Abstract
Breast cancer was the fourth leading cause of cancer-related death worldwide, and early mammography screening could decrease the breast cancer mortality. Artificial intelligence (AI)-assisted diagnose system based on machine learning (ML) methods can help improve the screening accuracy and efficacy. This study aimed to systematically review and make a meta-analysis on the diagnostic accuracy of mammography diagnosis of breast cancer through various ML methods. Springer Link, Science Direct (Elsevier), IEEE Xplore, PubMed and Web of Science were searched for relevant studies published from January 2000 to September 2021. The study was registered with the PROSPERO International Prospective Register of Systematic Reviews (protocol no. CRD42021284227). A Quality Assessment of Diagnostic Accuracy Studies-2 (QUADAS-2) was used to assess the included studies, and reporting was evaluated using the Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA). The pooled summary estimates for sensitivity, specificity, the area under the receiver operating characteristic curve (AUC) for three ML methods (convolutional neural network [CNN], artificial neural network [ANN], support vector machine [SVM]) were calculated. A total of 32 studies with 23,804 images were included in the meta-analysis. The overall pooled estimate for sensitivity, specificity and AUC was 0.914 [95% CI 0.868–0.945], 0.916 [95% CI 0.873–0.945] and 0.945 for mammography diagnosis of breast cancer through three ML methods. The pooled sensitivity, specificity and AUC of CNN were 0.961 [95% CI 0.886–0.988], 0.950 [95% CI 0.924–0.967] and 0.974. The pooled sensitivity, specificity and AUC of ANN were 0.837 [95% CI 0.772–0.886], 0.894 [95% CI 0.764–0.957] and 0.881. The pooled sensitivity, specificity and AUC of SVM were 0.889 [95% CI 0.807–0.939], 0.843 [95% CI 0.724–0.916] and 0.913. Machine learning methods (especially CNN) show excellent performance in mammography diagnosis of breast cancer screening based on retrospective studies. More rigorous prospective studies are needed to evaluate the longitudinal performance of AI.








Similar content being viewed by others
Availability of data and materials
The data of this study are from published literatures and shown in Appendix B.
References
Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, Bray F. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA-Cancer J Clin. 2021;71(3):209–49.
Parkin DM, Bray F, Ferlay J, Pisani P. Global cancer statistics, 2002. CA-Cancer J Clin. 2005;55(2):74–108.
Jemal A, Bray F, Center MM, Ferlay J, Ward E, Forman D. Global cancer statistics. CA Cancer J Clin. 2011;61(2):69–90.
Torre LA, Bray F, Siegel RL, Ferlay J, Lortet-Tieulent J, Jemal A. Global cancer statistics, 2012. CA-Cancer J Clin. 2015;65(2):87–108.
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA-Cancer J Clin. 2018;68(6):394–424.
Jedy-Agba E, McCormack V, Adebamowo C, dosSantos-Silva I. Stage at diagnosis of breast cancer in sub-Saharan Africa: a systematic review and meta-analysis. Lancet Global Health. 2016;4(12):E923–35.
DeSantis CE, Ma J, Gaudet MM, Newman LA, Miller KD, Sauer AG, Jemal A, Siegel RL. Breast cancer statistics, 2019. CA-Cancer J Clin. 2019;69(6):438–51.
WHO: New global breast cancer initiative highlights renewed commitment to improve survival. https://www.who.int/news/item/08-03-2021-new-global-breast-cancer-initiative-highlights-renewed-commitment-to-improve-survival. Accessed Feb 9, 2022.
Marmot MG, Altman DG, Cameron DA, Dewar JA, Thompson SG, Wilcox M, Independent UKPBCS. The benefits and harms of breast cancer screening: an independent review. Lancet. 2012;380(9855):1778–86.
Duggan C, Trapani D, Ilbawi AM, Fidarova E, Laversanne M, Curigliano G, Bray F, Anderson BO. National health system characteristics, breast cancer stage at diagnosis, and breast cancer mortality: a population-based analysis. Lancet Oncol. 2021;22(11):1632–42.
