Abstract
Femoropopliteal artery (FPA) mechanics play a paramount role in pathophysiology and the artery’s response to therapeutic interventions, but data on FPA mechanical properties are scarce. Our goal was to characterize human FPAs over a wide population to derive a constitutive description of FPA aging to be used for computational modeling. Fresh human FPA specimens (\(n=579\)) were obtained from \(n=351\) predominantly male (80 %) donors 54±15 years old (range 13–82 years). Morphometric characteristics including radius, wall thickness, opening angle, and longitudinal pre-stretch were recorded. Arteries were subjected to multi-ratio planar biaxial extension to determine constitutive parameters for an invariant-based model accounting for the passive contributions of ground substance, elastin, collagen, and smooth muscle. Nonparametric bootstrapping was used to determine unique sets of material parameters that were used to derive age-group-specific characteristics. Physiologic stress–stretch state was calculated to capture changes with aging. Morphometric and constitutive parameters were derived for seven age groups. Vessel radius, wall thickness, and circumferential opening angle increased with aging, while longitudinal pre-stretch decreased (\(p<0.01\)). Age-group-specific constitutive parameters portrayed orthotropic FPA stiffening, especially in the longitudinal direction. Structural changes in artery wall elastin were associated with reduction of physiologic longitudinal and circumferential stretches and stresses with age. These data and the constitutive description of FPA aging shed new light on our understanding of peripheral arterial disease pathophysiology and arterial aging. Application of this knowledge might improve patient selection for specific treatment modalities in personalized, precision medicine algorithms and could assist in device development for treatment of peripheral artery disease.







Similar content being viewed by others
References
Adam DJ, Beard JD, Cleveland T et al (2005) Bypass versus angioplasty in severe ischaemia of the leg (BASIL): multicentre, randomised controlled trial. Lancet 366:1925–1934. doi:10.1016/S0140-6736(05)67704-5
Baek S, Gleason RL, Rajagopal KR, Humphrey JD (2007) Theory of small on large: potential utility in computations of fluid-solid interactions in arteries. Comput Methods Appl Mech Eng 196:3070–3078. doi:10.1016/j.cma.2006.06.018
Benetos A, Laurent S, Hoeks AP (1993) Arterial alterations with aging and high blood pressure. A noninvasive study of carotid and femoral arteries. Arterioscler Thromb Vasc Biol 13:90–97. doi:10.1161/01.ATV.13.1.90
Bortolotto LA, Hanon O, Franconi G et al (1999) The aging process modifies the distensibility of elastic but not muscular arteries. Hypertension 34:889–892. doi:10.1161/01.HYP.34.4.889
Brandfonbrener M, Landowne M, Shock NW (1955) Changes in cardiac output with age. Circulation 12:557–566. doi:10.1161/01.CIR.12.4.557
Conte MS, Bandyk DF, Clowes AW et al (2006) Results of PREVENT III: a multicenter, randomized trial of edifoligide for the prevention of vein graft failure in lower extremity bypass surgery. J Vasc Surg 43:742–751. doi:10.1016/j.jvs.2005.12.058
Ferruzzi J, Vorp DA, Humphrey JD (2011) On constitutive descriptors of the biaxial mechanical behaviour of human abdominal aorta and aneurysms. J R Soc Interface 8:435–450
Gasser TC, Ogden RW, Holzapfel G (2006) Hyperelastic modeling of arterial layers with distributed collagen fibre orientations. J R Soc Interface 3:15–35. doi:10.1098/rsif.2005.0073
Greenwald S (2007) Ageing of the conduit arteries. J Pathol 211:157–172. doi:10.1002/path
Holzapfel GA, Ogden RW (2010) Modelling the layer-specific three-dimensional residual stresses in arteries, with an application to the human aorta. J R Soc Interface 7:787–799
Holzapfel GA, Gasser TC, Ogden RW et al (2000) A new constitutive framework for arterial wall mechanics and a comparative study of material models. J Elast 61:1–48
Holzapfel GA, Sommer G, Auer M et al (2007) Layer-specific 3D residual deformations of human aortas with non-atherosclerotic intimal thickening. Ann Biomed Eng 35:530–545
Horny L, Adamek T, Zitny R (2012) Age-related changes in longitudinal prestress in human abdominal aorta. Arch Appl Mech 83:875–888. doi:10.1007/s00419-012-0723-4
Horný L, Netušil M, Voňavková T (2013) Axial prestretch and circumferential distensibility in biomechanics of abdominal aorta. Biomech Model Mechanobiol. doi:10.1007/s10237-013-0534-8
Horný L, Adámek T, Kulvajtová M (2016) A comparison of age-related changes in axial prestretch in human carotid arteries and in human abdominal aorta. Biomech Model Mechanobiol. doi:10.1007/s10237-016-0797-y
Humphrey JD (2002) Cardiovascular solid mechanics: cells, tissues, and organs. Springer
Humphrey JD (2008) Vascular adaptation and mechanical homeostasis at tissue, cellular, and sub-cellular levels. Cell Biochem Biophys 50:53–78. doi:10.1007/s12013-007-9002-3
Humphrey JD, Eberth JF, Dye WW, Gleason RL (2009) Fundamental role of axial stress in compensatory adaptations by arteries. J Biomech 42:1–8. doi:10.1016/j.jbiomech.2008.11.011.Fundamental
