Abstract
Objective
The planning of health care management benefits from understanding future trends in demand and costs. In the case of lung diseases in the national German hospital market, we therefore analyze the current structure of care, and forecast future trends in key process indicators.
Methods
We use standardized, patient-level, activity-based costing from a national cost calculation data set of respiratory cases, representing 11.9–14.1 % of all cases in the major diagnostic category “respiratory system” from 2006 to 2012. To forecast hospital admissions, length of stay (LOS), and costs, the best adjusted models out of possible autoregressive integrated moving average models and exponential smoothing models are used.
Results
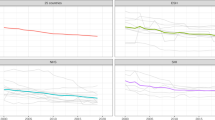
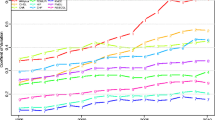
The number of cases is predicted to increase substantially, from 1.1 million in 2006 to 1.5 million in 2018 (+2.7 % each year). LOS is expected to decrease from 7.9 to 6.1 days, and overall costs to increase from 2.7 to 4.5 billion euros (+4.3 % each year). Except for lung cancer (−2.3 % each year), costs for all respiratory disease areas increase: surgical interventions +9.2 % each year, COPD +3.9 %, bronchitis and asthma +1.7 %, infections +2.0 %, respiratory failure +2.6 %, and other diagnoses +8.5 % each year. The share of costs of surgical interventions in all costs of respiratory cases increases from 17.8 % in 2006 to 30.8 % in 2018.
Conclusions
Overall costs are expected to increase particularly because of an increasing share of expensive surgical interventions and rare diseases, and because of higher intensive care, operating room, and diagnostics and therapy costs.

Similar content being viewed by others
References
Halbert, R.J., Natoli, J.L., Gano, A., Badamgarav, E., Buist, A.S., Mannino, D.M.: Global burden of COPD: systematic review and meta-analysis. Eur Respir J 28(3), 523–532 (2006). doi:10.1183/09031936.06.00124605
Buist, A.S., McBurnie, M.A., Vollmer, W.M., Gillespie, S., Burney, P., Mannino, D.M., Menezes, A.M., Sullivan, S.D., Lee, T.A., Weiss, K.B., Jensen, R.L., Marks, G.B., Gulsvik, A., Nizankowska-Mogilnicka, E.: International variation in the prevalence of COPD (the BOLD Study): a population-based prevalence study. Lancet 370(9589), 741–750 (2007). doi:10.1016/s0140-6736(07)61377-4
Braman, S.S.: The global burden of asthma. Chest 130(1 Suppl), 4s–12s (2006). doi:10.1378/chest.130.1_suppl.4S
Mannino, D.M., Buist, A.S.: Global burden of COPD: risk factors, prevalence, and future trends. Lancet 370(9589), 765–773 (2007). doi:10.1016/s0140-6736(07)61380-4
Waatevik, M., Skorge, T.D., Omenaas, E., Bakke, P.S., Gulsvik, A., Johannessen, A.: Increased prevalence of chronic obstructive pulmonary disease in a general population. Respir Med 107(7), 1037–1045 (2013). doi:10.1016/j.rmed.2013.04.008
Bahadori, K., Doyle-Waters, M.M., Marra, C., Lynd, L., Alasaly, K., Swiston, J., FitzGerald, J.M.: Economic burden of asthma: a systematic review. BMC Pulm Med 9(1), 24 (2009). doi:10.1186/1471-2466-9-24
D’Souza, A.O., Shah, M., Dhamane, A.D., Dalal, A.A.: Clinical and economic burden of COPD in a Medicaid population. COPD 11(2), 212–220 (2014). doi:10.3109/15412555.2013.836168
Andersen, H., Lampela, P., Nevanlinna, A., Saynajakangas, O., Keistinen, T.: High hospital burden in overlap syndrome of asthma and COPD. Clin Respir J 7(4), 342–346 (2013). doi:10.1111/crj.12013
Eurostat: Hospital discharges by diagnosis, in-patients, total number (hlth_co_disch1) (2014). http://epp.eurostat.ec.europa.eu/portal/page/portal/statistics/search_database. Accessed 9 Nov 2014
Statistisches Bundesamt [The Federal Statistical Office]: Fallpauschalenbezogene Krankenhausstatistik, Fachserie 12 Reihe 6.4 (2013). https://www.destatis.de/DE/Publikationen/Thematisch/Gesundheit/Krankenhaeuser/FallpauschalenKrankenhaus.html. Accessed 9 Nov 2014