The Nuffield Trust. Cancer survival rates. https://www.nuffieldtrust.org.uk/resource/breast-and-cervical-cancer-screening. Accessed Feb 9, 2022.
Akinyemiju TF. Socio-economic and health access determinants of breast and cervical cancer screening in low-income countries: analysis of the world health survey. PLoS ONE. 2012;7(11):e48834.
Lauby-Secretan B, Scoccianti C, Loomis D, Benbrahim-Tallaa L, Bouvard V, Bianchini F, Straif K, Handbook IARC, W. Breast-cancer screening—viewpoint of the IARC working group. N Engl J Med. 2015;372(24):2353–8.
Heywang-Koebrunner SH, Hacker A, Sedlacek S. Advantages and disadvantages of mammography screening. Breast Care. 2011;6(3):199–207.
Ribli D, Horvath A, Unger Z, Pollner P, Csabai I. Detecting and classifying lesions in mammograms with deep learning. Sci Rep. 2018. https://doi.org/10.1038/s41598-018-22437-z.
Abdullah P, Alabousi M, Ramadan S, Zawawi I, Zawawi M, Bhogadi Y, Freitas V, Patlas MN, Alabousi A. Synthetic 2D mammography versus standard 2D digital mammography: a diagnostic test accuracy systematic review and meta-analysis. Am J Roentgenol. 2021;217(2):314–24.
Benzebouchi NE, Azizi N, Ayadi K. In A Computer-aided diagnosis system for breast cancer using deep convolutional neural networks, 4th international conference on computational intelligence in data Mining (ICCIDM), Burla, INDIA. 2019. Nov 11–12; Burla, INDIA, 2017; pp 583–593.
Geras KJ, Mann RM, Moy L. Artificial intelligence for mammography and digital breast tomosynthesis: current concepts and future perspectives. Radiology. 2019;293(2):246–59.
Yala A, Schuster T, Miles R, Barzilay R, Lehman C. A deep learning model to triage screening mammograms: a simulation study. Radiology. 2019;293(1):38–46.
Lehman CD, Wellman RD, Buist DSM, Kerlikowske K, Tosteson ANA, Miglioretti DL, Breast Canc S. Diagnostic accuracy of digital screening mammography with and without computer-aided detection. JAMA Intern Med. 2015;175(11):1828–37.
Gur D, Sumkin JH, Rockette HE, Ganott M, Hakim C, Hardesty L, Poller WR, Shah R, Wallace L. Changes in breast cancer detection and mammography recall rates after the introduction of a computer-aided detection system. J Natl Cancer Inst. 2004;96(3):185–90.
Fenton JJ, Taplin SH, Carney PA, Abraham L, Sickles EA, D’Orsi C, Berns EA, Cutter G, Hendrick RE, Barlow WE, Elmore JG. Influence of computer-aided detection on performance of screening mammography. N Engl J Med. 2007;356(14):1399–409.
Fenton JJ, Abraham L, Taplin SH, Geller BM, Carney PA, D’Orsi C, Elmore JG, Barlow WE, Breast Canc Surveillance C. Effectiveness of computer-aided detection in community mammography practice. J Natl Cancer Inst. 2011;103(15):1152–61.
Azavedo E, Zackrisson S, Mejare I, Arnlind MH. Is single reading with computer-aided detection (CAD) as good as double reading in mammography screening? A systematic review. Bmc Med Imaging. 2012;12.
Gilbert FJ, Astley SM, McGee MA, Gillan MGC, Boggis CRM, Griffiths PM, Duffy SW. Single reading with computer-aided detection and double reading of screening mammograms in the United Kingdom national breast screening program. Radiology. 2006;241(1):47–53.
