Abstract
Symptomatic osteoarthritis (OA) of the knee develops often in association with anterior cruciate ligament (ACL) deficiency. Two distinct pathologies should be recognised while considering treatment options in patients with end-stage medial compartment OA and ACL deficiency. Patients with primary ACL deficiency (usually traumatic ACL rupture) can develop secondary OA (typically presenting with symptoms of instability and pain) and these patients are typically young and active. Patients with primary end stage medial compartment OA can develop secondary ACL deficiency (usually degenerate ACL rupture) and these patients tend to be older. Treatment options in either of these patient groups include arthroscopic debridement, reconstruction of the ACL, high tibial osteotomy (HTO) with or without ACL reconstruction, unicompartmental knee arthroplasty (UKA) and total knee arthroplasty (TKA). General opinion is that a functionally intact ACL is a fundamental prerequisite to perform a UKA. This is because previous reports showed higher failure rates when ACL was deficient, probably secondary to wear and tibial loosening. Nevertheless in some cases of ACL deficiency with end-stage medial compartment OA, UKA has been performed in isolation and recent papers confirm good short- to mid-term outcome without increased risk of implant failure. Shorter hospital stay, fewer blood transfusions, faster recovery and significantly lower risk of developing major complications like death, myocardial infarction, stroke, deep vein thrombosis (as compared to TKA) make the UKA an attractive option, especially in the older patients. On the other hand, younger patients with higher functional demands are likely to benefit from a simultaneous or staged ACL reconstruction in addition to UKA to regain knee stability. These procedures tend to be technically demanding. The main aim of this review was to provide a synopsis of the existing literature and outline an evidence-based treatment algorithm.
Similar content being viewed by others
Introduction
Few rules are known in medicine, but one of these assumes that unicompartmental knee arthroplasty (UKA) for medial osteoarthritis (MOA) is contraindicated if anterior cruciate ligament (ACL) is functionally deficient.
This has been generally accepted since the first reports highlighted a higher incidence of complications, in terms of tibial loosening and higher revision rate, when UKA were performed in ACL-deficient knees [9, 11].
Primary MOA in an ACL-intact knee usually involves the antero-medial aspect of the inner compartment and is therefore called antero-medial osteoarthritis. The preserved postero-medial compartment maintains a functional medial collateral ligament (MCL) [25] as every time the knee flexes, the femur rides out of the tibial defect allowing the MCL to regain its normal length. In such knees, with the passage of time, if the antero-medial OA is not treated, the wear patch on the medial tibial plateau extends posteriorly, the ACL progressively becomes damaged, typically from notch osteophytes, and eventually ruptures. These patients typically exhibit a more extensive wear pattern involving also the posterior aspect of the medial compartment [27]. In patients with primary ACL damage and secondary knee OA due to repeated episodes of anterior subluxation of the tibia in respect of the femur, the tibial wear patch is typically postero-medial, allowing normal antero-medial cartilage (Fig. 1). Every time the patient moves his/her knee, the femur rides free of the defect and corrects the varus deformity, thereby maintaining the normal length and functionality of the MCL.
Typical indications for UKA are a stable knee, functionally intact lateral and femoro-patellar compartments, correctable (intra-articular) varus deformity, less than 10°–15° of fixed flexion deformity, and flexion beyond 100°. Outside these indications, typically a patient should be offered a total knee arthroplasty (TKA). If usual indications are applied, UKA guarantees several advantages over TKA, in terms of better range of motion, less soft tissue damage allowing early and rapid recovery, preservation of bone stock, minimal blood loss, lower complication rates (including significantly reduced risks of stroke, heart attack, death or venous thromboembolism) and preservation of normal kinematic function. Furthermore, with an intact ACL, many series have shown that Oxford medial unicompartmental knee arthroplasty achieved survival rates of more than 90 % at 10 and 15 years, irrespective of patient’s age or activity level. In addition, the wear rates of an Oxford UKA are significantly lower than those of fixed bearing UKA or TKA due to its unique design characteristics of a fully congruous mobile bearing UKA maximising the contact area and minimising the contact stresses throughout the arc of knee flexion [19, 26].
