Abstract
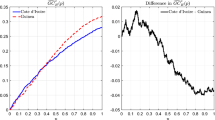
Using representative microdata from the German Socio-Economic Panel Study (SOEP), we show that the welfare measure choice has a substantial impact on the degree of welfare-related health inequality. To assess the sensitivity of welfare-related health inequality measures, we combine a unique set of income and wealth measures with different subjective, cardinalized, and (quasi-)objective health measures. The influence of the welfare measure is more pronounced when using subjective health measures than when using (quasi-)objective health measures.
We’re sorry, something doesn't seem to be working properly.
Please try refreshing the page. If that doesn't work, please contact support so we can address the problem.
Similar content being viewed by others
Notes
However, all correction methods do not derive a correction within a regression framework for the standard errors.
Since we use the 2006 (quasi-)objective health measures together with the 2007 wealth measures, a shift in the health distribution between 2006 an 2007 might contaminate our results. The same could be true for systematic health-related panel attrition. The SF12 and grip strength are surveyed every other year in the SOEP and the wealth measures every 5 years. Hence, as a robustness check, we performed the same analysis with the 2007 income and wealth and the 2008 (quasi-)objective health measures. The results are not sensitive and very stable. They are available upon request from the corresponding author.
We apply the modified OECD equivalence scale, which assigns a value of 1 to the household head, 0.5 to other adults, as well as 0.3 to children up to 14 years of age.
We decided to condition on the height and weight of the respondents, since it has been shown that both factors are correlated strongly with grip strength and thus physical health [13, 26]. Since physical health is also part of the overall health measures and for reasons of consistency, we have incorporated these variables throughout the analysis. However, one referee correctly pointed out that height and weight itself are health measures and thus potential outcome variables. Moreover, they are measured with error [29]. Likewise, one could argue that correlations of our health measures with labor market characteristics, education, and other socio-economic background characteristics should not be netted out prior to the main analysis. For example, health may affect the decision to work and, at the same time, employment itself may affect health [27]. Hence, we carried out exactly the same analysis as discussed below, but disregarded these variables, i.e., we indirectly standardized the health measures, but only with regard to gender and age. The results are very similar and robust, but almost all inequality measures increase slightly in size, i.e., welfare-related health inequality slightly decreases. This systematic shift does not affect our findings or conclusion. The results are available upon request from the corresponding author.
References
Abul-Naga, R., Yalcin, T.: Inequality measurement for ordered response health data. J. Health Econ. 27, 1614–1625 (2008)
Andersen, H.H., Mühlbacher, A., Nübling, M., Schupp, J., Wagner, G.G.: Computation of standard values for physical and mental health scale scores using the SOEP version of sf12v2. J. Appl. Soc. Sci. Stud. (Zeitschrift für Wirtschafts- und Sozialwissenschaften) 127, 171–182 (2007)
Bago d’Uva, T., O’Donnell, O., van Doorslaer, E.: Differential health reporting by education level and its impact on the measurement of health inequalities among older Europeans. Int. J. Epidemiol. 37, 1375–1383 (2008)
Burkhauser, R.V., Feng, S., Jenkins, S.P., Larrimore, J.: Estimating trends in US income inequality using the Current Population Survey: the importance of controlling for censoring. J. Econ. Inequal. 9, 393–415 (2011)
Danish Ministry of Health [Sundhedsministeriet]: The Government’s Public Health Programme 1999–2008 [Regeringens folkesundhedsprogram 1999–2008]. Danish Ministry of Health, Copenhagen (1999)
