Abstract
Background
The number of marginal living kidney donors has increased. Medically complex donors who have hypertension, older age, or low estimated glomerular filtration rate (eGFR) have been more likely to be used.
Methods
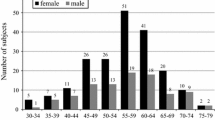
We conducted a retrospective cohort study of living kidney donors at a single center. We analyzed 309 living donors and divided them into three groups: group with older donors (aged ≥70 years) (n = 41), middle-aged (aged 46–69 years) (n = 239), and young donors (aged <46 years) (N = 29). Donor factors associated with chronic kidney disease (CKD) stage 3b or worse within 5 years post-donation were investigated.
Results
Of the 309 live donors, 86 (27.8%) developed CKD stage3b or worse within 5 years post-donation. The incidence of CKD stage3b or worse within 5 years post-donation was significantly higher in older donor (p < 0.01). Cox regression models revealed that older donor ages and lower eGFR were significantly related to the development of CKD stage3b or worse, independent of comorbidities such as obesity and hypertension [hazard ratio (95% CI); 4.59 (1.02–20.6), p = 047, 0.95 (0.94–0.96), p ≤ 0.01, respectively]. However, recovery of eGFR 4–5 years after donation was noted in the middle-aged and older donor groups, whereas the level of eGFR remained unchanged in the young group.
Conclusions
Older donors tend to develop CKD stage3b within 5 years post-donation but with the potential of recovery. Healthy older people (aged ≥70 years) could be candidates for living donors under careful monitoring of kidney function after donation.


Similar content being viewed by others
Data availability
The data which support the findings of this study are available from the corresponding author, [K.U.], upon reasonable request.
References
Aikawa A. Current status and future aspects of kidney transplantation in Japan. Ren Replace Ther. 2018;4:1–12. https://doi.org/10.1186/s41100-018-0186-3.
(IRODaT) IRiODaT. International registry in organ donation and transplantation (IRODaT) newsletter 20 IRODaT—international registry on organ donation and transplantation, WORLDWIDE ACTUAL DECEASED ORGAN DONORS 2020 (PMP). https://www.irodat.org/img/database/grafics/2020_01_worldwide-actual-deceased-organ-donors.png.
Reese PP, Feldman HI, McBride MA, Anderson K, Asch DA, Bloom RD. Substantial variation in the acceptance of medically complex live kidney donors across US renal transplant centers. Am J Transplant. 2008;8(10):2062–70. https://doi.org/10.1111/j.1600-6143.2008.02361.x.
Delmonico F. A report of the Amsterdam forum on the care of the live kidney donor: data and medical guidelines. Transplantation. 2005;79(6 Suppl):S53-66.
Muzaale AD, Massie AB, Wang MC, et al. Risk of end-stage renal disease following live kidney donation. JAMA. 2014;311(6):579–86. https://doi.org/10.1001/jama.2013.285141.
Al Ammary F, Luo X, Muzaale AD, et al. Risk of ESKD in older live kidney donors with hypertension. Clin J Am Soc Nephrol. 2019;14(7):1048–55. https://doi.org/10.2215/cjn.14031118.
Matas AJ, Berglund DM, Vock DM, Ibrahim HN. Causes and timing of end-stage renal disease after living kidney donation. Am J Transplant. 2018;18(5):1140–50. https://doi.org/10.1111/ajt.14671.
Araki E, Goto A, Kondo T, et al. Japanese clinical practice guideline for diabetes 2019. Diabetol Int. 2020;11(3):165–223. https://doi.org/10.1007/s13340-020-00439-5.
Solez K, Axelsen RA, Benediktsson H, et al. International standardization of criteria for the histologic diagnosis of renal allograft rejection: the Banff working classification of kidney transplant pathology. Kidney Int. 1993;44(2):411–22. https://doi.org/10.1038/ki.1993.259.
Rule AD, Amer H, Cornell LD, et al. The association between age and nephrosclerosis on renal biopsy among healthy adults. Ann Intern Med. 2010;152(9):561–7. https://doi.org/10.7326/0003-4819-152-9-201005040-00006.
Roufosse C, Simmonds N, Clahsen-van Groningen M, et al. A 2018 reference guide to the Banff classification of renal allograft pathology. Transplantation. 2018;102(11):1795–814. https://doi.org/10.1097/tp.0000000000002366.
Matsuo S, Imai E, Horio M, et al. Revised equations for estimated GFR from serum creatinine in Japan. Am J Kidney Dis. 2009;53(6):982–92. https://doi.org/10.1053/j.ajkd.2008.12.034.
Devanand V, Chithrapavai SU. Correlation of 2 hours and 24 hours creatinine clearance in renal donors after unilateral nephrectomy. J Clin Diagn Res. 2013;7(10):2119–21. https://doi.org/10.7860/jcdr/2013/5696.3447.
Minutolo R, Lapi F, Chiodini P, et al. Risk of ESRD and death in patients with CKD not referred to a nephrologist: a 7-year prospective study. Clin J Am Soc Nephrol. 2014;9(9):1586–93. https://doi.org/10.2215/cjn.10481013.