These are the key reasons for UKA to be a preferred and appealing treatment option for either young and/or active patient or more elderly patient with significant co-morbidities even if ACL is deficient. TKA may represent a suboptimal option in terms of implant longevity in the former group and in terms of comorbidities in the latter.
Indications
Indications for UKA are based primarily on patho-anatomy rather than patient characteristics. Any patient with anteromedial OA and bone-on-bone arthritis with intact lateral cartilage (Fig. 2) and correctable varus deformity are ideal candidates for UKA, provided the ACL is intact or is reconstructed. If partial thickness lesions are present, especially in a malaligned knee, high tibial osteotomy (HTO) may become the preferred treatment of choice.
However, when approaching a patient with MOA in ACL-deficient knees, the main features to take into account are patient’s biological age, functional demands and primary symptom.
Age and functional activity play a significant role in our decision regarding whether to reconstruct the ACL or not. Elderly patients with lower functional requests, may benefit from the UKA without ACL reconstruction. On the other hand, in younger patients with isolated MOA, an ACL reconstruction, regaining stability in their knee, is preferred.
In the subjective evaluation of these patients, mechanical pain is usually present due to the MOA, eventually associated with a swollen knee. On the other hand, instability, even if ACL is deficient, may not be referred as a main symptom, probably because of the muscular status, the functional requests or the presence of posterior osteophytes [18] and capsule stiffness, which contribute to knee stability. In those patients, ACL reconstruction may not be performed to avoid further surgical steps and increasing arthrofibrosis risk. Considering the ACL-deficient knee, it is important to identify those without functional impairment and instability, known as “copers”, who are able to resume pre-injury activity level without the need for ACL reconstruction [14]. According to those assumptions a treatment algorithm may be drawn (Fig. 3).
Lower limb alignment is an important factor to consider in the assessment of a painful MOA knee, independently of ACL status. In the presence of extra-articular deformity, and initial-to-moderate OA, HTO would be the treatment of choice to correct the varus malalignment, thus restoring a neutral mechanical axis and reducing pressures on cartilage defects [12]. In contrast, a well aligned knee is better approached with a UKA, because its main aim is to restore the ligament to normal rather than to correct limb alignment without altering the physiological joint line [10].
If these considerations are accepted as a general rule, challenges may arise in the management of patients with malalignment and advanced disease, and patients with normal alignment but early partial thickness disease. The former group may benefit from a TKA rather than an HTO as their results in advanced OA are known to be poor [7]. In young patients, however, HTO is still an option to delay more invasive procedures like arthroplasties, even if symptoms relief may be partial. On the other hand, patients with good alignment and partial thickness disease should be not approached with an HTO to avoid unphysiological alteration of the joint line. UKA would also not be appropriate because, in the setting of partial thickness disease, results are worse than with bone on bone arthritis, and post-operative outcomes are less predictable [22].
Technical features
Nowadays UKA is a well standardised operation but performing it in ACL-deficient knees adds uncertainty about whether the ACL should be reconstructed or not.
ACL reconstruction can be performed simultaneously or in a staged procedure. Combined UKA and ACL reconstruction (Fig. 4) becomes a longer and more technical demanding procedure but avoids the need for a re-operation, with one more anaesthesia, longer recovery time and higher social costs. A staged procedure starting with ACL reconstruction may be indicated if instability is the main symptom, proceeding with the UKA only if pain arises later.
