Abstract
Purpose
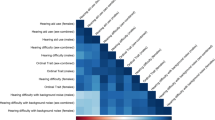
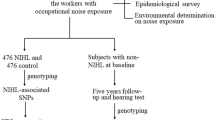
Speech-in-noise (SIN) traits exhibit high inter-subject variability, even for healthy young adults reporting normal hearing. Emerging evidence suggests that genetic variability could influence inter-subject variability in SIN traits. Genome-wide association studies (GWAS) have uncovered the polygenic architecture of various adult-onset complex human conditions. Polygenic risk scores (PRS) summarize complex genetic susceptibility to quantify the degree of genetic risk for health conditions. The present study conducted PRS-based association analyses to identify PRS risk factors for SIN and hearing threshold measures in 255 healthy young adults (18–40 years) with self-reported normal hearing.
Methods
Self-reported SIN perception abilities were assessed by the Speech, Spatial, and Qualities of Hearing Scale (SSQ12). QuickSIN and audiometry (0.25–16 kHz) were performed on 218 participants. Saliva-derived DNA was used for low-pass whole genome sequencing, and 2620 PRS variables for various traits were calculated using the models derived from the polygenic risk score (PGS) catalog. The regression analysis was conducted to identify predictors for SSQ12, QuickSIN, and better ear puretone averages at conventional (PTA0.5–2), high (PTA4-8), and extended-high (PTA12.5–16) frequency ranges.
Results
Participants with a higher genetic predisposition to HDL cholesterol reported better SSQ12. Participants with high PRS to dementia revealed significantly elevated PTA4-8, and those with high PRS to atrial fibrillation and flutter revealed significantly elevated PTA12.5–16.
Conclusion
These results indicate that healthy individuals with polygenic risk of certain health conditions could exhibit a subclinical decline in hearing health measures at young ages, decades before clinically meaningful SIN deficits and hearing loss could be observed. PRS could be used to identify high-risk individuals to prevent hearing health conditions by promoting a healthy lifestyle.




Similar content being viewed by others
Data Availability
The database will be available on NIH dbGaP after the completion of the project R21DC016704-01A1.
Abbreviations
- PRS:
-
Polygenic risk score
- GWAS:
-
Genome-wide association study
- SNP:
-
Single nucleotide polymorphism
References
Carhart R, Tillman TW (1970) Interaction of competing speech signals with hearing losses. Arch Otolaryngol 91(3):273–279
Holmes E, Griffiths TD (2019) ‘Normal’ hearing thresholds and fundamental auditory grouping processes predict difficulties with speech-in-noise perception. Sci Rep 9(1):16771
Shub DE, Makashay MJ, Brungart DS (2020) Predicting speech-in-noise deficits from the audiogram. Ear Hear 41(1):39–54
Beck HE, Zimmermann NE, McVicar TR, Vergopolan N, Berg A, Wood EF (2018) Present and future Köppen-Geiger climate classification maps at 1-km resolution. Scientific data 5(1):1–12
Hind SE, Haines-Bazrafshan R, Benton CL, Brassington W, Towle B, Moore DR (2011) Prevalence of clinical referrals having hearing thresholds within normal limits. Int J Audiol 50(10):708–716
Hunter LL, Monson BB, Moore DR, Dhar S, Wright BA, Munro KJ, Zadeh LM, Blankenship CM, Stiepan SM, Siegel JH (2020) Extended high frequency hearing and speech perception implications in adults and children. Hear Res 397:107922
Liberman MC, Kujawa SG (2017) Cochlear synaptopathy in acquired sensorineural hearing loss: manifestations and mechanisms. Hear Res 349:138–147
Grose JH, Mamo SK, Hall JW III (2009) Age effects in temporal envelope processing: speech unmasking and auditory steady state responses. Ear Hear 30(5):568–575
Darwin CJ (1997) Auditory grouping. Trends Cogn Sci 1(9):327–333