McKinney SM, Sieniek M, Godbole V, Godwin J, Antropova N, Ashrafian H, Back T, Chesus M, Corrado GC, Darzi A, Etemadi M, Garcia-Vicente F, Gilbert FJ, Halling-Brown M, Hassabis D, Jansen S, Karthikesalingam A, Kelly CJ, King D, Ledsam JR, Melnick D, Mostofi H, Peng L, Reicher JJ, Romera-Paredes B, Sidebottom R, Suleyman M, Tse D, Young KC, De Fauw J, Shetty S. International evaluation of an AI system for breast cancer screening. Nature. 2020;577(7788):89–94.
Kim HE, Kim HH, Han BK, Kim KH, Han K, Nam H, Lee EH, Kim EK. Changes in cancer detection and false-positive recall in mammography using artificial intelligence: a retrospective, multireader study. Lancet Digit Health. 2020;2(3):E138–48.
Rodriguez-Ruiz A, Lang K, Gubern-Merida A, Broeders M, Gennaro G, Clauser P, Helbich TH, Chevalier M, Tan T, Mertelmeier T, Wallis MG, Andersson I, Zackrisson S, Mann RM, Sechopoulos I. Stand-alone artificial intelligence for breast cancer detection in mammography: comparison with 101 radiologists. JNCI-J Natl Cancer Inst. 2019;111(9):916–22.
Gilbert FJ, Astley SM, Gillan MGC, Agbaje OF, Wallis MG, James J, Boggis CRM, Duffy SW, Grp CI. Single reading with computer-aided detection for screening mammography. N Engl J Med. 2008;359(16):1675–84.
Salim M, Wahlin E, Dembrower K, Azavedo E, Foukakis T, Liu Y, Smith K, Eklund M, Strand F. External evaluation of 3 commercial artificial intelligence algorithms for independent assessment of screening mammograms. JAMA Oncol. 2020; 6(10):1581-1588.
Schaffter T, Buist DSM, Lee CI, Nikulin Y, Ribli D, Guan Y, Lotter W, Jie Z, Du H, Wang S, Feng J, Feng M, Kim H-E, Albiol F, Albiol A, Morrell S, Wojna Z, Ahsen ME, Asif U, Yepes AJ, Yohanandan S, Rabinovici-Cohen S, Yi D, Hoff B, Yu T, Neto EC, Rubin DL, Lindholm P, Margolies LR, McBride RB, Rothstein JH, Sieh W, Ben-Ari R, Harrer S, Trister A, Friend S, Norman T, Sahiner B, Strand F, Guinney J, Stolovitzky G, Consortium DD. Evaluation of combined artificial intelligence and radiologist assessment to interpret screening mammograms. Jama Netw Open (2020); 3(3):e200265–e200265.
Rodriguez-Ruiz A, Krupinski E, Mordang J-J, Schilling K, Heywang-Koebrunner SH, Sechopoulos J, Mann RM. Detection of breast cancer with mammography: effect of an artificial intelligence support system. Radiology. 2019;290(2):305–14.
American college of radiology data science institute. AI central. https://aicentral.acrdsi.org/. Accessed April 9, 2022
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan SE, Chou R, Glanville J, Grimshaw JM, Hrobjartsson A, Lalu MM, Li T, Loder EW, Mayo-Wilson E, McDonald S, McGuinness LA, Stewart LA, Thomas J, Tricco AC, Welch VA, Whiting P, Moher D, The PRISMA. statement: an updated guideline for reporting systematic reviews. Int J Surg. 2020;2021:88.
Hosny A, Parmar C, Quackenbush J, Schwartz LH, Aerts HJWL. Artificial intelligence in radiology. Nat Rev Cancer. 2018;18(8):500–10.
Whiting PF, Rutjes AWS, Westwood ME, Mallett S, Deeks JJ, Reitsma JB, Leeflang MMG, Sterne JAC, Bossuyt PMM, Grp Q. QUADAS-2: a revised tool for the quality assessment of diagnostic accuracy studies. Ann Intern Med. 2011;155(8):529-U104.
Rose DC, Arel I, Karnowski TP, Paquit VC. Applying deep-layered clustering to mammography image analytics. 2010; p. 4-14
Danala G, Patel B, Aghaei F, Heidari M, Li J, Wu T, Zheng B. Classification of breast masses using a computer-aided diagnosis scheme of contrast enhanced digital mammograms. Ann Biomed Eng. 2018;46(9):1419–31.