The surgical technique has been described by different authors [6, 21, 31, 33]. One key technical aspect is to avoid impingement of the graft tunnel on the tibial component of the UKA [15], and a second key aspect is to tension the graft properly. In addition, it is also possible that one may weaken the tibial plateau, leading to an additional risk of tibial fracture. Therefore, the advice is to perform the tibial tunnel slightly more laterally than usual [31] and/or in a more vertical direction to reduce the medial stress/impingement (Fig. 5). If cementless implants are used, the tibial tunnel should be drilled after positioning of the tibial component to lower the risk of fracture during tibial implant application. There is no clear evidence for this suggestion although it is intuitive to do so. After drilling the femoral tunnel and fixing the femoral end of the ACL graft, one can complete the implantation of the UKA. Finally, the tibial end of the graft can be fixed at the end of the procedure to achieve the right tension.
The choice of graft is not clearly stated in the literature [21]. Mainly bone-patellar tendon-bone (BPTB) and hamstring autografts are used but other options described include the use of allografts and synthetic implants. For the one-stage procedure, our opinion is to favour a bone-tendon-bone graft rather than a hamstring graft because it provides stronger initial fixation (bone to bone rather than bone to tendon), and the tibial tunnel can be drilled through the donor site in the tibial tubercle and so slightly lateralised, as previously mentioned. The medial third of the patellar tendon may be harvested through the traditional UKA approach, thus reducing the operative morbidity of the traditional middle third, which may lead to devascularisation of the remaining medial portion of the patellar tendon [15].
Tibial slope modification has been reported to play a role in ACL strain and knee stability. Opening and closing wedge osteotomies, increasing [3, 17] and decreasing [13] the posterior slope, respectively, have an effect on knee stability if performed in ACL-deficient patients. In the same way, tibial tray slope may be modified in UKA to reduce anterior tibial translation in ACL-deficient knees, as reported by Suero et al. [28] in a cadaveric study with fixed bearing UKA in non-weight bearing conditions. They showed an anterior tibial translation of about 5 mm, close to the intact knee, during a Lachman test with an 8° levelling of the posterior tibial slope. However, rotational stability during a pivot shift test was not influenced by slope modifications [28]. The role of tibial slope was confirmed also in a retrospective clinical paper by Hernigou and Deschamps [11]. This latter study found an increase in aseptic loosening rate if slope was more than 7° with a fixed bearing UKA, thus recommending not to exceed this limit [11].
The choice between mobile and fixed bearing depends partially on the surgeon’s preference. The potential for accelerated polyethylene wear, when performing an ACL-deficient UKA, is one of the main concerns that frighten surgeons. Fixed bearings are usually flatter, allowing a sliding motion of the femoral condyle. On the other hand, mobile bearings present a sliding motion on their inferior aspect over the tibial tray while a rolling motion of the femoral component is expected on the congruent superior surface. In laboratory evaluation, Blunn et al. [1] found a dramatically increased polyethylene wear with cyclic sliding compared with compression or rolling because of increased subsurface shear stresses, concluding that low-conformity components (i.e. fixed bearings) inserted with high ligamentous laxity are susceptible to antero-posterior sliding and hence high wear [1].
Table 1 reports survival rates of UKA by bearing type, obtained by pooling data from published papers about UKA in ACL-deficient knees. Although clinical outcomes are fairly similar, ACL reconstruction with fixed bearing seems to be the best choice in terms of survival rates, failures and revisions/100 observed years, although it is impossible to draw definitive conclusions due to the relatively short follow up period (65 months) and the small size of the population involved (262 knees). One can expect that mobile bearing is at risk of instability or dislocation but, according to these data, only two cases are reported, one each in the ACL-deficient and ACL reconstructed groups.
One more concern is the definition of intact ACL. Pre-operative assessment performed by clinical test and/or MRI study can under- or over-estimate the prevalence of ACL lesion. The presence of bone deformities, osteophytes or soft tissue contracture may alter the perception of antero-posterior laxity [2]. Our preferred option is intra-operative assessment under direct visualisation. We use a tendon hook and pass it around the native ACL and give a hard pull. If the ligament gets pulled off then clearly the ACL was deficient but if it does not then it is considered functionally intact. We have used this criterion for the last 35 years and have not found any reasons/evidence to change our practice. It is possible that an anatomically intact ACL has already lost its functional role due to degenerative changes in the microstructure, as has been reported by Trompeter et al. [32], who showed that greater than two out of three ACLs found to be macroscopically normal during TKA present moderate-to-severe disease at microscopic assessment.