Dryden A, Allen HA, Henshaw H, Heinrich A (2017) The association between cognitive performance and speech-in-noise perception for adult listeners: a systematic literature review and meta-analysis. Trends in hearing 21:2331216517744675
Astheimer LB, Sanders LD (2009) Listeners modulate temporally selective attention during natural speech processing. Biol Psychol 80(1):23–34
Bhatt IS, Washnik N, Torkamani A (2022) Suprathreshold auditory measures for detecting early-stage noise-induced hearing loss in young adults. J Am Acad Audiol 33(04):185–195
Jiang K, Armstrong NM, Agrawal Y, Gross AL, Schrack JA, Lin FR, Ferucci L, Resnick SM, Deal JA, Powell DS (2022) Associations of audiometric hearing and speech-in-noise performance with cognitive decline among older adults: the Baltimore Longitudinal Study of Aging (BLSA). Front Neurol 13:1029851
Stevenson JS, Clifton L, Kuźma E, Littlejohns TJ (2022) Speech-in-noise hearing impairment is associated with an increased risk of incident dementia in 82,039 UK Biobank participants. Alzheimers Dement 18(3):445–456
Brewer CC, Zalewski CK, King KA, Zobay O, Riley A, Ferguson MA, Bird JE, McCabe MM, Hood LJ, Drayna D, Griffith AJ, Morell RJ, Friedman TB, Moore DR (2016) Heritability of non-speech auditory processing skills. Euro J Human Gene 24(8):1137–1144
Saidia AR, Ruel J, Bahloul A, Chaix B, Venail F, Wang J (2023) Current advances in gene therapies of genetic auditory neuropathy spectrum disorder. J Clin Med 12(3):738
Choi JE, Seok JM, Ahn J, Ji YS, Lee KM, Hong SH, Choi BO, Moon IJ (2018) Hidden hearing loss in patients with Charcot-Marie-Tooth disease type 1A. Sci Rep 8(1):1–8
Pinar A, Hawi Z, Cummins T, Johnson B, Pauper M, Tong J, Tiego J, Finlay A, Klein M, Franke B, Fornito A, Bellgrove MA (2018) Genome-wide association study reveals novel genetic locus associated with intra-individual variability in response time. Trans Psychiat 8(1):207
Trampush JW, Yang MLZ, Yu J, Knowles E, Davies G, Liewald DC et al (2017) GWAS meta-analysis reveals novel loci and genetic correlates for general cognitive function: a report from the COGENT consortium. Mole Psychiat 22(3):336–345
Torkamani A, Wineinger NE, Topol EJ (2018) The personal and clinical utility of polygenic risk scores. Nat Rev Genet 19(9):581–590
Chen SF, Dias R, Evans D, Salfati EL, Liu S, Wineinger NE, Torkamani A (2020) Genotype imputation and variability in polygenic risk score estimation. Genome medicine 12:1–13
Choi SW, Mak TSH, O’Reilly PF (2020) Tutorial: a guide to performing polygenic risk score analyses. Nat Protoc 15(9):2759–2772
Lambert SA, Gil L, Jupp S, Ritchie SC, Xu Y, Buniello A et al (2021) The Polygenic Score Catalog as an open database for reproducibility and systematic evaluation. Nat Gene 53(4):420–425
Marston NA, Pirruccello JP, Melloni GE, Koyama S, Kamanu FK, Weng LC et al (2023) Predictive utility of a coronary artery disease polygenic risk score in primary prevention. JAMA Cardiol 8(2):130–137
Tanigawa Y, Qian J, Venkataraman G, Justesen JM, Li R, Tibshirani R, Hastie T, Rivas MA (2022) Significant sparse polygenic risk scores across 813 traits in UK Biobank. PLoS Gene 18(3):e1010105
Dikilitas O, Schaid DJ, Kosel ML, Carroll RJ, Chute CG, Denny JA et al (2020) Predictive utility of polygenic risk scores for coronary heart disease in three major racial and ethnic groups. Am J Human Gene 106(5):707–716
Janssens ACJ (2019) Validity of polygenic risk scores: are we measuring what we think we are? Hum Mol Genet 28(R2):R143–R150
Noble W, Jensen NS, Naylor G, Bhullar N, Akeroyd MA (2013) A short form of the Speech, Spatial and Qualities of Hearing scale suitable for clinical use: the SSQ12. Int J Audiol 52(6):409–412