Erreygers, G.: Correcting the concentration index. J. Health Econ. 28, 504–515 (2009)
Erreygers, G.: Correcting the concentration index: a reply to Wagstaff. J. Health Econ. 28, 521–524 (2009)
Erreygers, G., van Ourti, T.: Putting the cart before the horse. A comment on Wagstaff on inequality measurement in the presence of binary variables. Health Econ. 20, 1161–1165 (2011)
Erreygers, G., van Ourti, T.: Measuring socioeconomic inequality in health, health care, and health financing by means of rank-dependent indices: a recipe for good practice. J. Health Econ. 30, 685–694 (2011)
Frick, J.R., Grabka, M.M., Sierminska, E.M.: Representative wealth data for Germany from the German SOEP: the impact of methodological decisions around imputation and the choice of the aggregation unit. SOEPpapers 3, DIW Berlin, The German Socio-Economic Panel (2007a). Available at: http://ideas.repec.org/p/diw/diwsop/diw_sp3.html. Last accessed on February 2, 2012
Frick, J.R., Grabka, M.M., Marcus, J.: Editing and multiple imputation of item-non-response in the 2002 wealth module of the German Socio-Economic Panel (SOEP). Data Documentation 18, DIW Berlin, German Institute for Economic Research (2007b). Available at: http://ideas.repec.org/p/diw/diwddc/dd18.html. Last accessed on February 2, 2012
Gakidou, E.E., Murray, C.J.L., Frenk, J.: Defining and measuring health inequality: an approach based on the distribution of health expectancy. Bull. World Health Organ. 78, 42–54 (2000)
Hank, K., Jürges, H., Schupp, J., Wagner, G.G.: Isometrische Greifkraft und sozialgerontologische Forschung: Ergebnisse und Analysepotentiale des SHARE und SOEP. Zeitschrift für Gerontologie und Geriatrie 42, 117–126 (2009)
House of Commons Health Committee: Health Inequalities: Third Report of Session 2008–2009. HMSO, London (2009)
Jones, A.M., Rice, N., d’Uva, T.B., Balia, S.: Applied Health Economics. Routledge, Abington (2007)
Jürges, H.: True health vs. response styles: exploring cross-country differences in self-reported health. Health Econ. 16, 163–178 (2007)
Jürges, H.: Health inequalities by education, income and wealth: a comparison of 11 European countries and the US. Appl. Econ. Lett. 17, 91–97 (2010)
Kakwani, N., Wagstaff, A., van Doorslaer, E.: Socioeconomic inequalities in health: measurement, computation, and statistical inference. J. Econ. 77, 87–103 (1997)
Lecluyse, A.: Income-related health inequality in Belgium: a longitudinal perspective. Eur. J. Health Econ. 8, 237–243 (2007)
Le Grand, J.: Inequality in health: some international comparisons. Eur. Econ. Rev. 31, 182–191 (1987)
Lindelow, M.: Sometimes more equal than others: how health inequalities depend on the choice of welfare indicator. Health Econ. 15, 263–279 (2006)
McGee, D.L., Liao, Y., Cao, G., Cooper, R.S.: Self-reported health status and mortality in a multiethnic US cohort. Am. J. Epidemiol. 149, 41–46 (1999)
O’Donnell, O., van Doorslaer, E., Wagstaff, A., Lindelow, M.: Analyzing Health Equity Using Household Survey Data: A Guide to Techniques and their Implementation. D.C., World Bank Publications, Washington (2007)
Hays, R.D., Sherbourne, C.D, Mazel, R., RAND: User’s Manual for the Medical Outcomes Study (MOS) Core Measures of Health-Related Quality of Life. RAND Monograph Report, Santa Monica, RAND Corporation (1995). Available at: http://www.rand.org/pubs/monograph_reports/MR162.html. Last accessed on February 2, 2012
Rantanen, T., Guralnik, J.M., Foley, D., Masaki, K., Leveille, S., Curb, J.D., White, L.: Midlife hand grip strength as a predictor of old age disability. J. Am. Med. Assoc. 281, 558–560 (1999)
Rantanen, T., Harris, T., Leveille, S.G., Visser, M., Foley, D., Masaki, K., Guralnik, J.M.: Muscle strength and body mass index as long-term predictors or mortality in initially healthy men. J. Gerontol. Med. Sci. 55A, M168–M173 (2000)
Schmitz, H.: Why are the unemployed in worse health? The causal effect of unemployment on health. Labour Econ. 18, 71–78 (2011)