European Respiratory Society: European Lung White Book (2013). http://www.erswhitebook.org/chapters/the-burden-of-lung-disease/. Accessed 9 Nov 2014
Ford, E.S.: Hospital discharges, readmissions, and emergency department visits for chronic obstructive pulmonary disease or bronchiectasis among US adults: findings from the Nationwide Inpatient Sample 2001–2012 and Nationwide Emergency Department Sample 2006–2011. Chest (2014). doi:10.1378/chest.14-2146
Lorenzoni, L., Belloni, A., Sassi, F.: Health-care expenditure and health policy in the USA versus other high-spending OECD countries. Lancet 384(9937), 83–92 (2014). doi:10.1016/s0140-6736(14)60571-7
Schulz, E., Leidl, R., Konig, H.H.: The impact of ageing on hospital care and long-term care–the example of Germany. Health Policy Amst Neth 67(1), 57–74 (2004)
Strunk, B.C., Ginsburg, P.B., Banker, M.I.: The effect of population aging on future hospital demand. Health Aff Proj Hope 25(3), w141–w149 (2006). doi:10.1377/hlthaff.25.w141
Stark, D., Mould, D., Schweikert, A.: 5 steps to creating a forecast. J Healthc Financ Manag Assoc 62(4), 100–105 (2008)
Institute for the Hospital Remuneration System (InEK): G-DRG Report-Browser (2014). http://www.g-drg.de/cms/Archiv. Accessed 9 Nov 2014
Vogl, M.: Assessing DRG cost accounting with respect to resource allocation and tariff calculation: the case of Germany. Health Econ Rev 2(1), 15 (2012). doi:10.1186/2191-1991-2-15
Vogl, M.: Improving patient-level costing in the English and the German ‘DRG’ system. Health Policy 109(3), 290–300 (2013)
Vogl, M.: Hospital financing: calculating inpatient capital costs in Germany with a comparative view on operating costs and the English costing scheme. Health Policy 115(2–3), 141–151 (2014). doi:10.1016/j.healthpol.2014.01.013
Kaplan, R.S., Anderson, S.R.: Time-driven activity-based costing: a simpler and more powerful path to higher profits. Harvard Business Press, Boston (2007)
Schreyogg, J., Tiemann, O., Busse, R.: Cost accounting to determine prices: how well do prices reflect costs in the German DRG-system? Health care Manag Sci 9(3), 269–279 (2006)
Institut für das Entgeltsystem im Krankenhaus (InEK): Abschlussbericht zur Weiterentwicklung des G-DRG System für das Jahr 2011. http://www.g-drg.de/cms/Archiv (2011). Accessed 19 Mar 2015
Kimberly, J.R., de Pouvourville, G., D’Aunno, T.: The globalization of managerial innovation in health care. Cambridge University Press, Cambridge (2009)
Busse, R., Geissler, A., Quentin, W., Wiley, M.W.: Diagnosis-related groups in Europe: moving towards transparency, efficiency and quality in hospitals. McGraw-Hill, Open University Press, New York (2011)
Massacci, D.: Predicting the distribution of stock returns: model formulation, statistical evaluation, VaR analysis and economic significance. J Forecast 34(3), 191–208 (2015). doi:10.1002/for.2332
Wohlrabe, K., Buchen, T.: Assessing the macroeconomic forecasting performance of boosting: evidence for the United States, the Euro area and Germany. J Forecast 33(4), 231–242 (2014). doi:10.1002/for.2293
Jones, S.S., Thomas, A., Evans, R.S., Welch, S.J., Haug, P.J., Snow, G.L.: Forecasting daily patient volumes in the emergency department. Acad Emerg Med: Off J Soc Acad Emerg Med 15(2), 159–170 (2008). doi:10.1111/j.1553-2712.2007.00032.x
Hoot, N.R., Epstein, S.K., Allen, T.L., Jones, S.S., Baumlin, K.M., Chawla, N., Lee, A.T., Pines, J.M., Klair, A.K., Gordon, B.D., Flottemesch, T.J., LeBlanc, L.J., Jones, I., Levin, S.R., Zhou, C., Gadd, C.S., Aronsky, D.: Forecasting emergency department crowding: an external, multicenter evaluation. Ann Emerg Med 54(4), 514–522.e519 (2009). doi:10.1016/j.annemergmed.2009.06.006
Boyle, J., Jessup, M., Crilly, J., Green, D., Lind, J., Wallis, M., Miller, P., Fitzgerald, G.: Predicting emergency department admissions. Emerg Med J EMJ 29(5), 358–365 (2012). doi:10.1136/emj.2010.103531
