Abstract
The goal of this work is to assess the impact of vascular anatomy definition degree in the predictions of blood flow models of the arterial network. To this end, results obtained with an anatomically detailed network containing over 2000 vessels are systematically compared with those obtained with an anatomically simplified network containing the main 86 vessels, the latter being a truncated version of the former one. The comparison is performed quantitatively and qualitatively in terms of pressure and flow rate waveforms, wave intensity analysis and impedance analysis. Comparisons are performed under physiological conditions and for the case of common carotid artery occlusion. Mechanisms of blood flow delivery to the brain, as well as different blood flow steal phenomena, are unveiled in light of model predictions. Results show that detailed and simplified models are in reasonable agreement regarding the hemodynamics in larger vessels and in healthy scenarios. The anatomically detailed arterial network features improved predictive capabilities at peripheral vessels. Moreover, discrepancies between models are substantially accentuated in the case of anatomical variations or abnormal hemodynamic conditions. We conclude that physiologically meaningful agreement between models is obtained for normal hemodynamic conditions. This agreement rapidly deteriorates for abnormal blood flow conditions such as those caused by total arterial occlusion. Differences are even larger when modifications of the vascular anatomy are considered. This rational comparison allows us to gain insight into the need for anatomically detailed arterial networks when addressing complex hemodynamic interactions.









Similar content being viewed by others
References
Alastruey J, Parker K, Peiró J, Byrd S, Sherwin S (2007) Modelling the circle of Willis to assess the effects of anatomical variations and occlusions on cerebral flows. J Biomech 40:1794–1805
Alastruey J, Hunt A, Weinberg P (2014) Novel wave intensity analysis of arterial pulse wave propagation accounting for peripheral reflections. Ann Biomed Eng 30:249–279
Armentano R, Levenson J, Barra J, Cabrera E, Breitbart G, Pichel R, Simon A (1991) Assessment of elastin and collagen contribution to aortic elasticity in concious dogs. Am J Physiol Heart Circ Physiol 260:H1870–H1877
Avolio A (1980) Multi-branched model of the human arterial system. Med Biol Eng Comput 18:709–718
Avolio A, Van Bortel L, Boutouyrie P, Cockcroft J, McEniery C, Protogerou A, Roman M, Safar M, Segers P, Smulyan H (2009) Role of pulse pressure amplification in arterial hypertension: experts’ opinion and review of the data. Hypertension 54:375–383
Blanco P, Watanabe S, Dari E, Passos M, Feijóo R (2014) Blood flow distribution in an anatomically detailed arterial network model: criteria and algorithm. Biomech Model Mechanobiol 13:1303–1330
Blanco P, Watanabe S, Passos M, Lemos P, Feijóo R (2015) An anatomically detailed arterial network model for one-dimensional computational hemodynamics. IEEE Trans Biomed Eng 62:736–753
Blanco P, Müller L, Watanabe S, Feijóo R (2016) Computational modeling of blood flow steal phenomena caused by subclavian stenoses. J Biomech 49(9):1593–1600
Blanco PJ, Müller LO, Spence JD (2017) Blood pressure gradients in cerebral arteries: a clue to pathogenesis of cerebral small vessel disease. Stroke Vasc Neurol 3(e000):087
Bokkers R, Wessels F, van der Worp H, Zwanenburg J, Mali W, Hendrikse J (2011) Vasodilatory capacity of the cerebral vasculature in patients with carotid artery stenosis. AJNR Am J Neuroradiol 32:1030–1033
Burton A (1954) Relation of structure to function of the tissues of the wall of blood vessels. Physiol Rev 34:619–642