Schneider, U., Pfarr, C., Schneider, B.S., Ulrich, V.: I feel good! Gender differences and reporting heterogeneity in self-assessed health. Eur. J. Health Econ. (2012). doi: 10.1007/s10198-011-0301-7
Sturm, R.: The effects of obesity, smoking, and drinking on medical problems and costs. Health Aff. 21, 245–253 (2002)
Tubeuf, S., Jusot, F.: Social health inequalities among older Europeans: the contribution of social and family background. Eur. J. Health Econ. 12, 61–77 (2011)
Wagner, G.G., Frick, J.R., Schupp, J.: The German Socio-Economic Panel Study (SOEP)–evolution, scope and enhancements. J. Appl. Soc. Sci. Stud. (Schmollers Jahrbuch) 127, 139–169 (2007)
Wagstaff, A.: The bounds of the Concentration Index when the variable of interest is binary, with an application to immunization inequality. Health Econ. 14, 429–432 (2005)
Wagstaff, A.: The bounds of the Concentration Index when the variable of interest is binary, with an application to immunization inequality. J. Health Econ. 28, 516–520 (2009)
Wagstaff, A.: The Concentration Index of a binary outcome revisited. Health Econ. 20, 1155–1160 (2011)
Wagstaff, A.: Reply to Guido Erreygers and Tom van Ourti’s comment on “The Concentration Index of a binary outcome revisited”. Health Econ. 20, 1166–1168 (2011)
Wagstaff, A., Wantanabe, N.: What difference does the choice of SES make in health inequality measurement? Health Econ. 12, 885–890 (2003)
Wolff, E.N., Zacharias, A.: Household wealth and the measurement of economic well-being in the United States. J. Econ. Inequal. 7, 83–115 (2009)
World Health Organization (WHO): The World Health Report 2000-Health Systems: Improving Performance. World Health Organization (WHO), Geneva (2000)
van Doorslaer, E., Jones, A.M.: Inequalities in self-reported health: validation of a new approach to measurement. J. Health Econ. 22, 61–87 (2003)
Zheng, B.: A new approach to measure socioeconomic inequality in health. J. Econ. Inequal. 9, 555–577 (2011)
Zhong, H.: The impact of missing data in the estimation of concentration index: a potential source of bias. Eur. J. Health Econ. 11, 255–266 (2010)
Ziebarth, N.R.: Measurement of health, health inequality, and reporting heterogeneity. Soc. Sci. Med. 71, 116–124 (2010)
Acknowledgments
We thank the editor, two anonymous referees, Cristina Blanco, Andrew Jones, Martin Karlsson, Jenny Kragl, Tom van Ourti, and participants at seminars in Darmstadt at the “Health. Happiness. Inequality–Modelling the Pathways between Income Inequality and Health” conference, as well as in Rome at the Meeting of the Applied Econometrics Association and the “Econometrics of Healthy Human Resources.” Special thanks go to Adam Lederer for co-editing this paper.
Author information
Authors and Affiliations
Corresponding author
Additional information
Joachim R. Frick: Deceased.
In December 2011, after having bravely fought for more than one year against an extremely virulent form of cancer, Joachim R. Frick—my co-author on this manuscript—passed away. Joachim was more than just a mentor and advisor to me. I first met Joachim in July 2004. At that time, I was a Master’s student at the Berlin Institute of Technology (TU Berlin). In collaboration with the SOEP department at DIW Berlin, Joachim offered a course on how to work with SOEP data and with Stata®. This was the first time that I actually worked with microdata and I realized that research was what I wanted to do in the future. Joachim shaped the course of my life ever since. Without taking this course and without Joachim’s encouragement to apply I would never earned my PhD from TU Berlin and DIW Berlin. As I reflect back, and as I find my place in the academy, I am sure that without Joachim I would not be where I am now and would not be doing what I do now. Thanks Joachim, I will never forget. Rest in peace.
Appendix
Appendix
See Table 4.
Rights and permissions
About this article
Cite this article
Frick, J.R., Ziebarth, N.R. Welfare-related health inequality: does the choice of measure matter?. Eur J Health Econ 14, 431–442 (2013). https://doi.org/10.1007/s10198-012-0387-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10198-012-0387-6