Abstract
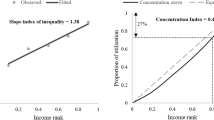
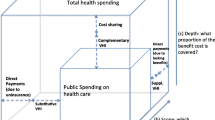
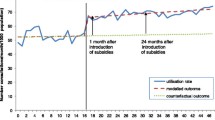
This article reviews the quantitative evidence on the behavioural effects of copayment within the health area across a wide range of countries. The review distinguishes itself from previous similar reviews by having a high degree of transparency for the search strategy used to identify the studies included in the review as well as the criteria for inclusion and by including the most recent literature. Empirical studies were identified by performing searches in EconLit. The literature search identified a total of 47 studies of the behavioural effects of copayment. Considering the demand effects, the majority of the reviewed studies found that copayment reduces the use of prescription medicine, consultations with general practitioners and specialists, and ambulatory care, respectively. The literature found no significant effects of copayment on the prevalence of hospitalisations. The empirical evidence on whether copayment for some services, but not for others, causes substitution from the services that are subject to copayment to the ‘free’ services rather than lower total use is sparse and mixed. Likewise, the health effects of copayment have only been analysed empirically in a limited number of studies, of which half did not find any significant effects in the short term. Finally, the empirical evidence on the distributional consequences of copayment indicates that individuals with low income and in particular need of care generally reduce their use relatively more than the remaining population in consequence of copayment. Hence, it is clear that copayment involves some important economic and political trade-offs.
Similar content being viewed by others
Notes
Given that demand is approximated by actual use in all of the reviewed studies, the terms demand and use are applied interchangeably throughout the article.
Examples of health care services for which the price elasticity of demand is most likely limited are chemotherapy, bypass operations and other major interventions, which may be lifesaving but pose considerable health risks in themselves.
For example, it is possible that increased copayment for prescription medicine reduces the demand for general practice consultations, which often result in a prescription.
Master Theses are not systematically available from all institutes and faculties and are therefore not included.
A review of the empirical literature on the consequences of different types of copayment within the pharmaceutical area found that indirect copayment has the ability to shift use from expensive to cheaper types of medicine, although often with modest savings in consequence [5].
See Atherly [20] for a review of effect studies for the elderly in the US, for whom variation in the level of copayment is mainly cause by voluntary purchase of supplementary private health insurance and Kiil [21] for an overview of effect studies of voluntary private health insurance in universal health care systems.
* Indicates a truncated search, i.e. a search on the stem of the word as well as its different endings.
Relevant employees at a number of Danish research institutions, ministries and interest groups were also contacted in order to ensure that all relevant literature was included. However, this did not result in the identification of additional studies.
In consequence of the rather general search terms used, the main reason that many studies were classified as being irrelevant and discarded was that they dealt with something else than copayment. More specific groups of discarded studies include studies that investigate effects of supply-side payment systems, studies based on data collected prior to 1990, studies of indirect copayment, and studies that identified the effect of copayment by using variation in copayment rates between individuals who have voluntarily selected themselves into different schemes or purchased complementary private health insurance.
Some of the more recent working papers may reasonably be expected to be published in article format at a later point in time.
Specifically, while there is an upper limit for the total earnings of doctors, they are allowed to exceed the threshold with income stemming from copayment. This structure may unintentionally have created an incentive for the doctors to seek to increase the visit rate among the patients who are required to copay in order to increase total earnings.
Cockx and Brasseur [30] adjust the estimates reported in van de Voorde et al. [62] by taking into account that the increases in the relative copayments for the three types of doctor visits considered were not proportional and decomposing the demand effect into an income effect and a substitution effect.
The authors note that the fact that general practitioners receive a fixed fee for patients aged 70 and above creates an incentive for the general practitioners to seek to limit the number of visits for this patient group.
With the exception of Puig-Junoy et al. [53].