Dauber W (2007) Pocket atlas of human anatomy by Feneis, 5th edn. Thieme, New York
Dorrance G (1934) Ligation of the great vessels of the neck. Ann Surg 99:721–742
Epstein S, Willemet M, Chowienczyk P, Alastruey J (2015) Reducing the number of parameters in 1d arterial blood flow modeling: less is more for patient-specific simulations. Am J Physiol Heart Circ Physiol 309:H222–H234
Fossan FE, Mariscal-Harana J, Alastruey J, Hellevik LR (2018) Optimization of topological complexity for one-dimensional arterial blood flow models. J R Soc Interface 15(149):20180,546
Geelkerken RH, Lamers CB, Delahunt TA, Hermans J, Zwijsen JH, van Bockel J (1998) Duodenal meal stimulation leads to coeliac artery vasoconstriction and superior mesenteric artery vasodilatation: an intra-abdominal ultrasound study. Ultrasound Med Biol 24(9):1351–1356
Godlevska M, Slutskii L, Purinya B (1974) Comparison of the mechanical and biochemical characteristics of human brain arteries. Polym Mech 10:941–949
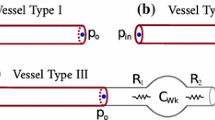
Guan D, Liang F, Gremaud PA (2016) Comparison of the windkessel model and structured-tree model applied to prescribe outflow boundary conditions for a one-dimensional arterial tree model. J Biomech 49(9):1583–1592
Heald C, Fowkes F, Murray G, Price J (2006) Risk of mortality and cardiovascular disease associated with the ankle-brachial index: systematic review. Atherosclerosis 189:61–69
HeMoLab (2013) ADAN-WEB application. http://hemolab.lncc.br/adan-web. Accessed 4 Feb 2020
Ho H, McGhee C, Hunter P (2012) Numerical analysis for the blood flow in a patient-specific ophthalmic artery. Med Eng Phys 34:123–127
Jianu A, Motoc A, Mihai A, Rusu M (2009) An anatomical study of the thyroid arteries anastomoses. Rom J Morphol Embryol 50:97–101
Koeppl T, Schneider M, Pohl U, Wohlmuth B (2014) The influence of an unilateral carotid artery stenosis on brain oxygenation. Med Eng Phys 36:905–914
Liang F, Takagi S, Himeno R, Liu H (2009) Biomechanical characterization of ventricular-arterial coupling during aging: a multi-scale model study. J Biomech 42(6):692–704
Liang F, Fukasaku K, Liu H, Takagi S (2011) A computational model study of the influence of the anatomy of the circle of willis on cerebral hyperperfusion following carotid artery surgery. BioMed Eng OnLine 10:84
Liebeskind D (2003) Collateral circulation. Stroke 34:2279–2284
Matthys K, Alastruey J, Peiró J, Khir A, Segers P, Verdonck P, Parker K, Sherwin S (2007) Pulse wave propagation in a model human arterial network: assessment of 1-D numerical simulations against in vitro measurements. J Biomech 40:3476–3486
Müller L, Toro E (2014a) Enhanced global mathematical model for studying cerebral venous blood flow. J Biomech 47:3361–3372
Müller L, Toro E (2014b) A global multiscale mathematical model for the human circulation with emphasis on the venous system. Int J Numer Methods Biomed Eng 30:681–725
Müller L, Blanco P, Watanabe S, Feijóo R (2016) A high-order local time stepping finite volume solver for one-dimensional blood flow simulations: application to the ADAN model. Int J Numer Methods Biomed Eng 32(e02):761
Mynard J, Nithiarasu P (2008) A 1d arterial blood flow model incorporating ventricular pressure, aortic valve and regional coronary flow using the locally conservative Galerkin (LCG) method. Commun Numer Methods 24:367–417
Mynard J, Smolich J (2015) One-dimensional haemodynamic modeling and wave dynamics in the entire adult circulation. Ann Biomed Eng 43:1443–1460
Mynard J, Davidson M, Penny D, Smolich J (2012) Non-linear separation of pressure, velocity and wave intensity into forward and backward components. Med Biol Eng Comput 50:641–648
Netter F (2011) Atlas of human anatomy, 5th edn. Elsevier, Amsterdam