Heidari M, Khuzani AZ, Danala G, Qiu Y, Zheng B. In improving performance of breast cancer risk prediction using a new cad-based region segmentation scheme, conference on medical imaging—computer-aided diagnosis. Houston:TX; 2018.
Heidari M, Mirniaharikandehei S, Danala G, Qiu Y, Zheng B. In A new case-based CAD scheme using a hierarchical SSIM feature extraction method to classify between malignant and benign cases, SPIE Conference on medical imaging–imaging informatics for healthcare, research, and applications. Houston:TX; 2020.
Heidari M, Lakshmivarahan S, Mirniaharikandehei S, Danala G, Maryada SKR, Liu H, Zheng B. Applying a random projection algorithm to optimize machine learning model for breast lesion classification. IEEE Trans Biomed Eng. 2021;68(9):2764–75.
Ray A, Ming C, Gelogo Y. Performance comparison of different machine learning algorithms for risk prediction and diagnosis of breast cancer. 2020; p. 71–6.
Kanchanamani M, Perumal V. Performance evaluation and comparative analysis of various machine learning techniques for diagnosis of breast cancer. Biomed Res India. 2016;27(3):623–31.
Pharswan R, Singh J. Performance analysis of SVM and KNN in breast cancer classification: a survey. In: internet of things and big data applications. Springer; 2020:pp 133-140.
Kar S, Majumder DD. An investigative study on early diagnosis of breast cancer using a new approach of mathematical shape theory and neuro-fuzzy classification system. Int J Fuzzy Syst. 2016;18(3):349–66.
Xiaoming L, Jun L, Zhilin F. Mass classification in mammography with morphological features and multiple kernel learning. 2011: p 4 pp.-4.
Liu X, Xu X, Liu J, Tang J. In mass classification with level set segmentation and shape analysis for breast cancer diagnosis using mammography, 7th international conference on intelligent computing (ICIC). Zhengzhou; People’s Republic of China:2012.
Wang Y, Yang F, Zhang J, Wang H, Yue X, Liu S. Application of artificial intelligence based on deep learning in breast cancer screening and imaging diagnosis. Neural Comput Appl. 2021;33(15):9637–47.
Lu H-C, Loh E-W, Huang S-C. Ieee in the classification of mammogram using convolutional neural network with specific image preprocessing for breast cancer detection, 2nd international conference on artificial intelligence and big data (ICAIBD). Chengdu; People’s Republic of China:pp 9–12.
Alkhaleefah M, Wu C-C. Ieee in a hybrid CNN and RBF-based SVM approach for breast cancer classification in mammograms, IEEE international conference on systems, man, and cybernetics (SMC). IEEE Syst Man & Cybernet Soc; Miyazaki, JAPAN:2018.
Alkhaleefah M, Chittem PK, Achhannagari VP, Ma S-C, Chang Y-L. Ieee in the influence of image augmentation on breast lesion classification using transfer learning, international conference on artificial intelligence and signal processing (AISP). VIT AP Univ, Amaravati; INDIA:2020.
Bae JH, Park JH, Park JH, Sunwoo MH. Ieee in multi-channel input deep convolutional neural network for mammogram diagnosis, 17th international SoC design conference (ISOCC). Yeosu; South Korea:2020:pp 23-24.
Al-masni MA, Al-antari MA, Park JM, Gi G, Kim TY, Rivera P, Valarezo, E, Han SM, Kim TS. Ieee in detection and classification of the breast abnormalities in digital mammograms via regional convolutional neural network, 39th annual international conference of the IEEE-engineering-in-medicine-and-biology-society (EMBC). South Korea: 2017:pp 1230–1233.
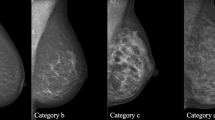
Suh YJ, Jung J, Cho B-J. Automated breast cancer detection in digital mammograms of various densities via deep learning. J Pers Med. 2020;10(4):211.
