Abstract
Background
Proton-pump inhibitors (PPIs) are widely used to treat gastroesophageal reflex disease, peptic ulcer disease, and stress ulcer prophylaxis. This study estimated the progress rate of renal dysfunction in patients taking PPIs in clinical settings and compared the results with those of patients taking histamine-2 receptor antagonists (H2RAs).
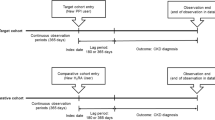
Methods
We retrospectively reviewed patients’ data collected from Kochi Medical School Hospital’s information system between 2001 and 2019. Patients were classified into PPI and H2RA groups, and survival time was defined as the period between initial drug administration and a 30% decrease in estimated glomerular filtration rate (eGFR).
Results
On survival analysis, the PPI group was associated with higher event incidence rates compared to that in the H2RA group. The rate of underlying disease was significantly higher in the PPI group than in the H2RA group, with no significant differences in age and sex between the groups. Comparing the PPI group to the H2RA group, the use of aspirin, clopidogrel, statin, and angiotensin II receptor blocker was significantly higher, whereas the use of non-steroidal anti-inflammatory drugs and steroids was significantly less. Regarding survival rate and 30% decrease in eGFR, the PPI group had a significantly higher survival rate compared to that in the H2RA group at 730 days, but not earlier. PPI use, older age, and eGFR ≥ 90 mL/min/1.73 m2 exhibited high hazard ratios.
Conclusions
PPI use was significantly associated with an increased risk of chronic kidney disease development compared to that with H2RA use.


Similar content being viewed by others
References
Forgacs I, Loganayagam A. Overprescribing proton pump inhibitors. BMJ. 2008;336:2–3.
Farrell B, Pottie K, Thompson W, et al. Deprescribing proton pump inhibitors: evidence-based clinical practice guideline. Can Fam Physician. 2017;63:354–64.
Maher RL, Hanlon J, Hajjar ER. Clinical consequences of polypharmacy in elderly. Expert Opin Drug Saf. 2014;13:57–65.
Benmassaoud A, McDonald EG, Lee TC. Potential harms of proton pump inhibitor therapy: rare adverse effects of commonly used drugs. CMAJ. 2016;188:657–62.
Johnstone J, Nerenberg K, Loeb M. Meta-analysis: proton pump inhibitor use and the risk of community-acquired pneumonia. Aliment Pharmacol Ther. 2010;31:1165–77.
Leonard J, Marshall JK, Moayyedi P. Systematic review of the risk of enteric infection in patients taking acid suppression. Am J Gastroenterol. 2007;102:2047–57.
Blank ML, Parkin L, Paul C, Herbison P. A nationwide nested case-control study indicates an increased risk of acute interstitial nephritis with proton pump inhibitor use. Kidney Int. 2014;86:837–44.
Xie Y, Bowe B, Li T, Xian H, Yan Y, Al-Aly Z. Risk of death among users of proton pump inhibitors: a longitudinal observational cohort study of United States veterans. BMJ Open. 2017;7:e015735.
Coca SG, Singanamala S, Parikh CR. Chronic kidney disease after acute kidney injury: a systematic review and meta-analysis. Kidney Int. 2012;81:442–8.
Härmark L, van der Wiel HE, de Groot MC, van Grootheest AC. Proton pump inhibitor-induced acute interstitial nephritis. Br J Clin Pharmacol. 2007;64:819–23.
Lazarus B, Chen Y, Wilson FP, et al. Proton pump inhibitor use and the risk of chronic kidney disease. JAMA Intern Med. 2016;176:238–46.
Xie Y, Bowe B, Li T, Xian H, Balasubramanian S, Al-Aly Z. Proton pump inhibitors and risk of incident CKD and progression to ESRD. J Am Soc Nephrol. 2016;27:3153–63.
Antoniou T, Macdonald EM, Hollands S, et al. Proton pump inhibitors and the risk of acute kidney injury in older patients: a population-based cohort study. CMAJ Open. 2015;3:E166–71.
Qiu T, Zhou J, Zhang C. Acid-suppressive drugs and risk of kidney disease: a systematic review and meta-analysis. J Gastroenterol Hepatol. 2018. https://doi.org/10.1111/jgh.14157.
Klepser DG, Collier DS, Cochran GL. Proton pump inhibitors and acute kidney injury: a nested case-control study. BMC Nephrol. 2013;14:150.
Yang Y, George KC, Shang WF, Zeng R, Ge SW, Xu G. Proton-pump inhibitors use, and risk of acute kidney injury: a meta-analysis of observational studies. Drug Des Devel Ther. 2017;11:1291–9.
Lee J, Mark RG, Celi LA, Danziger J. Proton pump inhibitors are not associated with acute kidney injury in critical illness. J Clin Pharmacol. 2016;56:1500–6.
Otomo K, Horino T, Miki T, et al. Serum uric acid level as a risk factor for acute kidney injury in hospitalized patients: a retrospective database analysis using the integrated medical information system at Kochi Medical School hospital. Clin Exp Nephrol. 2016;20:235–43.
Matsuo S, Imai E, Horio M, et al. Revised equations for estimated GFR from serum creatinine in Japan. Am J Kidney Dis. 2009;53:982–92.
Kanda E, Usui T, Kashihara N, Iseki C, Iseki K, Nangaku M. Importance of glomerular filtration rate change as surrogate endpoint for the future incidence of end-stage renal disease in general Japanese population: community-based cohort study. Clin Exp Nephrol. 2018;22:318–27.
Wijarnpreecha K, Thongprayoon C, Chesdachai S, Panjawatanana P, Ungprasert P, Cheungpasitporn W. Associations of proton-pump inhibitors and H2 receptor antagonists with chronic kidney disease: a meta-analysis. Dig Dis Sci. 2017;62:2821–7.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have declared that no conflict of interest exists.
Ethical approval
All procedures performed this study were in accordance with the ethical standards of and approved by the ethical review board of Kochi Medical School (approval No. 23-15) and were conducted in accordance with the 1964 Helsinki Declaration and its later amendments.
Informed consent
All patient data were obtained from the hospital’s central clinical data warehouse (the Retrieval System for Open Medical Analysis 2 warehouse) with general consent from patients through the opt-out policy of the Kochi Medical School Hospital.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Hatakeyama, Y., Horino, T., Matsumoto, T. et al. Long-term continuous use of proton-pump inhibitors is associated with renal function decline in patients without acute kidney injury. Clin Exp Nephrol 25, 1087–1092 (2021). https://doi.org/10.1007/s10157-021-02066-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10157-021-02066-z