Results
Biomechanical studies
An in vitro robotic studies by Suggs showed that knee stability is not altered by a medial fixed bearing UKA but they conclude that ACL is essential to avoid greater anterior tibial translation [29]. Their findings on similar ACL forces in the native knee and following UKA led to the conclusion that ACL also plays a role in the latter condition. Of course this is true assuming that UKA is well balanced with equal flexion and extension gaps, otherwise it may happen that ACL loses its physiological strain, thus rendering it non-functional. Citak et al. [5] demonstrated restored knee kinematics after performing a combined ACL reconstruction and fixed bearing UKA on cadaver specimens. In particular, there was no significant difference in lateral compartment translation during the Lachman and pivot shift tests between the ACL-intact UKA and the ACL-reconstructed UKA.
In vivo knee kinematics studies have also been performed, analyzing patellar tendon angle (PTA) in the sagittal plane (Fig. 6) as a marker of knee kinematics during high demand exercises between full extension and flexion [23]. PTA is a good measure of both patello-femoral and tibio-femoral joint kinematics, and is related to both the patella-femoral and the tibio-femoral contact forces. Major abnormalities in the PTA are likely to be a result of abnormalities in the relationship of the femur to the tibia. Anterior subluxation of the femur increases the angle, whereas posterior subluxation decreases it. Pandit et al. [23] found that normal kinematics is restored in vivo after ACL reconstruction in UKA, even if a slight anterior tibial (or posterior femoral, considering a closed chain exercise) displacement persists. This may determine similar components loading and, eventually, similar long-term survival. In ACL-deficient knees Pegg et al. [24] showed different knee kinematics between ACL-deficient and ACL-intact patients after UKA, particularly noticeable during the step-up between 30° and 60° of flexion, with a decrease in PTA in the ACL-deficient group. Overall, the kinematics of the ACL-deficient knees seemed to be more physiological than data reported for TKA, but not as close to healthy knees as ACL-reconstructed UKA knees.
Clinical studies
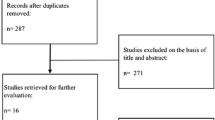
Several clinical studies have reported UKA results in ACL-deficient patient, combined [6, 15, 31, 33, 34] or not [2, 8, 9, 11] with ACL reconstruction stage. Demographic data are reported in Table 2.
Pre-operative pain was described as the usual symptom leading to UKA in ACL-reconstructed patients, along with instability, although the latter was not clearly quantified by the authors of the papers cited.
Table 2 shows that, in patients with ACL deficiency and OA, reconstruction of the ACL was performed in patients who were significantly younger as compared to those in whom it was not performed (mean age 50 vs 66 years). This finding is likely due to the lower demand in older patients, who may cope better with instability, or indeed may be affected by a more severe pattern of arthritis, with stiffness and osteophytes contributing to stability [4].
Raw survival rates, failures, revisions, complications and re-operations per observed years are reported in Table 3. Analysing failures and revisions per 100 observed years allows a comparison across studies with different follow up periods, but it is limited by the assumption that the distribution of complications is linear over time.
Complications
According to a recently published systematic review [16], complications are considered as any deviation from the expected post-operative course, both operative and non-operative. Failures were defined as any event resulting in further surgery in which a component was changed, a new component was added or where bearing dislocation had occurred in the case of UKA [20], and any traumatic graft rupture for ACL reconstructions [30]. Any operation where the patient underwent further surgery requiring the removal and/or exchange of any material implanted during the index operation was considered as a revision.
UKA ACL-deficient studies showed 19 failures in 154 followed patients [12.3 %; 4 progression of lateral OA (Fig. 7), 1 painful joint replacement, 12 tibia loosening, 1 bearing instability, 1 not specified], all of which required revision (12.3 %; 10 conversions to TKA, 1 arthrodesis, 1 conversion to bi-unicompartmental arthroplasty, 7 not specified). No further complications were reported in the above mentioned group.