Zebari DA, Zeebaree DQ, Abdulazeez AM, Haron H, Hamed HNA. Improved threshold based and trainable fully automated segmentation for breast cancer boundary and pectoral muscle in mammogram images. Ieee Access. 2020;8:203097–116.
Faisal Z, El Abbadi NK. In breast cancer recognition by computer aided based on improved fuzzy c-mean and ann, international conference on new trends in information and communications technology applications. Springer:Cham; 2020:pp 246–257.
Braz Junior G, de Paiva AC, Silva AC, Muniz de Oliveira AC. Classification of breast tissues using Moran’s index and Geary’s coefficient as texture signatures and SVM. Comput Biol Med. 2009;39(12):1063–72.
da Silva VR, Jr. de Paiva AC, Silva AC, Muniz de Oliveira AC. Semivariogram applied for classification of benign and malignant tissues in mammography. In Campilho A, Kamel M, editors. Image analysis and recognition, Pt 2, 2006:Vol. 4142, pp. 570–579.
Touahri R, Azizi N, Hammami NE, Aldwairi M, Benaida F. Ieee in automated breast tumor diagnosis using local binary patterns (LBP) based on deep learning classification, international conference on computer and information sciences (ICCIS), Jouf Univ, Sakaka, SAUDI ARABIA, 2019 Apr 03–04; Jouf Univ, Sakaka, SAUDI ARABIA, 2019:pp 309–313.
Keles A, Keles A. Extracting fuzzy rules for the diagnosis of breast cancer. Turk J Electr Eng Comput Sci. 2013;21(5):1495–503.
Abdel Rahman AS, Belhaouari SB, Bouzerdoum A, Baali H, Alam T, Eldaraa AM, Breast mass tumor classification using deep learning. 2020:p. 271–6.
Music L, Gabeljic N. In predicting the severity of a mammographic tumor using an artificial neural network, international conference on medical and biological engineering in bosnia and herzegovina (CMBEBIH), Banja Luka, BOSNIA & HERCEG, 2020.
Yemini M, Zigel Y, Lederman D. Ieee In detecting masses in mammograms using convolutional neural networks and transfer learning, IEEE International conference on the science of electrical engineering in Israel (ICSEE), Eilat, ISRAEL, 2018 Dec 12–14; Eilat, ISRAEL, 2018.
Derbel N, Tmar H, Mahfoudhi A. A multi-view deep convolutional neural network for reduction of false positive findings in breast cancer screening. 2020:p. 6 pp.-6.
Stelzer PD, Steding O, Raudner MW, Euller G, Clauser P, Baltzer PAT. (2020) Combined texture analysis and machine learning in suspicious calcifications detected by mammography: potential to avoid unnecessary stereotactical biopsies. Eur J Radiol. 2020;132:109309.
Laghmati S, Tmiri A, Cherradi B. In machine learning based system for prediction of breast cancer severity, international conference on wireless networks and mobile communications (WINCOM). Fac Sci Technol Fez, Fez, MOROCCO, 2019.
SaA H, Sayed MS, Abdalla MI, Rashwan MA. Breast cancer masses classification using deep convolutional neural networks and transfer learning. Multimed Tools Appl. 2020;79(41–42):30735–68.
Heath M, Bowyer K, Kopans D, Moore R, Kegelmeyer P. In The digital database for screening mammography, 5th international workshop on digital mammography. Toronto: Canada; 2001.
Lopez MAGy, de Posada NG, Moura DC, Pollan RR, Franco Valiente J M, Ortega CS, del Solar MR, Herrero GD, Pereira Ramos IMA, Loureiro JP, Fernandes TC, Ferreira de Araujo BM. In BCDR: a breast cancer digital repository, 15th international conference on experimental mechanics (ICEM). 2012. Univ Porto, Fac Engn (FEUP), Porto, PORTUGAL, 22–27; Univ Porto, Fac Engn (FEUP), Porto, PORTUGAL.