Koestler, D.C., Ombao, H., Bender, J.: Ensemble-based methods for forecasting census in hospital units. BMC Med Res Methodol 13, 67 (2013). doi:10.1186/1471-2288-13-67
Limb, M.: Hospitals forecast a rise in emergency admissions, while commissioners forecast a fall. BMJ Clin Res Ed 349, g4699 (2014). doi:10.1136/bmj.g4699
Heidenreich, P.A., Trogdon, J.G., Khavjou, O.A., Butler, J., Dracup, K., Ezekowitz, M.D., Finkelstein, E.A., Hong, Y., Johnston, S.C., Khera, A., Lloyd-Jones, D.M., Nelson, S.A., Nichol, G., Orenstein, D., Wilson, P.W., Woo, Y.J.: Forecasting the future of cardiovascular disease in the United States: a policy statement from the American Heart Association. Circulation 123(8), 933–944 (2011). doi:10.1161/CIR.0b013e31820a55f5
Soyiri, I.N., Reidpath, D.D.: Evolving forecasting classifications and applications in health forecasting. Int J Gen Med 5, 381–389 (2012). doi:10.2147/ijgm.s31079
Soyiri, I.N., Reidpath, D.D.: An overview of health forecasting. Environ Health Prev Med 18(1), 1–9 (2013). doi:10.1007/s12199-012-0294-6
Cote, M.J., Tucker, S.L.: Four methodologies to improve healthcare demand forecasting. J Healthc Financ Manag Assoc 55(5), 54–58 (2001)
Box, G.E.P., Jenkins, G.M., Reinsel, G.C.: Time series analysis: forecasting and control, 4th edn. Wiley, New Jersey (2008)
Gardner, E.S.: Exponential smoothing: the state of the art. J Forecast 4(1), 1–28 (1985)
Hyndman, R.J., Athanasopoulos, G.: Forecasting: principles and practice (2013). https://www.otexts.org/book/fpp. Accessed 19 Nov 2014
Billah, B., King, M.L., Snyder, R.D., Koehler, A.B.: Exponential smoothing model selection for forecasting. Int J Forecast 22(2), 239–247 (2006)
Gardner, E.S., Dannenbring, D.G.: Forecasting with exponential smoothing: some guidelines for model selection. Decis Sci 11(2), 370–383 (1980)
Statistisches Bundesamt [The Federal Statistical Office]: Verbraucherpreisindizes [consumer price index] (2014). https://www.destatis.de/DE/ZahlenFakten/GesamtwirtschaftUmwelt/Preise/Verbraucherpreisindizes/Verbraucherpreisindizes.html. Accessed 19 Nov 2014
Samet, J.M., Avila-Tang, E., Boffetta, P., Hannan, L.M., Olivo-Marston, S., Thun, M.J., Rudin, C.M.: Lung cancer in never smokers: clinical epidemiology and environmental risk factors. Clin Cancer Res Off J Am Assoc Cancer Res 15(18), 5626–5645 (2009). doi:10.1158/1078-0432.ccr-09-0376
Lamprecht, B., McBurnie, M.A., Vollmer, W.M., Gudmundsson, G., Welte, T., Nizankowska-Mogilnicka, E., Studnicka, M., Bateman, E., Anto, J.M., Burney, P., Mannino, D.M., Buist, S.A.: COPD in never smokers: results from the population-based burden of obstructive lung disease study. Chest 139(4), 752–763 (2011). doi:10.1378/chest.10-1253
Deutsche Gesellschaft für Gesundheitsökonomie: Perspectives of reforming hospital financing in Germany [in German]. Gesundheitsökonomie und Qualitätsmanagement 19(6), 248–249 (2014)
Appleby, J.: Do we have too many hospitals? BMJ Clin Res Ed. 348, (2014). doi:10.1136/bmj.g1374
Pokhrel, S., Evers, S., Leidl, R., Trapero-Bertran, M., Kalo, Z., Vries, H., Crossfield, A., Andrews, F., Rutter, A., Coyle, K., Lester-George, A., West, R., Owen, L., Jones, T., Vogl, M., Radu-Loghin, C., Voko, Z., Huic, M., Coyle, D.: EQUIPT: protocol of a comparative effectiveness research study evaluating cross-context transferability of economic evidence on tobacco control. BMJ open 4(11), e006945 (2014). doi:10.1136/bmjopen-2014-006945
Conflict of interest
The authors declare that they have no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Vogl, M., Leidl, R. Informing management on the future structure of hospital care: an extrapolation of trends in demand and costs in lung diseases. Eur J Health Econ 17, 505–517 (2016). https://doi.org/10.1007/s10198-015-0699-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10198-015-0699-4