Killion MC, Niquette PA, Gudmundsen GI, Revit LJ, Banerjee S (2004) Development of a quick speech-in-noise test for measuring signal-to-noise ratio loss in normal-hearing and hearing-impaired listeners. The Journal of the Acoustical Society of America 116(4):2395–2405
Wilson RH, McArdle RA, Smith SL (2007) An evaluation of the BKB-SIN, HINT, QuickSIN, and WIN materials on listeners with normal hearing and listeners with hearing loss. J Speech Lang Hear Res 50(4):844–856
Rubinacci S, Ribeiro DM, Hofmeister RJ, Delaneau O (2021) Efficient phasing and imputation of low-coverage sequencing data using large reference panels. Nat Genet 53(1):120–126
Morales J, Welter D, Bowler EH, Cerezo M, Harris LW, McMahon AC et al (2018) A standardized framework for representation of ancestry data in genomics studies, with application to the NHGRI-EBI GWAS Catalog. Genome Biol 19(1):1–10
Wand H, Lambert SA, Tamburro C, Iacocca MA, O’Sullivan JW, Sillari C et al (2021) Improving reporting standards for polygenic scores in risk prediction studies. Nature 591(7849):211–219
Purcell S, Neale B, Todd-Brown K, Thomas L, Ferreira MA, Bender D et al (2007) PLINK: a tool set for whole-genome association and population-based linkage analyses. Am J Human Gene 81(3):559–575
Benjamini Y, Hochberg Y (1995) Controlling the false discovery rate: a practical and powerful approach to multiple testing. J Roy Stat Soc: Ser B (Methodol) 57(1):289–300
Dai H, Zhang Q, Much AA, Maor E, Segev A, Beinart R et al (2021) Global, regional, and national prevalence, incidence, mortality, and risk factors for atrial fibrillation, 1990–2017: results from the Global Burden of Disease Study 2017. Euro Heart J Qual Care Clin Out 7(6):574–582
Joseph PG, Healey JS, Raina P, Connolly SJ, Ibrahim Q, Gupta R et al; PURE Investigators (2021) Global variations in the prevalence, treatment, and impact of atrial fibrillation in a multi-national cohort of 153 152 middle-aged individuals. Cardiovas Res 117(6):1523–1531
Wang W, Saczynski J, Lessard D, Mailhot T, Barton B, Waring ME et al (2019) Physical, cognitive, and psychosocial conditions in relation to anticoagulation satisfaction among elderly adults with atrial fibrillation: The SAGE-AF study. J Cardiovas Electrophysiol 30(11):2508–2515
Wang WJ, Lessard D, Abu H, McManus DD, Mailhot T, Gurwitz JH, Goldberg RJ, Saczynski J (2020) Hearing loss and cognitive decline among older adults with atrial fibrillation: the SAGE-AF study. J Geriat Cardiol JGC 17(4):177–183
Maharani A, Dawes P, Nazroo J, Tampubolon G, Pendleton N, on behalf of SENSE‐Cog WP1 group (2018) Longitudinal relationship between hearing aid use and cognitive function in older Americans. J Am Geriat Soc 66(6):1130–1136
Lough M, Plack CJ (2022) Extended high-frequency audiometry in research and clinical practice. The Journal of the Acoustical Society of America 151(3):1944–1955
British Society of Audiology (2018) Recommended procedure. Pure-tone air-conduction and bone-conduction threshold audiometry with and without masking. https://www.thebsa.org.uk/resources/pure-tone-air-bone-conduction-threshold-audiometry-without-masking/ (Last viewed April 28, 2023)
Knopke S, Schubert A, Häussler SM, Gräbel S, Szczepek AJ, Olze H (2021) Improvement of working memory and processing speed in patients over 70 with bilateral hearing impairment following unilateral cochlear implantation. J Clin Med 10(15):3421
Utoomprurkporn N, Hardy CJ, Stott J, Costafreda SG, Warren J, Bamiou DE (2020) “The dichotic digit test” as an index indicator for hearing problem in dementia: systematic review and meta-analysis. J Am Acad Audiol 31(09):646–655
Loughrey DG, Kelly ME, Kelley GA, Brennan S, Lawlor BA (2018) Association of age-related hearing loss with cognitive function, cognitive impairment, and dementia: a systematic review and meta-analysis. JAMA Otolaryngol Head Neck Surg 144(2):115–126