Suckling J, Parker J, Dance DR, Astley S, Hutt I, Boggis CRM, Ricketts I, Stamatakis E, Cerneaz N, Kok SL, Taylor P, Betal D, Savage J. The mammographic image analysis society digital mammogram database. In Gale AG, Astley SM, Dance DR, Cairns AY, editors. International congress series; digital mammography. 1994; Vol. 1069, pp. 375–378.
Moreira IC, Amaral I, Domingues I, Cardoso A, Cardoso MJ, Cardoso JS. INbreast: toward a full-field digital mammographic database. Acad Radiol. 2012;19(2):236–48.
Sechopoulos I, Mann RM. Stand-alone artificial intelligence—the future of breast cancer screening? Breast. 2020;49:254–60.
Wing P, Langelier MH. Workforce shortages in breast imaging: impact on mammography utilization. Am J Roentgenol. 2009;192(2):370–8.
Gulland A. Staff shortages are putting UK breast cancer screening “at risk,” survey finds. BMJ. 2016;353:i2350.
Morrone D, Giordano L, Artuso F, Bernardi D, Fedato C, Frigerio A, Giorgi D, Naldoni C, Saguatti G, Severi D, Taffurelli M, Terribile D, Ventura L, Bucchi L. The professional quality criteria of Italian breast screening radiologists: results from a national survey comparing the programmes started in 2000–2012 versus the ones started in 1990–1999. Ann Ist Super Sanita. 2017;53(2):163–6.
Warren-Forward HM, Taylor J. Barriers and incentives for choosing to specialise in mammography: qualitative analysis. Radiography. 2017;23(1):32–7.
Carter SM, Rogers W, Win KT, Frazer H, Richards B, Houssami N. The ethical, legal and social implications of using artificial intelligence systems in breast cancer care. Breast. 2020;49:25–32.
Gastounioti A, Desai S, Ahluwalia VS, Conant EF, Kontos D. Artificial intelligence in mammographic phenotyping of breast cancer risk: a narrative review. Breast Cancer Res. 2022. https://doi.org/10.1186/s13058-022-01509-z.
Hickman SE, Woitek R, Le EPV, Im YR, Luxhoj CM, Aviles-Rivero AI, Baxter GC, MacKay JW, Gilbert FJ. Machine learning for workflow applications in screening mammography: systematic review and meta-analysis. Radiology. 2022;302(1):88–104.
Fleuren LM, Klausch TLT, Zwager CL, Schoonmade LJ, Guo T, Roggeveen LF, Swart EL, Girbes ARJ, Thoral P, Ercole A, Hoogendoorn M, Elbers PWG. Machine learning for the prediction of sepsis: a systematic review and meta-analysis of diagnostic test accuracy. Intensive Care Med. 2020;46(3):383–400.
Acknowledgements
We thank Zengbin Li and Rui Li for good suggestions in meta-analysis.
Funding
This work was supported by the National Natural Science Foundation of China (12171387 (MS)); China Postdoctoral Science Foundation (2018M631134 (MS), 2020T130095ZX (MS)); Young Talent Support Program of Shaanxi University Association for Science and Technology (20210307 (MS)). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
MS and JL conceived and designed the study. JL, HO, JL, YZ and XT collected the data. JL analyzed the data, carried out the analysis and performed numerical simulations. JL wrote the first draft of the manuscript. MS critically revised the manuscript. All the authors contributed to writing the paper and agreed with the manuscript results and conclusions.
Corresponding author
Ethics declarations
Competing interests
All authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
10238_2022_895_MOESM1_ESM.pdf
Appendix A is a combination of terms used in our search of the five databases. The five electronic databases are Springer Link, Science Direct, IEEE Xplore, PubMed and Web of Science (PDF 44 KB)
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Liu, J., Lei, J., Ou, Y. et al. Mammography diagnosis of breast cancer screening through machine learning: a systematic review and meta-analysis. Clin Exp Med 23, 2341–2356 (2023). https://doi.org/10.1007/s10238-022-00895-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10238-022-00895-0