In UKA ACL-reconstructed papers, involving 108 patients, in addition to 3 failures (2.8 %; 1 progression of lateral OA, 1 peri-prosthetic infection, 1 bearing dislocation), all of which required revision (2.8 %; 1 conversions to TKA, 1 two-stage revision to TKA, 1 bearing substitution), 4 complications (3.7 %; 1 lateral meniscal tear, 2 stiffness, 1 loose body), managed with a re-operation (3.7 %; 3 arthroscopies, 1 manipulation under anaesthesia) were reported [16].
Patients without ACL reconstruction, compared to patients with the combined procedure, have a significantly higher failure rate (by a factor of two), with a revision rate of 1.92 % at 10 years with, as would be expected, mobile bearing UKAs having a higher revision rate than fixed bearing UKA.
Tibial component loosening is the most frequently reported reason for failure in ACL-deficient knees, especially in the oldest series from Goodfellow (Oxford, mobile bearing) and Hernigou (Lotus, fixed bearing) [9, 11]. This trend has changed in the most recent studies, which showed improved survival rates with fewer revisions per 100 observed years (1 revision per 100 observed years in recent studies vs 3.33 in the oldest series) [2, 8], with one series reporting no evidence of loosening and equivalent patient recorded outcomes to patients with an intact ACL [2].
Different clinical scores were used in the various studies, and thus it was not possible to pool them. Clinical scores data are reported in Table 4.
Conclusions
In conclusion, ACL reconstruction and UKA is our preferred treatment option for patients with ACL deficiency and bone-on-bone medial compartment arthritis, particularly in the young and active. In the elderly, isolated UKA without ACL reconstruction seems to be a reasonable and attractive option if careful patient selection is performed. The absence of clinical pre-operative instability seems to have an important prognostic role in terms of functional results, especially if ACL reconstruction is not performed with the UKA. Simultaneous or staged ACL reconstruction, although making the procedure more complex, tends to provide superior outcomes, in particular in younger and more active patients.
References
Blunn GW, Walker PS, Joshi A, Hardinge K (1991) The dominance of cyclic sliding in producing wear in total knee replacements. Clin Orthop Relat R 273:253–260
Boissonneault A, Pandit H, Pegg E, Jenkins C, Gill HS, Dodd CA, Gibbons CL, Murray DW (2013) No difference in survivorship after unicompartmental knee arthroplasty with or without an intact anterior cruciate ligament. Knee Surg Sport Tr A 21(11):2480–2486. doi:10.1007/s00167-012-2101-8
Bombaci H, Canbora K, Onur G, Gorgec M (2005) The effect of open wedge osteotomy on the posterior tibial slope. Acta Orthop Traumato 39(5):404–410
Christensen NO (1991) Unicompartmental prosthesis for gonarthrosis. A nine-year series of 575 knees from a Swedish hospital. Clin Orthop Relat R 273:165–169
Citak M, Bosscher MR, Citak M, Musahl V, Pearle AD, Suero EM (2011) Anterior cruciate ligament reconstruction after unicompartmental knee arthroplasty. Knee Surg Sport Tr A 19(10):1683–1688. doi:10.1007/s00167-011-1449-5
Dervin GF, Conway AF, Thurston P (2007) Combined anterior cruciate ligament reconstruction and unicompartmental knee arthroplasty: surgical technique. Orthopedics 30(5 Suppl):39–41