References
Rovira, J., et al.: Comparing cost-sharing in European Union member states: a system-oriented framework. In: Leidl, R. (ed.) Health Care and Its Financing in the Single European Market, pp. 183–211. IOS Press, Amsterdam (1998)
Hansen, S.W., Houlberg, K.: Brugerbetaling på sundheds- og ældreområdet i komparativt perspektiv. AKF, Copenhagen (2012)
Gibson, T.B., Ozminkowski, R.J., Goetzel, R.Z.: The effects of prescription drug cost sharing: a review of the evidence. Am. J. Manag. Care 11, 730–740 (2005)
Goldman, D.P., Joyce, G.F., Zheng, Y.: Prescription drug cost sharing. Associations with medication and medical utilization and spending and health. J. Am. Med. Assoc. 298(1), 61–69 (2007)
Gemmill, M.C., Thomson, S., Mossialos, E.: What impact do prescription drug charges have on efficiency and equity? Evidence from high-income countries. Int. J. Equity Health 7(12), (2008)
Lexchin, J., Grootendorst, P.: Effects of prescription drug user fees on drug and health services use and on health status in vulnerable populations: a systematic review of the evidence. Int. J. Health Serv. 34(1), 101–122 (2004)
Carrieri, V.: The effects of cost-sharing in health care: what do we know from empirical evidence? Economia politica. J. Anal. Inst. Econ. 2, 351–374 (2010)
Holst, J.: Patient Cost Sharing—Reforms without Evidence, pp. 1–146. Social Science Research Centre, Berlin (2010)
Swartz, K.: Cost-sharing: effects on spending and outcomes. In: The Synthesis Project, pp. 1–36. Robert Wood Johnson Foundation (2010)
Rice, T., Matsuoka, K.Y.: The impact of cost-sharing on appropriate utilization and health status: a review of the literature on seniors. Med. Care Res. Rev. 61(4), 415–452 (2004)
Manning, W.G., et al.: Health insurance and the demand for medical care: evidence from a randomized experiment. Am. Econ. Rev. 77, 251–277 (1987)
Lohr, K.N., et al.: Use of medical care in the RAND health insurance experiment. Med. Care 24(9 Suppl), S1–S87 (1986)
Shapiro, M.F., Ware, J.E., Sherbourne, C.D.: Effects of cost sharing on seeking care for serious and minor symptoms. Results of a randomized controlled trial. Ann. Intern. Med. 104(2), 246–251 (1986)
Siu, A.L., et al.: Inappropriate use of hospitals in a randomized trial of health insurance plans. N. Engl. J. Med. 315, 1259–1266 (1986)
Brook, R.H., et al.: Does free care improve adults’ health? Results from a randomized controlled trial. N. Engl. J. Med. 309(23), 1426–1434 (1983)
Robinson, R.: User charges for health care. In: Mossialos, E., et al. (eds.) Funding Health Care: Options for Europe, pp. 161–183. Open University Press, London (2002)
Arrow, K.J.: Uncertainty and the welfare economics of medical care. Am. Econ. Rev. 53, 941–973 (1963)
Pauly, M.V.: The economics of moral hazard: comment. Am. Econ. Rev. 58, 531–537 (1968)
The World Bank: Country and Lending Groups. 2012 [cited 2012 27/2]. Available from: http://data.worldbank.org/about/country-classifications/country-and-lending-groups#High_income
Atherly, A.: Medicare’s accidental stepchild. Med. Care Res. Rev. 2, 131–161 (2001)
Kiil, A.: Does employment-based private health insurance increase the use of covered health care services? A matching estimator approach. Int. J. Health Care Financ. Econ. 12(1), 1–38 (2012)
Almarsdóttir, A.B., Morgall, J.M., Grimsson, A.: Cost containment of pharmaceutical use in Iceland: the impact of liberalisation and user charges. J. Health Serv. Res. Policy 5(2), 109–113 (2000)
Atella, V., et al.: Drug compliance, co-payment and health outcomes: evidence from a panel of Italian patients. Health Econ. 15, 875–892 (2006)
Augurzky, B., Bauer, T.K., Schaffner, S.: Copayments in the German Health System: Does It Work? in IZA Discussion Paper No. 2290 (2006)
Blais, L., et al.: Impact of a cost sharing drug insurance plan on drug utilization among individuals receiving social assistance. Health Policy 64, 163–172 (2003)
Bolin, K., et al.: Utilisation of physician services in the 50+ population. The relative importance of individual versus institutional factors in 10 European countries. Int. J. Health Care Financ. Econ. 9(1), 83–112 (2009)
