Abstract
Background
Autosomal dominant polycystic kidney disease (ADPKD) and autosomal recessive polycystic kidney disease (ARPKD) are major genetic polycystic kidney diseases that can progress to end-stage kidney disease (ESKD). Longitudinal data on the clinical characteristics associated with clinical outcomes in polycystic kidney disease (PKD), including the development of ESKD and cardiovascular disease (CVD) are lacking in Japan. To address this unmet need the authors are establishing a novel, web-based, Nationwide Cohort Registry Study—the Japanese Registry of PKD (JRP).
Methods
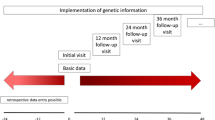
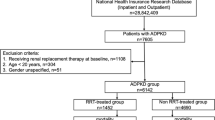
The JRP is a prospective cohort study for ADPKD (aim to recruit n = 1000 patients), and both a retrospective and prospective study for ARPKD (aim to recruit n = 100). In the prospective registry, patients will be followed-up for 10 years every 6 months and 12 months for patients with ADPKD and ARPKD, respectively. Data collection will be recorded on Research Electronic Data Capture (REDCap) starting on April 1, 2024, with recruitment ending on March 31, 2029. (jRCT 1030230618).
Results
Data to be collected include: baseline data, demographics, diagnostic and genetic information, radiological and laboratory findings, and therapeutic interventions. During follow-up, clinical events such as development of ESKD, hospitalization, occurrence of extra kidney complications including CVD events, and death will be recorded, as well as patient-reported health-related quality of life for patients with ADPKD.
Conclusions
The JRP is the first nationwide registry study for patients with ADPKD and ARPKD in Japan, providing researchers with opportunities to advance knowledge and treatments for ADPKD and ARPKD, and to inform disease management and future clinical practice.

Similar content being viewed by others
References
Bergmann C, Guay-Woodford LM, Harris PC, Horie S, Peters DJM, Torres VE. Polycystic kidney disease. Nat Rev Dis Primers. 2018;4(1):50. https://doi.org/10.1038/s41572-018-0047-y.
Mochizuki T, Wu G, Hayashi T, Xenophontos SL, Veldhuisen B, Saris JJ, et al. PKD2, a gene for polycystic kidney disease that encodes an integral membrane protein. Science. 1996;272(5266):1339–42. https://doi.org/10.1126/science.272.5266.1339.
Cornec-Le Gall E, Alam A, Perrone RD. Autosomal dominant polycystic kidney disease. Lancet. 2019;393(10174):919–35. https://doi.org/10.1016/S0140-6736(18)32782-X.
Ward CJ, Hogan MC, Rossetti S, Walker D, Sneddon T, Wang X, et al. The gene mutated in autosomal recessive polycystic kidney disease encodes a large, receptor-like protein. Nat Genet. 2002;30(3):259–69. https://doi.org/10.1038/ng833.
Torres VE, Harris PC, Pirson Y. Autosomal dominant polycystic kidney disease. Lancet. 2007;369(9569):1287–301. https://doi.org/10.1016/S0140-6736(07)60601-1.
Dicks E, Ravani P, Langman D, Davidson WS, Pei Y, Parfrey PS. Incident renal events and risk factors in autosomal dominant polycystic kidney disease: a population and family-based cohort followed for 22 years. Clin J Am Soc Nephrol. 2006;1(4):710–7. https://doi.org/10.2215/CJN.01581105.
Ostroff C, Perrone RD, Czerwiec FS. Current challenges and perspectives on developing a clinical trial design for ADPKD. Clin J Am Soc Nephrol. 2022;17(10):1559–62. https://doi.org/10.2215/CJN.05360522.
Cornec-Le Gall E, Audrezet MP, Chen JM, Hourmant M, Morin MP, Perrichot R, et al. Type of PKD1 mutation influences renal outcome in ADPKD. J Am Soc Nephrol. 2013;24(6):1006–13. https://doi.org/10.1681/ASN.2012070650.
Uchiyama K, Mochizuki T, Shimada Y, Nishio S, Kataoka H, Mitobe M, et al. Factors predicting decline in renal function and kidney volume growth in autosomal dominant polycystic kidney disease: a prospective cohort study (Japanese polycystic kidney disease registry: J-PKD). Clin Exp Nephrol. 2021;25(9):970–80. https://doi.org/10.1007/s10157-021-02068-x.
Guay-Woodford LM, Desmond RA. Autosomal recessive polycystic kidney disease: the clinical experience in North America. Pediatrics. 2003;111(5 Pt 1):1072–80. https://doi.org/10.1542/peds.111.5.1072.