Efe T, Ahmed G, Heyse TJ, Boudriot U, Timmesfeld N, Fuchs-Winkelmann S, Ishaque B, Lakemeier S, Schofer MD (2011) Closing-wedge high tibial osteotomy: survival and risk factor analysis at long-term follow up. BMC Musculoskel Dis 12:46. doi:10.1186/1471-2474-12-46
Engh GA, Ammeen DJ (2014) Unicondylar arthroplasty in knees with deficient anterior cruciate ligaments. Clin Orthop Relat R 472(1):73–77. doi:10.1007/s11999-013-2982-y
Goodfellow JW, Kershaw CJ, Benson MK, O’Connor JJ (1988) The Oxford knee for unicompartmental osteoarthritis. The first 103 cases. J Bone Joint Surg Br 70(5):692–701
Gulati A, Pandit H, Jenkins C, Chau R, Dodd CA, Murray DW (2009) The effect of leg alignment on the outcome of unicompartmental knee replacement. J Bone Joint Surg Br 91(4):469–474. doi:10.1302/0301-620X.91B4.22105
Hernigou P, Deschamps G (2004) Posterior slope of the tibial implant and the outcome of unicompartmental knee arthroplasty. J Bone Joint Surg Am 86-A(3):506–511
Hofmann S, Lobenhoffer P, Staubli A, Van Heerwaarden R (2009) Osteotomies of the knee joint in patients with monocompartmental arthritis. Orthopade 38(8):755–769. doi:10.1007/s00132-009-1458-y (quiz 770)
Hohmann E, Bryant A, Imhoff AB (2006) The effect of closed wedge high tibial osteotomy on tibial slope: a radiographic study. Knee Surg Sport Tr A 14(5):454–459. doi:10.1007/s00167-005-0700-3
Kaplan Y (2011) Identifying individuals with an anterior cruciate ligament-deficient knee as copers and noncopers: a narrative literature review. J Orthop Sport Phys 41(10):758–766. doi:10.2519/jospt.2011.3384
Krishnan SR, Randle R (2009) ACL reconstruction with unicondylar replacement in knee with functional instability and osteoarthritis. J Orthop Surg Res 4:43. doi:10.1186/1749-799X-4-43
Mancuso F, Hamilton TW, Kumar V, Murray DW, Pandit H (2016) Clinical outcome after UKA and HTO in ACL deficiency: a systematic review. Knee Surg Sport Traumatol Arthrosc 24:112–122 doi:10.1007/s00167-014-3346-1
Marti CB, Gautier E, Wachtl SW, Jakob RP (2004) Accuracy of frontal and sagittal plane correction in open-wedge high tibial osteotomy. Arthroscopy 20(4):366–372. doi:10.1016/j.arthro.2004.01.024
Mullis BH, Karas SG, Kelley SS (2007) Characterization of a consistent radiographic finding in chronic anterior cruciate ligament deficiency: the posteromedial osteophyte. Am J Orthop 36(9):494–497
Murray DW, Goodfellow JW, O’Connor JJ (1998) The Oxford medial unicompartmental arthroplasty: a ten-year survival study. J Bone Joint Surg Br 80(6):983–989
Murray DW, Pandit H, Weston-Simons JS, Jenkins C, Gill HS, Lombardi AV, Dodd CA, Berend KR (2013) Does body mass index affect the outcome of unicompartmental knee replacement? Knee 20(6):461–465. doi:10.1016/j.knee.2012.09.017
Pandit H, Beard DJ, Jenkins C, Kimstra Y, Thomas NP, Dodd CA, Murray DW (2006) Combined anterior cruciate reconstruction and Oxford unicompartmental knee arthroplasty. J Bone Joint Surg Br 88(7):887–892. doi:10.1302/0301-620X.88B7.17847
Pandit H, Gulati A, Jenkins C, Barker K, Price AJ, Dodd CA, Murray DW (2011) Unicompartmental knee replacement for patients with partial thickness cartilage loss in the affected compartment. Knee 18(3):168–171. doi:10.1016/j.knee.2010.05.003
Pandit H, Van Duren BH, Gallagher JA, Beard DJ, Dodd CA, Gill HS, Murray DW (2008) Combined anterior cruciate reconstruction and Oxford unicompartmental knee arthroplasty: in vivo kinematics. Knee 15(2):101–106. doi:10.1016/j.knee.2007.11.008
