Abstract
Background
An earlier study showed that from a societal perspective it was less expensive to encourage patients to self-regulate their medication for GERD (gastro-esophageal reflux disease) by treating patients on-demand.
Objective
The objective was to investigate whether physician involvement in a clinical trial financed by the pharmaceutical industry subsequently results in higher health care costs.
Study design
An open, observational, multicenter study compared direct medical costs and total costs for three groups of patients with different exposure to the clinical trial; (1) Dual exposed, where both the patients and the GP participated in the former clinical trial, (2) GP exposed, where only the GP participated in the former clinical trial and (3) nonexposed, where neither the patients nor the GP participated in the former clinical trial.
Results
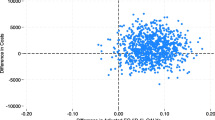
We did not find any statistically significant differences in neither direct medical nor total costs. However, we did observe a numerical difference in direct medical costs of 24% higher in the dual exposed group compared to the nonexposed group mainly due to a higher consumption of prescribed medication. The higher direct medical cost in the dual exposed group was however counterbalanced by lower observed direct nonmedical and indirect costs.
Conclusion
Although we did not find any statistical significant differences in health care costs, we did observe a higher consumption of prescribed medication and lower costs of work hours lost if both patient and GPs participated in a former clinical trial. The results may be limited due to a lower number of patients included than expected.


Similar content being viewed by others
Notes
From now on referred to as “the former clinical trial”.
The study assessed differences in direct medical costs and total costs for 3 different esomeprazole treatment strategies: On-demand treatment (patient controlled), Intermittent 2 weeks treatment (GP controlled) and Intermittent 4 weeks treatment (GP controlled).
.
See Table 1 for the kind of cost data included in the analysis.
Reasons for exclusion: Less than 3 days of symptoms (6), history of disease, that should exclude patient (13), did not use effective contraception (12) other reasons (8).
References
Meineche-Schmidt, V., Hauschildt Juhl, H., Østergaard, J.E., Luckow, A., Hvenegaard, A.: Costs and efficacy of three different esomeprazole treatment strategies for long-tern management of gastro-oesophageal reflux symptoms in primary care. Aliment. Pharmacol. Ther. 19, 907–915 (2004)
Meineche-Schmidt, V., Hvenegaard, A., Hauschildt Juhl, H.: Participation in a clinical trial influences the future management of patients. Aliment. Pharmacol. Ther. 24(7), 1117–1125 (2006)
Pieters, T.: Marketing medicines through randomised controlled trials: the case of interferons. BMJ 317(7167), 1231–1233 (1998)
Influence of pharmaceutical companies on prescribing (2001), Link to PDF: http://www.ukmicentral.nhs.uk/therapeu/sthderpres/2001_08.pdf Retrieved 13-10-2006
Pena E.: The Value of Phase IV. PharmaVoice (December): 1–9 (2003)
McGettigan, P., Golden, J., Fryer, J., Chan, R., Feely, J.: Prescribers prefer people: The sources of information used by doctors for prescribing suggest that the medium is more important than the message. Br. J. Clin. Pharmacol. 51(2), 184–189 (2001)
Prosser, H., Almond, S., Walley, T.: Influences on GP’s decision to prescribe new drugs-the importance of who says what. Fam. Pract. 20(1), 61–68 (2003)
Robertson, J., Treloar, C.J., Sprogis, A., Henry, D.A.: The influence of specialists on prescribing by GPs. A qualitative study. Aust. Fam. Phys. 32(7), 573–576 (2003)
Jones, M.I., Greenfield, S.M., Bradley, C.P.: Prescribing new drugs: qualitative study of influences on consultants and general practitioners. BMJ 323(7309), 378–381 (2001)
Stevenson, F.A., Greenfield, S.M., Jones, M., Nayak, A., Bradley, C.P.: GP’s perceptions of patient influence on prescribing. Fam. Pract. 16(3), 255–261 (1999)
Wazana, A.: Physicians and the pharmaceutical industry: is a gift ever just a gift? JAMA 283, 373–380 (2000)
Chren, M.M., Landefeld, C.S.: Physician’s behavior and their interactions with drug companies: a controlled study of physicians who requested additions to a hospital drug formulary. JAMA 271, 684–689 (1994)
Lurie, N., Rich, E.C., Simpson, D.E., Meyer, J., Schiedermayer, D.L., Goodman, J.L., et al.: Pharmaceutical representatives in academic medical centers. interaction with faculty and housestaff. J. Gen. Intern. Med. 5, 240–243 (1990)
Denig, P., Haaijer-Ruskamp, F.M., Wesseling, H., Versluis, A.: Impact of clinical trials on the adoption of new drugs within a university hospital. Eur. J. Clin. Pharmacol. 41, 325–328 (1991)
Andersen, M., Kragstrup, J., Søndergaard, J.: How conducting a clinical trial affects physician’s guideline adherence and drug preferences. JAMA 295(23), 2759–2764 (2006)
Pollock, K., Grime, J.: Strategies for reducing the prescribing of proton pump inhibitors (PPIs): patient self-regulation of treatment may be an under-exploited resource. Soc. Sci. Med. 51(12), 1827–1839 (2000)
Armstrong, D., Reyburn, H., Jones, R.: A study of general practitioner’s reasons for changing their prescribing behaviour. BMJ 312(7036), 949–952 (1996)
Hart, J., Salman, H., Bergman, M., Neuman, V., Rudniki, C., Gilenberg, D., et al.: Do drug costs affect physician’s prescription decisions? J. Intern. Med. 241(5), 415–420 (1997)
Madridejos Mora, R., mado Guirado, E., Perez Rodriguez, M.T.: Effectiveness of the combination of feedback and educational recommendations for improving drug prescription in general practice. Med. Care 42(7), 643–648 (2004)
Reichert, S., Simon, T., Halm, E.A.: Physician’s attitudes about prescribing and knowledge of the costs of common medications. Arch. Intern. Med. 160(18), 2799–2803 (2000)
Tamblyn, R., McLeod, P., Hanley, J.A., Girard, N., Hurley, J.: Physician and practice characteristics associated with the early utilization of new prescription drugs. Med. Care 41(8), 895–908 (2003)
Personal communication with vice-president Stig Waldorf, AstraZeneca Denmark (2005)
Acknowledgments
AstraZeneca, Denmark has supported the study financially.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hvenegaard, A., Juhl, H.H. & Habicht, A. Does participation in clinical trials influence the costs of future management of patients?. Eur J Health Econ 13, 569–574 (2012). https://doi.org/10.1007/s10198-011-0359-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10198-011-0359-2