Guay-Woodford LM, Bissler JJ, Braun MC, Bockenhauer D, Cadnapaphornchai MA, Dell KM, et al. Consensus expert recommendations for the diagnosis and management of autosomal recessive polycystic kidney disease: report of an international conference. J Pediatr. 2014;165(3):611–7. https://doi.org/10.1016/j.jpeds.2014.06.015.
Burgmaier K, Kilian S, Bammens B, Benzing T, Billing H, Buscher A, et al. Clinical courses and complications of young adults with autosomal recessive polycystic kidney disease (ARPKD). Sci Rep. 2019;9(1):7919. https://doi.org/10.1038/s41598-019-43488-w.
Bergmann C, Senderek J, Sedlacek B, Pegiazoglou I, Puglia P, Eggermann T, et al. Spectrum of mutations in the gene for autosomal recessive polycystic kidney disease (ARPKD/PKHD1). J Am Soc Nephrol. 2003;14(1):76–89. https://doi.org/10.1097/01.asn.0000039578.55705.6e.
Ebner K, Feldkoetter M, Ariceta G, Bergmann C, Buettner R, Doyon A, et al. Rationale, design and objectives of ARegPKD, a European ARPKD registry study. BMC Nephrol. 2015;16:22. https://doi.org/10.1186/s12882-015-0002-z.
Nishio S, Tsuchiya K, Nakatani S, Muto S, Mochizuki T, Kawano H, et al. A digest from evidence-based clinical practice guideline for polycystic kidney disease 2020. Clin Exp Nephrol. 2021;25(12):1292–302. https://doi.org/10.1007/s10157-021-02097-6.
Inaguma D, Imai E, Takeuchi A, Ohashi Y, Watanabe T, Nitta K, et al. Risk factors for CKD progression in Japanese patients: findings from the chronic kidney disease japan cohort (CKD-JAC) study. Clin Exp Nephrol. 2017;21(3):446–56. https://doi.org/10.1007/s10157-016-1309-1.
Perrone RD, Oberdhan D, Ouyang J, Bichet DG, Budde K, Chapman AB, et al. Overture: a worldwide, prospective, observational study of disease characteristics in patients with ADPKD. Kidney Int Rep. 2023;8(5):989–1001. https://doi.org/10.1016/j.ekir.2023.02.1073.
Joly D, Quinn J, Mokiou S, O’Reilly K, Sanchez-Covisa J, Wang-Silvanto J, et al. Rationale and study protocol of ACQUIRE, a prospective, observational study measuring quality of life, treatment preference and treatment satisfaction of autosomal dominant polycystic kidney disease (ADPKD) patients in Europe. BMC Nephrol. 2020;21(1):298. https://doi.org/10.1186/s12882-020-01927-1.
Park HC, Ryu H, Kim YC, Ahn C, Lee KB, Kim YH, et al. Genetic identification of inherited cystic kidney diseases for implementing precision medicine: a study protocol for a 3-year prospective multicenter cohort study. BMC Nephrol. 2021;22(1):2. https://doi.org/10.1186/s12882-020-02207-8.
Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)–a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–81. https://doi.org/10.1016/j.jbi.2008.08.010.
Uemura O, Nagai T, Ishikura K, Ito S, Hataya H, Gotoh Y, et al. Creatinine-based equation to estimate the glomerular filtration rate in Japanese children and adolescents with chronic kidney disease. Clin Exp Nephrol. 2014;18(4):626–33. https://doi.org/10.1007/s10157-013-0856-y.
Uemura O, Ishikura K, Gotoh Y, Honda M. Creatinine-based estimated glomerular filtration rate for children younger than 2 years. Clin Exp Nephrol. 2018;22(2):483–4. https://doi.org/10.1007/s10157-017-1460-3.
Matsuo S, Imai E, Horio M, Yasuda Y, Tomita K, Nitta K, et al. Revised equations for estimated GFR from serum creatinine in Japan. Am J Kidney Dis. 2009;53(6):982–92. https://doi.org/10.1053/j.ajkd.2008.12.034.
Uemura O, Nagai T, Ishikura K, Ito S, Hataya H, Gotoh Y, et al. Cystatin C-based equation for estimating glomerular filtration rate in Japanese children and adolescents. Clin Exp Nephrol. 2014;18(5):718–25. https://doi.org/10.1007/s10157-013-0910-9.
Kallich JD, Hays RD, Mapes DL, Coons SJ, Carter WB. The RAND kidney disease and quality of life instrument. Nephrol News Issues. 1995;9(9):29–36.
Simms RJ, Thong KM, Dworschak GC, Ong AC. Increased psychosocial risk, depression and reduced quality of life living with autosomal dominant polycystic kidney disease. Nephrol Dial Transplant. 2016;31(7):1130–40. https://doi.org/10.1093/ndt/gfv299.