Gurgel RK, Ward PD, Schwartz S, Norton MC, Foster NL, Tschanz JT (2014) Relationship of hearing loss and dementia: a prospective, population-based study. Otol Neurotol 35(5):775–781
Kwok SS, Nguyen XMT, Wu DD, Mudar RA, Llano DA (2022) Pure tone audiometry and hearing loss in Alzheimer’s disease: a meta-analysis. Front Psychol 12:6610
Abidin FNZ, Wells HR, Altmann A, Dawson SJ (2021) Hearing difficulty is linked to Alzheimer’s disease by common genetic vulnerability, not shared genetic architecture. NPJ Aging Mech Dis 7(1):17
Nilsson PM, Tuomilehto J, Rydén L (2019) The metabolic syndrome–what is it and how should it be managed? Euro J Prevent Cardiol 26(2_suppl):33–46
Sun YS, Fang WH, Kao TW, Yang HF, Peng TC, Wu LW, Chen LW et al (2015) Components of metabolic syndrome as risk factors for hearing threshold shifts. PloS One 10(8):e0134388
Suzuki K, Kaneko M, Murai K (2000) Influence of serum lipids on auditory function. Laryngoscope 110(10):1736–1738
Lüscher TF, Landmesser U, von Eckardstein A, Fogelman AM (2014) High-density lipoprotein: vascular protective effects, dysfunction, and potential as therapeutic target. Circ Res 114(1):171–182
Le Prell CG, Brungart DS (2016) Speech-in-noise tests and supra-threshold auditory evoked potentials as metrics for noise damage and clinical trial outcome measures. Otol Neurotol 37(8):e295–e302
Wells HR, Freidin MB, Abidin FNZ, Payton A, Dawes P, Munro KJ et al (2019) GWAS identifies 44 independent associated genomic loci for self-reported adult hearing difficulty in UK Biobank. Am J Human Gene 105(4):788–802
Lee J, Dhar S, Abel R, Banakis R, Grolley E, Lee J, Zecker S, Siegel J (2012) Behavioral hearing thresholds between 0.125 and 20 kHz using depth-compensated ear simulator calibration. Ear Hear 33(3):315–329
Liberman MC, Epstein MJ, Cleveland SS, Wang H, Maison SF (2016) Toward a differential diagnosis of hidden hearing loss in humans. PLoS ONE 11(9):e0162726
Alqattan D, Turner P (2021) The effect of background noise on speech perception in monolingual and bilingual adults with normal hearing. Noise Health 23(110):67
Pronk M, Lissenberg-Witte BI, van der Aa HP, Comijs HC, Smits C, Lemke U, Zekveld AA, Kramer SE (2019) Longitudinal relationships between decline in speech-in-noise recognition ability and cognitive functioning: the Longitudinal Aging Study Amsterdam. J Speech Lang Hear Res 62(4S):1167–1187
Smith SB, Krizman J, Liu C, White-Schwoch T, Nicol T, Kraus N (2019) Investigating peripheral sources of speech-in-noise variability in listeners with normal audiograms. Hear Res 371:66–74
Heinrich A (2021) The role of cognition for speech-in-noise perception: considering individual listening strategies related to aging and hearing loss. Int J Behav Dev 45(5):382–388
Heinrich A, Henshaw H, Ferguson MA (2015) The relationship of speech intelligibility with hearing sensitivity, cognition, and perceived hearing difficulties varies for different speech perception tests. Front Psychol 6:782
Acknowledgements
We thank Jeff Lane, Megan Booth, Sarah Kingsbury, Hailey Kingsbury, Klayre Michel, Kila Haney, Qiayi He, Madeline McCarville, and Miranda Becker for their assistance in data collection and handling.
Funding
The study was funded by the National Institute on Deafness and Other Communication Disorders Grant R21DC016704-01A1.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Bhatt, I.S., Ramadugu, S.K., Goodman, S. et al. Polygenic Risk Score-Based Association Analysis of Speech-in-Noise and Hearing Threshold Measures in Healthy Young Adults with Self-reported Normal Hearing. JARO 24, 513–525 (2023). https://doi.org/10.1007/s10162-023-00911-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10162-023-00911-4