Abstract
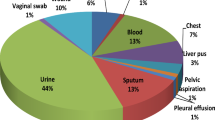
The treatment for infections in hospitalized patients can be summarized in the timely start of empirical therapy, followed by adjustment on the basis of isolates and microbial susceptibilities. Initial therapy may be based on international guidelines. However, to know local frequencies of bacterial and fungal strains together with patterns of drug resistance should be a better approach to therapy. REGIMEN is a retrospective observational study of all consecutive recorded bacterial and fungal isolates, collected between October 2009 and August 2011 from patients admitted in a 53-bedded ward of internal medicine of a non-teaching Italian hospital. We investigated type of samples and of microorganisms, patterns of susceptibility and resistance to antibiotics, and in-hospital mortality. A total of 504 samples were examined (244 from urine, 189 from blood and 71 from skin and various exudates). Participants were old (mean age, 83 years), and so overall mortality was high (20 %). There were high frequencies of drug resistance; only 27.9 % of urinary gram-negatives and 52.6 % of blood gram-negatives were susceptible to levofloxacin. Susceptibility profiles compatible with the presence of extended-spectrum beta-lactamases were present in 64.2 % of gram-negative strains, and 10.1 % were also resistant to carbapenems. ESKAPE organisms account for a third of all bacterial infections. Local patterns of drug resistance should influence empirical antibiotic therapy for patients admitted in internal medicine wards, where mortality is high.



Similar content being viewed by others
References
Leeka S, Terrel CL, Edson RS (2011) General principles of antimicrobial therapy. Mayo Clin Proc 86:156–167
Delinger RP, Levy MM, Carlet JM et al (2008) Surviving Sepsis Campaign: international guidelines for management of severe sepsis and septic shock 2008. Crit Care Med 36:296–327
Kollef MH, Sherman G, Ward S, Fraser VJ (1999) Inadequate antimicrobial treatment of infections: a risk factor for hospital mortality among critically ill patients. Chest 115:462–474
Ibrahim EH, Sherman G, Ward S, Fraser VJ, Kollef MH (2000) The influence of inadequate antimicrobial treatment of bloodstream infections on patient outcomes in the ICU setting. Chest 118:146–155
Thompson RL, Wright AJ (1998) General principles of antimicrobial therapy. Mayo Clin Proc 73:995–1006
Prevention of catheter-associated urinary tract infection (2008) In: Betsy Lehman Center for Patient Safety and Medical Error Reduction. JSI Research and Training Institute, Inc. Prevention and control of healthcare-associated infections in Massachusetts. Part 1: final recommendations of the Expert Panel. Boston (MA): Massachusetts Department of Public Health, pp 83–89
Lo E, Nicolle L, Classen D et al (2008) Strategies to prevent catheter-associated urinary tract infections in acute care hospitals. Infect Control Hosp Epidemiol 1:S41–S50
Horan TC, Andrus MA, Dudeck MA (2008) CDC/NHSN surveillance definition of health care-associated infection and criteria for specific types of infections in the acute care setting. Am J Infect Control 36:309–332
CLSI 2009. Performance standards for disk susceptibility tests. Approved standard, 10th Ed, M02-A10 Clinical and Laboratory Standards Institute, Wayne
American College of Obstetricians and Gynecologists (ACOG) (2008) ACOG Practice Bulletin No. 91: treatment of urinary tract infections in nonpregnant women. Obstet Gynecol 111(3):785–794
University of Michigan Health System (UMHS) (2005) Urinary tract infection. Ann Arbor (MI), 2005. Accessed at http://www.med.umich.edu/1info/fhp/practiceguides/uti/uti.pdf on 2010/11/13
Scottish Intercollegiate Guidelines Network (SIGN) (2006) Management of suspected bacterial urinary tract infection. Nurs Times 102(36):25–26
Hooton TM, Bradley SF, Cardenas DD, Colgan R, Geerlings SE, Rice JC et al (2010) Diagnosis, Prevention, and Treatment of Catheter-Associated Urinary Tract Infection in Adults: 2009 International Clinical Practice Guidelines from the Infectious Diseases Society of America. Clin Infect Dis 50:625–663
Grabe M, Bishop MC, Bjerklund-Johansen TE et al (2009) Guidelines on urological infections. Arnhem. http://www.med.umich.edu/1info/fhp/practiceguides/uti/uti.pdf. Accessed 13 Nov 2010
Paul M, Shani V, Muchtar E, Kariv G, Robenshtok E, Leibovici L (2010) Systematic review and meta-analysis of the efficacy of appropriate empiric antibiotic therapy for sepsis. Antimicrob Agents Chemother 54:4851–4863
Micek ST, Welch EC, Khan J, Pervez M, Doherty JA, Reichley RM et al (2011) Resistance to empiric antimicrobial treatment predicts outcome in severe sepsis associated with gram-negative bacteremia. J Hosp Med 6:405–410
Vogelaers D, De Bels D, Foret F, Cran S, Gilbert E, Scoonheydt K et al (2010) Patterns of antimicrobial therapy in severe nosocomial infections: empiric choices, proportion of appropriate therapy, and adaptation rates–a multicentre, observational survey in critically ill patients. Int J Antimicrob Agents 35:375–381
Pop-Vicas A, Tacconelli E, Gravestein S, D’Agata EM (2009) Influx of multidrug-resistant, gram-negative bacteria in the hospital setting and the role of elderly patients with bacterial bloodstream infection. Infect Control Hosp Epidemiol 30:325–331
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Cei, M., Pardelli, R., Sani, S. et al. Local resistance patterns to antimicrobials in internal medicine: a focused report from the REGIMEN (REGistro Infezioni in MEdicina INterna) study. Clin Exp Med 14, 77–82 (2014). https://doi.org/10.1007/s10238-012-0219-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10238-012-0219-0