Pegg EC, Mancuso F, Alinejad M, van Duren BH, O’Connor JJ, Murray DW, Pandit HG (2015) Sagittal kinematics of mobile unicompartmental knee replacement in anterior cruciate ligament deficient knees. Clin Biomech 31:33–39. doi:10.1016/j.clinbiomech.2015.10.004
Philpott A, Weston-Simons JS, Grammatopoulos G, Bejon P, Gill HS, McLardy-Smith P, Gundle R, Murray DW, Pandit H (2014) Predictive outcomes of revision total hip replacement—a consecutive series of 1176 patients with a minimum 10-year follow-up. Maturitas 77(2):185–190. doi:10.1016/j.maturitas.2013.10.019
Price AJ, Dodd CA, Svard UG, Murray DW (2005) Oxford medial unicompartmental knee arthroplasty in patients younger and older than 60 years of age. J Bone Joint Surg Br 87(11):1488–1492. doi:10.1302/0301-620X.87B11.16324
Ritter MA, Faris PM, Thong AE, Davis KE, Meding JB, Berend ME (2004) Intra-operative findings in varus osteoarthritis of the knee. An analysis of pre-operative alignment in potential candidates for unicompartmental arthroplasty. J Bone Joint Surg Br 86(1):43–47
Suero EM, Citak M, Cross MB, Bosscher MR, Ranawat AS, Pearle AD (2012) Effects of tibial slope changes in the stability of fixed bearing medial unicompartmental arthroplasty in anterior cruciate ligament deficient knees. Knee 19(4):365–369. doi:10.1016/j.knee.2011.07.004
Suggs JF, Li G, Park SE, Steffensmeier S, Rubash HE, Freiberg AA (2004) Function of the anterior cruciate ligament after unicompartmental knee arthroplasty: an in vitro robotic study. J Arthroplasty 19(2):224–229
Suomalainen P, Jarvela T, Paakkala A, Kannus P, Jarvinen M (2012) Double-bundle versus single-bundle anterior cruciate ligament reconstruction: a prospective randomized study with 5-year results. Am J Sport Med 40(7):1511–1518. doi:10.1177/0363546512448177
Tinius M, Hepp P, Becker R (2012) Combined unicompartmental knee arthroplasty and anterior cruciate ligament reconstruction. Knee Surg Sport Tr A 20(1):81–87. doi:10.1007/s00167-011-1528-7
Trompeter AJ, Gill K, Appleton MA, Palmer SH (2009) Predicting anterior cruciate ligament integrity in patients with osteoarthritis. Knee Surg Sport Tr A 17(6):595–599. doi:10.1007/s00167-008-0701-0
Ventura A, Legnani C, Terzaghi C, Iori S, Borgo E (2015) Medial unicondylar knee arthroplasty combined to anterior cruciate ligament reconstruction. Knee Surg Sport Traumatol Arthrosc. doi:10.1007/s00167-015-3808-0
Weston-Simons JS, Pandit H, Jenkins C, Jackson WF, Price AJ, Gill HS, Dodd CA, Murray DW (2012) Outcome of combined unicompartmental knee replacement and combined or sequential anterior cruciate ligament reconstruction: a study of 52 cases with mean follow-up of 5 years. J Bone Joint Surg Br 94(9):1216–1220. doi:10.1302/0301-620X.94B9.28881
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
One or more of the authors have received or will receive benefits for personal or professional use from a commercial party related directly or indirectly to the subject of this article. In addition, benefits have been or will be directed to a research fund, foundation, educational institution, or other non-profit organisation with which one or more of the authors are associated.
Ethical standards
For this type of study formal consent is not required.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Mancuso, F., Dodd, C.A., Murray, D.W. et al. Medial unicompartmental knee arthroplasty in the ACL-deficient knee. J Orthopaed Traumatol 17, 267–275 (2016). https://doi.org/10.1007/s10195-016-0402-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10195-016-0402-2