Abstract
This study examines the changes in marginal revenue during psychiatric inpatient stays in a large Swiss psychiatric hospital after the introduction of a mixed reimbursement system with tariff rates that vary over length of stay. A discrete time duration model with a difference-in-difference specification and time-varying coefficients is estimated to assess variations in policy effects over length of stay. Among patients whose costs are fully reimbursed by the mixed scheme, the model demonstrates a significant effect of marginal revenue on length of stay. No significant policy effects are found among patients for whom only health insurance rates are delivered as mixed tariffs and government contributions are made retrospectively. The results indicate that marginal revenue can affect length of stay in inpatient psychiatry facilities, but that the reduction in marginal revenue must be sufficiently large.




Similar content being viewed by others
Notes
Between 2008 and 2011, the following cantons had reimbursement agreements with the canton of Zurich that allowed their residents to be treated in Zurich hospitals: Appenzell-Innerhoden, Appenzell-Auserrhoden, Glarus, Graubünden, St. Gallen, Schaffhausen, Thurgau, and Zug. Patients from other cantons or from abroad had to pay the government share themselves.
According to staff of the health administration of the canton of Zurich the intervention hospital was selected because it was a state run hospital and because it treated a typical patient population. The comparison group also included state-run hospitals.
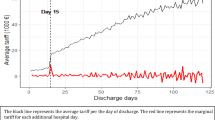
As an example, a stay of 20 days in the intervention hospital was reimbursed by health insurance with \(20 \times 309=6180\) in 2008, and \(3062 + 5 \times 356 + 15 \times 217 = 8097\) in 2009.
An episode of a non-Zurich resident of 36 days was reimbursed by health insurance and the government with \(36\times 803=28{,}908\) in 2008, and with \(7720 + 5\times 897 + 31 \times 546 = 29{,}131\) in 2009. The revenue from health insurance for a stay of a Zurich resident of 40 days was \(40 \times 309 = 12{,}360\) in 2008, and \(3062 + 5 \times 356 + 35 \times 217 = 12{,}437\) in 2009.
The CGI rating is an overall assessment of symptom severity by the treating physician; its scores range from 1 (normal, not at all ill) to 7 (extremely ill).
References
Ashcraft, M.L.F., Fries, B.E., Nerenz, D.R., Falcon, S., Srivastava, S.V., Lee, C.Z., Berki, S.E., Errera, P.: A psychiatric patient classification system: an alternative to diagnosis-related groups. Med. Care 27(5), 543–557 (1989)
Siegel, C., Alexander, M.J., Lin, S., Laska, E.: An alternative to drugs: a clinically meaningful and cost-reducing approach. Med. Care 24(5), 407–417 (1986)
Warnke, I., Rössler, W., Herwig, U.: Does psychopathology at admission predict the length of inpatient stay in psychiatry? Implications for financing psychiatric services. BMC Psychiatry 11(1), 120 (2011)
Hunter, C.E., McFarlane, A.C.: DRGs and Australian psychiatry. Aust. N. Z. J. Psychiatry 28(1), 114–120 (1994)
Taube, C., Lee, E.S., Forthofer, R.N.: Drgs in psychiatry: an empirical evaluation. Med. Care 22(7), 597–610 (1984)
Drozd, E., Cromwell, J., Gage, B., Maier, J., Greenwald, L., Goldman, H.: Patient casemix classification for medicare psychiatric prospective payment. Am. J. Psychiatry 163(4), 724–732 (2006)
Chalkley, M., Malcomson, J.M.: Government purchasing of health services. In: Culyer AJ, Newhouse JP (eds) Handbook of Health Economics, vol. 1, chap. 15, pp. 847–890. Elsevier, Amsterdam (2000)
Frank, R.G., Lave, J.R.: A comparison of hospital responses to reimbursement policies for medicaid psychiatric patients. Rand J. Econ. 20(4), 588–600 (1989)
Freiman, M.P., Ellis, R.P., McGuire, T.G.: Provider response to medicare’s PPS: reductions in length of stay for psychiatric patients treated in scatter beds. Inquiry 26, 192–201 (1989)
Ellis, R.P., McGuire, T.G.: Hospital response to prospective payment: moral hazard, selection, and practice-style effects. J. Health Econ. 15(3), 257–277 (1996)
Dranove, D., White, W.D.: Recent theory and evidence on competition in hospital markets. J. Econ. Manag. Strategy 3(1), 169–209 (1994)
Norton, E.C., Van Houtven, C.H., Lindrooth, R.C., Normand, S.L.T., Dickey, B.: Does prospective payment reduce inpatient length of stay? Health Econ. 11(5), 377–387 (2002)
Cutler, D.M.: The incidence of adverse medical outcomes under prospective payment. Econom. J. Econom. Soc. 63(1), 29–50 (1995)
Ellis, R.P., McGuire, T.G.: Provider behavior under prospective reimbursement: Cost sharing and supply. J. Health Econ. 5(2), 129–151 (1986)
Ellis, R.P., McGuire, T.G.: Optimal payment systems for health services. J. Health Econ. 9(4), 375–396 (1990)
McGuire, T.G.: Physician agency and payment for primary medical care. In: Glied, S., Smith, P.C. (eds.) The Oxford Handbook of Health Economics, chap. 25, pp. 602–623. Oxford University Press Inc., New York
Singer, J.D., Willett, J.B.: It’s about time: using discrete-time survival analysis to study duration and the timing of events. J. Educ. Stat. 18(2), 155–195. ISSN 03629791 (1993)
Beck, N., Katz, J.N., Tucker, R.: Taking time seriously: time-series-cross-section analysis with a binary dependent variable. Am. J. Polit. Sci. 42(4), 1260–1288 (1998)
Kalbfleisch, J., Prentice, R.: The statistical analysis of failure time data. In: Applied Probability and Statistics. Wiley Series in Probability and Mathematical Statistics. Wiley, New York (2002). ISBN: 9780471055198
Allison, P.D.: Discrete-time methods for the analysis of event histories. Sociolog. Methodol. 13, 61–98 (1982). ISSN: 00811750
Ai, C., Norton, E.C.: Interaction terms in logit and probit models. Econ. Lett. 80(1), 123–129 (2003)
Puhani, P.A.: The treatment effect, the cross difference, and the interaction term in nonlinear difference-in-differences models. Econ. Lett. 115(1), 85–87 (2012)
Lancaster, T.: The econometric analysis of transition data. In: Econometric Society Monographs. Cambridge University Press, Cambridge (1992). ISBN: 9780521437899
Acknowledgments
I am very grateful to Claude Jeanrenaud, Per Johansson, and Simon Wieser for their support and guidance. Carsten Colombier, Peter Zweifel, Maarten Lindeboom, Jürgen Maurer, Alberto Holly, Mark Dusheiko, and other participants of the Swiss Health Economics Workshop and the SSPH+ PhD seminar provided useful comments. I also thank the two anonymous reviewers whose comments helped improve and clarify this manuscript. All errors are my own.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
There are no current external funding sources for this study.
Conflict of interest
The author declares that there are no conflicts of interest.
Rights and permissions
About this article
Cite this article
Pletscher, M. Marginal revenue and length of stay in inpatient psychiatry. Eur J Health Econ 17, 897–910 (2016). https://doi.org/10.1007/s10198-015-0735-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10198-015-0735-4