Olufsen M, Peskin C, Kim W, Pedersen E, Nadim A, Larsen J (2000) Numerical simulation and experimental validation of blood flow in arteries with structured-tree outflow conditions. Ann Biomed Eng 28:1281–1299
Osada T, Murase N, Kime R, Shiroishi K, Shimomura K, Nagata H, Katsumura T (2007) Arterial blood flow of all abdominal-pelvic organs using Doppler ultrasound: range, variability and physiological impact. Physiol Meas 28(10):1303–1316
O’Rourke M, Hashimoto J (2007) Mechanical factors in arterial aging: a clinical perspective. J Am Coll Cardiol 50:1–13
Ouriel K, Greenberg R, Sarac T (2001) Hemodynamic conditions at the carotid bifurcation during protective common carotid occlusion. J Vasc Surg 34:577–580
Ozbek S, Killi AMR, Pourbagher M, Demirpolat G, Oran I, Pourbagher A (1998) Carotid steal: report of ten cases. J Ultrasound Med 17:623–629
Perdikaris P, Grinberg L, Karniadakis GE (2015) An effective fractal-tree closure model for simulating blood flow in large arterial networks. Ann Biomed Eng 43(6):1432–1442
Ramsey MW, Sugawara M (1997) Arterial wave intensity and ventriculoarterial interaction. Heart Vessels Suppl 12:128–134
Reymond P, Merenda F, Perren F, Rüfenacht D, Stergiopulos N (2009) Validation of a one-dimensional model of the systemic arterial tree. Am J Physiol Heart Circ Physiol 297:H208–H222
Safaei S, Bradley CP, Suresh V, Mithraratne K, Muller A, Ho H, Ladd D, Hellevik LR, Omholt SW, Chase JG, Müller LO, Watanabe SM, Blanco PJ, de Bono B, Hunter PJ (2016) Roadmap for cardiovascular circulation model: roadmap for cardiovascular circulation model. J Physiol 594:6909–6928
Safaei S, Blanco PJ, Müller LO, Hellevik LR, Hunter PJ (2018) Bond graph model of cerebral circulation: toward clinically feasible systemic blood flow simulations. Front Physiol 9:148
Sato K, Ogoh S, Hirasawa A, Oue A, Sadamoto T (2011) The distribution of blood flow in the carotid and vertebral arteries during dynamic exercise in humans. J Physiol 589(11):2847–2856
Segers P, Stergiopulos N, Verdonck P, Westerhof N (2001) Mathematical model analysis of heart-arterial interaction in hypertension. In: 2001 conference proceedings of the 23rd annual international conference of the IEEE engineering in medicine and biology society, vol 1, pp 192–195
Stergiopulos N, Young D, Rogge T (1992) Computer simulation of arterial flow with applications to arterial and aortic stenoses. J Biomech 25:1477–1488
Tindall G, Odom G, Dillon M Jr, Cupp HB Jr, Mahaley MS Jr, Greenfield JC Jr (1963) Direction of blood flow in the internal and external carotid arteries following occlusion of the ipsilateral common carotid artery. Observation in 19 patients. J Neurosurg 20:985–994
Toole J, McGraw C (1975) The steal syndromes. Ann Rev Med 26:321–329
Urquiza S, Desimone H, Goñi M, Introzzi A, Clara F (1995) Prediction of human arterial pulse wave shape changes in aging and hypertension. In: Power H, Hart RT, Hosoda S et al (eds) Computer simulations in biomedicine. Milan, Italy, pp 131–138
Wang J, Parker K (2004) Wave propagation in a model of the arterial circulation. J Biomech 37:457–470
Weizsacker H, Pinto J (1988) Isotropy and anisotropy of the arterial wall. J Biomech 21:477–487
Acknowledgements
This work was partially supported by the Brazilian agencies CNPq (465586/2014-7, 407751/2018-1) and FAPERJ (E26-203.283/2016). The support of these agencies is gratefully acknowledged.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Blanco, P.J., Müller, L.O., Watanabe, S.M. et al. On the anatomical definition of arterial networks in blood flow simulations: comparison of detailed and simplified models. Biomech Model Mechanobiol 19, 1663–1678 (2020). https://doi.org/10.1007/s10237-020-01298-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10237-020-01298-4