Anderegg MA, Dhayat NA, Sommer G, Semmo M, Huynh-Do U, Vogt B, et al. Quality of life in autosomal dominant polycystic kidney disease patients treated with tolvaptan. Kidney Med. 2020;2(2):162–71. https://doi.org/10.1016/j.xkme.2019.11.008.
Muto S, Ando M, Nishio S, Hanaoka K, Ubara Y, Narita I, et al. The relationship between liver cyst volume and QOL in Japanese ADPKD patients. Clin Exp Nephrol. 2020;24(4):314–22. https://doi.org/10.1007/s10157-019-01830-6.
Chapman AB, Wei W. Imaging approaches to patients with polycystic kidney disease. Semin Nephrol. 2011;31(3):237–44. https://doi.org/10.1016/j.semnephrol.2011.05.003.
Mori T, Hosomichi K, Chiga M, Mandai S, Nakaoka H, Sohara E, et al. Comprehensive genetic testing approach for major inherited kidney diseases, using next-generation sequencing with a custom panel. Clin Exp Nephrol. 2017;21(1):63–75. https://doi.org/10.1007/s10157-016-1252-1.
Moriyama T, Nakayama Y, Soejima M, Yokota Y, Ota K, Ito S, et al. Effect of tolvaptan on renal involvement in patients with autosomal dominant polycystic kidney disease according to different gene mutations. Clin Exp Nephrol. 2021;25(3):251–60. https://doi.org/10.1007/s10157-020-01988-4.
Obeid JS, McGraw CA, Minor BL, Conde JG, Pawluk R, Lin M, et al. Procurement of shared data instruments for research electronic data capture (REDCap). J Biomed Inform. 2013;46(2):259–65. https://doi.org/10.1016/j.jbi.2012.10.006.
Adeva M, El-Youssef M, Rossetti S, Kamath PS, Kubly V, Consugar MB, et al. Clinical and molecular characterization defines a broadened spectrum of autosomal recessive polycystic kidney disease (ARPKD). Medicine (Baltimore). 2006;85(1):1–21. https://doi.org/10.1097/01.md.0000200165.90373.9a.
Bergmann C, Senderek J, Windelen E, Kupper F, Middeldorf I, Schneider F, et al. Clinical consequences of PKHD1 mutations in 164 patients with autosomal-recessive polycystic kidney disease (ARPKD). Kidney Int. 2005;67(3):829–48. https://doi.org/10.1111/j.1523-1755.2005.00148.x.
Burgmaier K, Ariceta G, Bald M, Buescher AK, Burgmaier M, Erger F, et al. Severe neurological outcomes after very early bilateral nephrectomies in patients with autosomal recessive polycystic kidney disease (ARPKD). Sci Rep. 2020;10(1):16025. https://doi.org/10.1038/s41598-020-71956-1.
Burgmaier K, Kilian S, Arbeiter K, Atmis B, Buscher A, Derichs U, et al. Early childhood height-adjusted total kidney volume as a risk marker of kidney survival in ARPKD. Sci Rep. 2021;11(1):21677. https://doi.org/10.1038/s41598-021-00523-z.
Oberdhan D, Cole JC, Krasa HB, Cheng R, Czerwiec FS, Hays RD, et al. Development of the autosomal dominant polycystic kidney disease impact scale: a new health-related quality-of-life instrument. Am J Kidney Dis. 2018;71(2):225–35. https://doi.org/10.1053/j.ajkd.2017.08.020.
Acknowledgements
This study was supported in part by a Grant-in-Aid for Intractable Renal Diseases Research, Research on rare and intractable diseases, Health and Labour Sciences Research Grants from the Ministry of Health, Labour and Welfare of Japan. The authors acknowledge valuable contributions of the following collaborators and Dr. Keiko Ota at the Department of Center for Clinical Research and Innovation, Osaka Metropolitan University.