Cherkin, D.C., Grothaus, L., Wagner, E.H.: Is magnitude of co-payment effect related to income? Using census data for health services research. Soc. Sci. Med. 43(1), 33–41 (1992)
Christensen, B.: Characteristics of attenders and non-attenders at health examinations for ischaemic heart disease in general practice. Scand. J. Prim. Health Care 13, 26–31 (1995)
Christensen, B.: Payment and attendance at general practice preventive health examinations. Fam. Med. 27(8), 531–534 (1995)
Cockx, B., Brasseur, C.: The demand for physician services. Evidence from a natural experiment. J. Health Econ. 22, 881–913 (2003)
Contoyannis, P., et al.: Estimating the price elasticity of expenditure for prescription drugs in the presence of non-linear price schedules: an illustration from Quebec. Can. Health Econ. 14, 909–923 (2005)
Costa-Font, J., Kanavos, P., Rovira, J.: Determinants of out-of-pocket pharmaceutical expenditure and access to drugs in Catalonia. Appl. Econ. 39(5), 541–551 (2007)
Elofsson, S., Undén, A.-L., Krakau, I.: Patient charges—a hindrance to financially and psychologically disadvantage groups seeking care. Soc. Sci. Med. 46(10), 1375–1380 (1998)
Fiorio, C.V., Siciliani, L.: Co-payments and the demand for pharmaceuticals: evidence from Italy. Econ. Model. 27, 835–841 (2010)
Grootendorst, P., Levine, M.: Do Drug Plans Matter? Effects of Drug Plan Eligibility on Drug Use Among the Elderly, Social Assistance Recipients and the General Population, in QSEP Research Report No. 372. McMaster University (2002)
Gundgaard, J.: Income-related inequality in utilization of health services in Denmark: evidence from Funen County. Scand. J. Public Health 34, 10 (2006)
Jordin, B., Engholm, G.: Besöksfrekvenser för unga och äldre efter införandet av avgiftsfrihet för patienter yngre än 20 år. Socialmedicinsk tidsskrift: Organ för sjuk- och hälsovård 1, 85–90 (2001)
Kim, J.Y., Ko, S.K., Yang, B.M.: The effects of patient cost sharing on ambulatory utilization in South Korea. Health Policy 72(3), 293–300 (2005)
Kupor, S.A., et al.: The effect of copayments and income on the utilization of medical care by subscribers to Japan’s National Health Insurance System. Int. J. Health Serv. 25(2), 295–312 (1995)
Krutilová, V.: Impact of user fees in health care system on health care consumption. Rev. Econ. Perspect. 10(4), 113–132 (2010)
Layte, R., et al.: Do consultation charges deter general practitioner use among older people? Soc. Sci. Med. 68, 1432–1438 (2009)
Li, X., et al.: The impact of cost sharing of prescription drug expenditures on health care utilization by the elderly: own- and cross-price elasticities. Health Policy 82, 340–347 (2007)
Lostao, L., et al.: Patient cost sharing and social inequalities in access to health care in three western European countries. Soc. Sci. Med. 65, 367–376 (2007)
Lostao, L., et al.: Patient cost sharing and physician visits by socioeconomic position: findings in three Western European countries. J. Epidemiol. Community Health 61(5), 416–420 (2007)
Lundberg, L., et al.: Effects of user charges on the use of prescription medicines in different socio-economic groups. Health Policy 44, 123–134 (1998)
McManus, P., et al.: Prescription drug utilization following patient co-payment changes in Australia. Pharmacoepidemiol. Drug Saf. 5, 385–392 (1996)
Nexøe, J., Kragstrup, J., Rønne, T.: Impact of postal invitations and user fee on influenza vaccination rates among the elderly. Scand. J. Prim. Health Care 15, 109–112 (1997)
Nolan, A.: Evaluating the impact of eligibility for free care on the use of general practitioner (GP) services: a difference-in-difference matching approach. Soc. Sci. Med. 67, 1164–1172 (2008)
O’Reilly, D., et al.: Consultation charges in Ireland deter a large proportion of patients from seeing the GP: results of a cross-sectional survey. Eur. J. Gen. Pract. 13, 231–236 (2007)
Or, Z., Jusot, F., Yilmaz, E.: Impact of Health Care System on Socioeconomic Inequalities in Doctor Use, in IRDES Working Paper No. 17, Paris (2008)
Pilote, L., et al.: The effects of cost-sharing on essential drug prescriptions, utilization of medical care and outcomes after acute myocardial infarction in elderly patients. Can. Med. Assoc. J. 167(3), 246–252 (2002)