Kazancioğlu R. Risk factors for chronic kidney disease: an update. Kidney Int Suppl (2011). 2013;3(4):368–71. https://doi.org/10.1038/kisup.2013.79.
Menn-Josephy H, Lee CS, Nolin A, et al. Renal interstitial fibrosis: an imperfect predictor of kidney disease progression in some patient cohorts. Am J Nephrol. 2016;44(4):289–99. https://doi.org/10.1159/000449511.
Augustine JJ, Arrigain S, Mandelbrot DA, Schold JD, Poggio ED. Factors associated with residual kidney function and proteinuria after living kidney donation in the United States. Transplantation. 2021;105(2):372–81. https://doi.org/10.1097/tp.0000000000003210.
Locke JE, Reed RD, Massie A, et al. Obesity increases the risk of end-stage renal disease among living kidney donors. Kidney Int. 2017;91(3):699–703. https://doi.org/10.1016/j.kint.2016.10.014.
Lentine KL, Patel A. Risks and outcomes of living donation. Adv Chronic Kidney Dis. 2012;19(4):220–8. https://doi.org/10.1053/j.ackd.2011.09.005.
Grams ME, Sang Y, Levey AS, et al. Kidney-failure risk projection for the living kidney-donor candidate. N Engl J Med. 2016;374(5):411–21. https://doi.org/10.1056/NEJMoa1510491.
Hommos MS, Glassock RJ, Rule AD. Structural and functional changes in human kidneys with healthy aging. J Am Soc Nephrol. 2017;28(10):2838–44. https://doi.org/10.1681/asn.2017040421.
Nishida S, Hidaka Y, Toyoda M, et al. Factors related to suboptimal recovery of renal function after living donor nephrectomy: a retrospective study. BMC Nephrol. 2019;20(1):403. https://doi.org/10.1186/s12882-019-1588-3.
Mueller TF, Luyckx VA. The natural history of residual renal function in transplant donors. J Am Soc Nephrol. 2012;23(9):1462–6. https://doi.org/10.1681/asn.2011111080.
Lenihan CR, Busque S, Derby G, Blouch K, Myers BD, Tan JC. Longitudinal study of living kidney donor glomerular dynamics after nephrectomy. J Clin Invest. 2015;125(3):1311–8. https://doi.org/10.1172/jci78885.
Lam NN, Lloyd A, Lentine KL, et al. Changes in kidney function follow living donor nephrectomy. Kidney Int. 2020;98(1):176–86. https://doi.org/10.1016/j.kint.2020.03.034.
Rook M, Hofker HS, van Son WJ, Homan van der Heide JJ, Ploeg RJ, Navis GJ. Predictive capacity of pre-donation GFR and renal reserve capacity for donor renal function after living kidney donation. Am J Transplant. 2006;6(7):1653–9. https://doi.org/10.1111/j.1600-6143.2006.01359.x
Tan JC, Busque S, Workeneh B, et al. Effects of aging on glomerular function and number in living kidney donors. Kidney Int. 2010;78(7):686–92. https://doi.org/10.1038/ki.2010.128.
Rota-Musoll L, Brigidi S, Molina-Robles E, Oriol-Vila E, Perez-Oller L, Subirana-Casacuberta M. An intersectional gender analysis in kidney transplantation: women who donate a kidney. BMC Nephrol. 2021;22(1):59. https://doi.org/10.1186/s12882-021-02262-9.
Lentine KL, Kasiske BL, Levey AS, et al. KDIGO Clinical practice guideline on the evaluation and care of living kidney donors. Transplantation. 2017;101(8S Suppl 1):S1–109. https://doi.org/10.1097/tp.0000000000001769.
Andrews PA, Burnapp L. British transplantation society / renal association UK guidelines for living donor kidney transplantation 2018: summary of updated guidance. Transplantation. 2018;102(7):e307. https://doi.org/10.1097/tp.0000000000002253.
ERBP guideline on the management and evaluation of the kidney donor and recipient. Nephrol Dial Transplant. 2013;28(Suppl 2):ii1–71. https://doi.org/10.1093/ndt/gft218.
Richardson R, Connelly M, Dipchand C, et al. Kidney paired donation protocol for participating donors 2014. Transplantation. 2015;99(10 Suppl 1):S1-s88. https://doi.org/10.1097/tp.0000000000000918.
Acknowledgements
We are grateful to “Editage” for assistance with the English proofreading.
Funding
The authors declare that they have no relevant financial interests.
Author information
Authors and Affiliations
Contributions
RO, KU, and HI conceived the idea of the study. RO, KU and JH developed the statistical analysis plan and conducted statistical analyses. TB, TY, TH, KO, KK, TS, and ST contributed to the interpretation of the results. RO drafted the original manuscript. TT, and HI supervised the conduct of this study. All authors reviewed the manuscript draft and revised it critically on intellectual content. All authors approved the final version of the manuscript to be published.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing financial or other interest or personal relationship that could have influenced this paper or the study it describes.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
About this article
Cite this article
Oki, R., Unagami, K., Banno, T. et al. Renal outcome of living kidney donors aged more than 70 years. Clin Exp Nephrol (2024). https://doi.org/10.1007/s10157-024-02488-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10157-024-02488-5