The JRP collaborators: Satoru Muto, Haruna Kawano, Amane Endo, Tomoki Kimura, Yosuke Shimada, Juntendo University Hospital; Junichi Hoshino, Ken Tsuchiya, Hiroshi Kataoka, Shiho Makabe, Shun Manabe, Yusuke Ushio, Kenichiro Miura, Tokyo Women's Medical University Hospital; Shinya Nakatani, Osaka Metropolitan University; Koichi Nakanishi, Wataru Shimabukuro, University of the Ryukyus Hospital; Mai Sato, National Center for Child Health and Development; Saori Nishio, Fumihiko Hattanda, Hokkaido University Hospital; Tomofumi Moriyama,Seiji Tanaka, Tomofumi Moriyama, Kurume University Hospital; Kiyotaka Uchiyama, International University of Health and Welfare Narita Hospital; Daisuke Ichikawa, St. Marianna University School of Medicine Hospital; Hirayasu Kai, University of Tsukuba Hospital; Kazushige Hanaoka, Mahiro Kurashige, The Jikei University Hospital; Tadashi Otsuka, Hirofumi Watanabe, Takeshi Yamada, Niigata University Medical and Dental Hospital; Hiroki Hayashi, Fujita Health University Hospital; Kan Katayama, Mie University Hospital; Keiji Shimazu, Osaka Saiseikai Nakatsu Hospital; Koichi Seta, National Hospital Organization Kyoto Medical Center; Eiji Ishikawa, Saiseikai Matsusaka Genera Hospital; Sumi Hidaka, Shonan Kamakura General Hospital; Michihiro Mitobe, Takeda General Hospital; Takehiko Wada, Tatsuya Suwabe, Akinari Sekine, Toranomon Hospital; Toshio Mochizuki, PKD Nephrology Clinic; Takuya Fujimaru, Luke's International Hospital;Yoshinobu Nagaoka, Sapporo Medical University Hospital; Tanaka Hiroshi, Hirosaki University Hospital; Noriko Sugawara, Tohoku University Hospital; Hiroaki Tamura, Akita University Hospital; Ogino Daisuke, Yamagata University Hospital; Yuji Kano, Dokyo Medical University Hospital; Shuichiro Fujinaga, Saitama Prefectural Children’s Medical Center; Yuko Akioka, Saitama Medical University Hospital; Ryugo Hiramoto, Matsudo City General Hospital; Ken Kawamura, Seirei Sakura Citizen Hospital; Yuko Hamasaki, Toho University Omori Medical Center; Riku Hamada, Tokyo Metropolitan Children's Medical Center; Takeshi Yanagihara, Nippon Medical School Musashikosugi Hospital; Aya Inaba, Yokohama City University Medical Center; Hirotsugu Kitayama, Shizuoka Children’s Hospital; Masaki Yamamoto, Seirei Hamamatsu General Hospital; Yoshimitsu Goto, Japanese Red Cross Nagoya Daini Hospital; Naoya Fujita, Aichi Children's Health and Medical Center; Eiji Matsukuma, Gifu Prefectural General Medical Center; Toshihiro Sawai, Shiga University of Medical Science Hospital; Rika Fujimaru, Osaka City General Hospital; Kaori Fujiwara, Osaka Women's and Children's Hospital; Masashi Nishida, Japanese Red Cross Kyoto Daiichi Hospital; Takahisa Yoshikawa, Kyoto University Hospital; Kandai Nozu, Kobe University Hospital; Hiroshi Kaito, Hyogo Prefectural Kobe Children's Hospital; Naohiro Kamiyoshi, Japanese Red Cross Society Himeji Hospital; Tomoaki Ishikawa, Nara Medical University Hospital; Yuko Shima, Wakayama Medical University Hospital; Toshiyuki Ota, Hiroshima Prefectural Hospital; Kei Nishiyama, Kyushu University Hospital; Yoshitsugu Kaku, Fukuoka Children's Hospital Masafumi Oka, Saga University Hospital;, Hitoshi Nakazato, Kumamoto, University Hospital; Hideki Ban, Kumamoto Red Cross Hospital; Shinichi Shiona, Oita Prefectural Hospital; Takao Konomoto, University of Miyazaki Hospital; Akinori Miyazono, Kagoshima University Hospital; Tomoo Kise, Nanbu Medical Center, Children’s Medical Center; Kenichi Maruyama, Gunma Children’s Medical Center; Ayano Inui, Saiseikai Yokohamashi Tobu Hospital; Hideaki Okajima, Kanazawa Medical University Hospital; Takuo Kubota, Yoshitaka Isaka, Osaka University Hospital; Yukihiro Inomata, Kumamoto Rosai Hospital; and Toshifumi Yodoshi, Okinawa Chubu Hospital.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
All the authors have declared no competing interest.
Ethical approval
This study will be conducted in accordance with the 1964 Declaration of Helsinki, and the Ethical Guidelines for Medical and Health Research Involving Human Subjects by the Ministry of Health, Labor and Welfare and Ministry of Education, Japan (original version 2016, which was modified in 2017). The study protocol was reviewed and approved by the Ethics Committee, Juntendo University, Tokyo, Japan (Approval No. E23-0140), and was registered at Japan Registry of Clinical Trials (jRCT 1030230618).
Informed consent
Informed consent or assent (for minors) is to be obtained from all individual patients included in the study. An opt-out option is given for ARPKD patients who have been treated in the past and transferred to other hospitals, or who have died, as explained in the instructions posted on the website of the institution.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Nakatani, S., Kawano, H., Sato, M. et al. Protocol for the nationwide registry of patients with polycystic kidney disease: japanese national registry of PKD (JRP). Clin Exp Nephrol (2024). https://doi.org/10.1007/s10157-024-02509-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10157-024-02509-3