li L, Ji W, Zhang X. Overexpressed transcription factor FOXM1 contributes to the progression of colorectal cancer. Mol Med Rep. 2016;13(3):2696–700. https://doi.org/10.3892/mmr.2016.4875.
Yao Y, Wang X, Jiang L, Shao X, Zhu X, He S. Prognostic and clinicopathological value of FoxM1 expression in colorectal cancer: a systematic review and meta-analysis. Medicine. 2018;97(52):e13899–e13899. https://doi.org/10.1097/MD.0000000000013899.
Yang K, Jiang B, Lu Y, Shu Q, Zhai P, Zhi Q, Li Q. FOXM1 promotes the growth and metastasis of colorectal cancer via activation of β-catenin signaling pathway. Cancer Manag Res. 2019;11:3779–90. https://doi.org/10.2147/CMAR.S185438.
Chen S-H, Zhang B-Y, Zhou B, Zhu C-Z, Sun L-Q, Feng Y-J. Perineural invasion of cancer: a complex crosstalk between cells and molecules in the perineural niche. Am J Cancer Res. 2019;9(1):1–21.
Faggiano F, Partanen T, Kogevinas M, Boffetta P. Socioeconomic differences in cancer incidence and mortality. IARC Sci Publ. 1997;138:65–176.
Faggiano F, Zanetti R, Costa G. Cancer risk and social inequalities in Italy. J Epidemiol Commun Health. 1994;48(5):447–52. https://doi.org/10.1136/jech.48.5.447.
Luo YD, Ding X, Du HM, Wu YN, Li HQ, Wu HM, Zhang XM. FOXM1 is a novel predictor of recurrence in patients with oral squamous cell carcinoma associated with an increase in epithelial-mesenchymal transition. Mol Med Rep. 2019;19(5):4101–8. https://doi.org/10.3892/mmr.2019.10094.
Valverde A, Peñarando J, Cañas A, López-Sánchez LM, Conde F, Guil-Luna S, Hernández V, Villar C, Morales-Estévez C, de la Haba-Rodríguez J, Aranda E, Rodríguez-Ariza A. The addition of celecoxib improves the antitumor effect of cetuximab in colorectal cancer: role of EGFR-RAS-FOXM1-β- catenin signaling axis. Oncotarget. 2017;8(13):21754–69. https://doi.org/10.18632/oncotarget.15567.
O’Connell JB, Maggard MA, Ko CY. Colon cancer survival rates with the new American Joint Committee on Cancer sixth edition staging. J Natl Cancer Inst. 2004;96(19):1420–5. https://doi.org/10.1093/jnci/djh275.
Zlobec I, Lugli A. Prognostic and predictive factors in colorectal cancer. J Clin Pathol. 2008;61(5):561–9. https://doi.org/10.1136/jcp.2007.054858.
Li L, Wu D, Yu Q, Li L, Wu P. Prognostic value of FOXM1 in solid tumors: a systematic review and meta-analysis. Oncotarget. 2017;8(19):32298–308. https://doi.org/10.18632/oncotarget.15764.
Acknowledgements
The authors would like to thank patients who agreed to take part in this study. The authors would also like to thank the technical personnel of the Department of General Surgery and Pathology for their assistance in obtaining tissue samples and tissue blocks. The authors are thankful to Dr. Syed besina and Dr. Ishrat Younas Khan for providing support for IHC experimental and evaluation analysis
Funding
None.
Author information
Authors and Affiliations
Contributions
TBR wrote the manuscript and did the experimental work. IP and GAB revised the manuscript and assisted in data analysis. GR helped with data collection. RAW provided access to tissue samples. IYK helped in pathological data interpretation. SM drafted the overall design of this study and provided experimental support.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this article was revised: Modifications have been made in tables 3, 4, 5 and 7 and in the text. Full information regarding the corrections made can be found in the erratum for this article.
Rights and permissions
About this article
Cite this article
Rather, T.B., Parveiz, I., Bhat, G.A. et al. Evaluation of Forkhead BOX M1 (FOXM1) gene expression in colorectal cancer. Clin Exp Med 23, 2385–2405 (2023). https://doi.org/10.1007/s10238-022-00929-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10238-022-00929-7