Iida O, Nanto S, Uematsu M et al (2006) Effect of exercise on frequency of stent fracture in the superficial femoral artery. Am J Cardiol 98:272–274
Intengan HD, Schiffrin EL (2001) Vascular remodeling in hypertension: roles of apoptosis, inflammation, and fIbrosis. Hypertension 38:581–587
Jani B, Rajkumar C (2006) Ageing and vascular ageing. Postgrad Med J 82:357–362. doi:10.1136/pgmj.2005.036053
Kamenskiy AV, Pipinos II, Carson JS et al (2014) Age and disease-related geometric and structural remodeling of the carotid artery. J Vasc Surg. doi:10.1016/j.jvs.2014.10.041
Kamenskiy AV, Pipinos II, Dzenis YA et al (2014b) Passive biaxial mechanical properties and in vivo axial pre-stretch of the diseased human femoropopliteal and tibial arteries. Acta Biomater 10:1301–1313. doi:10.1016/j.actbio.2013.12.027
Kamenskiy A, Dzenis Y, Kazmi SAJ et al (2014c) Biaxial mechanical properties of the human thoracic and abdominal aorta, common carotid, subclavian, renal and common Iliac arteries. Biomech Model Mechanobiol 13:1341–1359. doi:10.1007/s10237-014-0576-6
Kamenskiy AV, Pipinos II, Dzenis Ya et al (2015) Effects of age on the physiological and mechanical characteristics of human femoropopliteal arteries. Acta Biomater 11:304–313. doi:10.1016/j.actbio.2014.09.050
Kamenskiy A, Seas A, Bowen G et al (2016) In situ longitudinal pre-stretch in the human femoropopliteal artery. Acta Biomater 32:231–237. doi:10.1016/j.actbio.2016.01.002
Lakatta EG, Wang M, Najjar SS (2009) Arterial aging and subclinical arterial disease are fundamentally intertwined at macroscopic and molecular levels. Med Clin North Am 93:583–604. doi:10.1016/j.mcna.2009.02.008
Learoyd BM, Taylor MG (1966) Alterations with age in the viscoelastic properties of human arterial walls. Circ Res 18:278–292. doi:10.1161/01.RES.18.3.278
Lee H-Y, Oh B-H (2010) Aging and arterial stiffness. Circ J 74:2257–2262. doi:10.1253/circj.CJ-10-0910
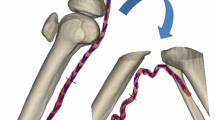
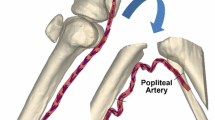
MacTaggart J, Phillips N, Lomneth C et al (2014) Three-dimensional bending, torsion and axial compression of the femoropopliteal artery during limb flexion. J Biomech 47:2249–2256
Mahoney EM, Wang K, Cohen DJ et al (2008) One-year costs in patients with a history of or at risk for atherothrombosis in the United States. Circ Cardiovasc Qual Outcomes 1:38–45. doi:10.1161/CIRCOUTCOMES.108.775247
Matsumoto T, Tsuchida M, Sato M (1996) Change in intramural strain distribution in rat aorta due to smooth muscle contraction and relaxation. Am J Physiol Soc H1711–1716
Mithieux SM, Weiss AS (2005) Elastin. Adv Protein Chem 70:437–461. doi:10.1016/S0065-3233(05)70013-9
Mozaffarian D, Benjamin EJ, Go AS, et al (2015) Heart disease and stroke statistics—2016 update: a report from the American Heart Association
O’Rourke MF (2007) Arterial aging: pathophysiological principles. Vasc Med 12:329–341. doi:10.1177/1358863X07083392
Qiu J, Zheng Y, Hu J et al (2014) Biomechanical regulation of vascular smooth muscle cell functions: from in vitro to in vivo understanding. J R Soc Interface 11:20130852. doi:10.1098/rsif.2013.0852
Schillinger M, Sabeti S, Loewe C (2006) Balloon angioplasty versus implantation of nitinol stents in the superficial femoral artery. N Engl J Med 354:1879–1888
Schillinger M, Sabeti S, Dick P et al (2007) Sustained benefit at 2 years of primary femoropopliteal stenting compared with balloon angioplasty with optional stenting. Circulation 115:2745–2749. doi:10.1161/CIRCULATIONAHA.107.688341
Siracuse JJ, Giles Ka, Pomposelli FB et al (2012) Results for primary bypass versus primary angioplasty/stent for intermittent claudication due to superficial femoral artery occlusive disease. J Vasc Surg 55:1001–1007. doi:10.1016/j.jvs.2011.10.128
Sommer G (2008) Mechanical properties of healthy and diseased human arteries. TU Graz
Stonebridge PA, Brophy CM (1991) Spiral laminar flow in arteries? Lancet 338:1360–1361
Ueno H, Kanellakis P, Agrotis a, Bobik a (2000) Blood flow regulates the development of vascular hypertrophy, smooth muscle cell proliferation, and endothelial cell nitric oxide synthase in hypertension. Hypertension 36:89–96. doi:10.1161/01.HYP.36.1.89
Acknowledgments
Research reported in this publication was supported in part by the National Heart, Lung, And Blood Institute of the National Institutes of Health under Award Numbers R01 HL125736 and F32 HL124905. The authors also wish to acknowledge the Nebraska Organ Recovery System (NORS), the Charles and Mary Heider Fund for Excellence in Vascular Surgery, and the MARC U*STAR Program for their help and support.
Funding This study was supported in part by the National Heart, Lung, And Blood Institute of the National Institutes of Health under Award Numbers R01 HL125736 and F32 HL124905.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Alexey Kamenskiy and Andreas Seas have contributed equally.
Rights and permissions
About this article
Cite this article
Kamenskiy, A., Seas, A., Deegan, P. et al. Constitutive description of human femoropopliteal artery aging. Biomech Model Mechanobiol 16, 681–692 (2017). https://doi.org/10.1007/s10237-016-0845-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10237-016-0845-7