Poirier, S., et al.: The effect of a $2 co-payment on prescription refill rates of quebec elderly and its relationship to socio-economic status. Can. Pharm. J. 130(10), 30–34 (1998)
Puig-Junoy, J., García-Gómez, P., Casado-Marín, D.: Free Medicines Thanks to Retirement: Moral Hazard and Hospitalization Offsets in an NHS, in Tintenberg Institute Discussion Paper 108/3 (2011)
Rosen, B., et al.: When co-payments for physician visits can affect supply as well as demand: findings from a natural experiment in Israel’s national health insurance system. Int. J. Health Plan. Manag. 26, e68–e84 (2011)
Rückert, I.-M., Böcken, J., Mielck, A.: Are German patients burdened by the practice charge for physician visits (‘Praxisgebuehr’)? A cross sectional analysis of socio-economic and health related factors. BMC Health Serv. Res. 8(232), 2008
Schreyögg, J., Grabka, M.M.: Copayments for Ambulatory Care in Germany: A Natural Experiment Using a Difference-in-Difference Approach, in SOEP Papers on Multidisciplinary Panel Data Research. DIW, Berlin (2008)
Scott, K.M., Marwick, J.C., Crampton, P.R.: Utilization of general practitioner services in New Zealand and its relationship with income, ethnicity and government subsidy. Health Serv. Manag. Res. 16(1), 45–55 (2003)
Simonsen, M., Skipper, L., Skipper, N.: Price Sensitivity of Demand for Prescription Drugs: Exploiting a Regression Kink Design, in Economics Working Paper. School of Economics and Management, Aarhus University (2010)
Skipper, N.: On Utilization and Stockpiling of Prescription Drugs when Co-payments Increase: Heterogeneity Across Types of Drugs, in Economics Working Paper. School of Economics and Management, Aarhus University (2010)
Street, A., Jones, A., Furuta, A.: Cost-sharing and pharmaceutical utilisation and expenditure in Russia. J. Health Econ. 18, 459–472 (1999)
Tamblyn, R., et al.: Adverse events associated with prescription drug cost-sharing among poor and elderly persons. J. Am. Med. Assoc. 285(4), 421–429 (2001)
van de Voorde, C., van Doorslaer, E., Schokkaert, E.: Effects of cost sharing on physician utilization under favourable conditions for supplier-induced demand. Health Econ. 10, 457–471 (2001)
van Doorslaer, E., et al.: The redistributive effect of health care finance in twelve OECD countries. J. Health Econ. 18, 291–313 (1999)
Wagstaff, A., et al.: Equity in the finance of health care: some further international comparisons. J. Health Econ. 18, 263–290 (1999)
Wang, P.S., et al.: Impact of drug cost sharing on service use and adverse clinical outcomes in elderly receiving antidepressants. J. Mental Health Policy Econ. 13(1), 37–44 (2010)
Winkelmann, R.: Co-payments for prescription drugs and the demand for doctor visits—evidence from a natural experiment. Health Econ. 13, 1081–1089 (2004)
Zápal, J.: Doctor-visit co-payment exemption for children: first look at the data. Czech J. Econ. Financ. 60(1), 58–72 (2010)
Zhong, H.: Equity in pharmaceutical utilization in Ontario: a cross-section and over time analysis. Can. Public Policy 33(4), 487–507 (2007)
Louckx, F.: Patient cost sharing and access to health care. In: Mackenbach, J., Bakker, M. (eds.) Reducing Inequalities in Health. A European Perspective, pp. 188–198. Routledge, London (2002)
Paulus, A., Sutherland, H., Tsakloglou, P.: The distributional impact of in-kind public benefits in European countries. J. Policy Anal. Manag. 29, 243–266 (2010)
Aaberge, R., et al.: The Distributional Impact of Public Services when Needs Differ, in IZA Discussion Paper No. 4826. Institute for the study of Labor, Bonn (2010)
Acknowledgments
The authors would like to thank research librarian Lisa la Cour for providing valuable guidance on how to search for literature and helping us collect the relevant studies and two anonymous reviewers for their helpful comments.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kiil, A., Houlberg, K. How does copayment for health care services affect demand, health and redistribution? A systematic review of the empirical evidence from 1990 to 2011. Eur J Health Econ 15, 813–828 (2014). https://doi.org/10.1007/s10198-013-0526-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10198-013-0526-8