Abstract
Background
The baseline data obtained in the CKD-JAC demonstrated that insufficient treatment was being provided for renal anemia by institutions specializing in renal disease. The objective of this study was to investigate the status of treatment for renal anemia, including renal/cardiovascular outcomes and mortality, at regional medical facilities since the development of long-acting erythropoiesis-stimulating agents (LA-ESA).
Methods
Non-dialysis outpatients with chronic kidney disease and renal anemia were eligible. Anemia was treated based on the clinical condition of each patient and targeted hemoglobin (Hb) levels.
Results
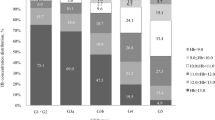
A total of 283 patients from 21 institutions were enrolled and followed up for a maximum of 3 years. A doubling of the serum creatinine level was observed in 89 patients, and renal replacement therapy was initiated in 57 patients. Multivariate Cox regression analysis revealed that a lower mean Hb level (mHb) and receiving fewer frequency of ESA during the follow-up period were independent determinants of the composite renal outcome and overall mortality. During the follow-up period, the percentages of patients with mHb of 10–10.9 g/dL and ≥ 11 g/dL were increased. Similar trends were seen regardless of whether the patients were treated by nephrologists or non-nephrologists. The frequency of ESA treatment was increased among the patients treated by non-nephrologists; however, it was much lower than nephrologists.
Conclusion
This study demonstrated that, in the era of LA-ESA treatment, higher Hb levels are associated with reduced composite renal outcomes at regional medical facilities. The importance of renal anemia management should be highlighted, even among non-nephrologists.



Similar content being viewed by others
References
Kazmi WH, Kausz AT, Khan S, et al. Anemia: an early complication of chronic renal insufficiency. Am J Kidney Dis. 2001;38:803–12.
Gouva C, Nikolopoulos P, Ioannidis JP, et al. Treating anemia early in renal failure patients slows the decline of renal function: a randomized controlled trial. Kidney Int. 2004;66:753–60.
Kuriyama S, Tomonari H, Yoshida H, et al. Reversal of anemia by erythropoietin therapy retards the progression of chronic renal failure, especially in nondiabetic patients. Nephron. 1997;77:176–85.
Silverberg DS, Wexler D, Blum M, et al. Aggressive therapy of congestive heart failure and associated chronic renal failure with medications and correction of anemia stops or slows the progression of both diseases. Perit Dial Int. 2001;21(Suppl 3):S236–S240.
Hayashi T, Suzuki A, Shoji T, et al. Cardiovascular effect of normalizing the hematocrit level during erythropoietin therapy in predialysis patients with chronic renal failure. Am J Kidney Dis. 2000;35:250–6.
Locatelli F, Aljama P, Barany P, et al. Revised European best practice guidelines for the management of anaemia in patients with chronic renal failure. Nephrol Dial Transplant. 2004;19(Suppl 2):ii1–ii47.
KDOQI Clinical Practice Guidelines and Clinical Practice. Recommendations for anemia in chronic kidney disease. Am J Kidney Dis. 2006;47:S11–S145.
KDOQI Clinical Practice Guideline Clinical Practice. Recommendations for anemia in chronic kidney disease: 2007 update of hemoglobin target. Am J Kidney Dis. 2007;50:471–530.
McMurray JJV, Parfrey PS, Adamson JW, et al. KDIGO clinical practice guideline for anemia in chronic kidney disease. Kidney Int. 2012;2:279–335.
Gejyo F, Saito A, Akizawa T, et al. 2004 Japanese Society for Dialysis Therapy guidelines for renal anemia in chronic hemodialysis patients. Ther Apher Dial. 2004;8:443–59.
Tsubakihara Y, Nishi S, Akiba T, et al. 2008 Japanese Society for Dialysis Therapy: guidelines for renal anemia in chronic kidney disease. Ther Apher Dial. 2010;14:240–75.
Yamamoto H, Nishi S, Tomo T, et al. 2015 Japanes Society for Dialysis Therepy: guidelines for renal anemia in chronic kidney disease. Ren Replace Ther. 2017;3:1–46.
Akizawa T, Makino H, Matsuo S, et al. Management of anemia in chronic kidney disease patients: baseline findings from Chronic Kidney Disease Japan Cohort Study. Clin Exp Nephrol. 2011;15:248–57.
Panichi V, Rosati A, Bigazzi R, et al. Anaemia and resistance to erythropoiesis-stimulating agents as prognostic factors in haemodialysis patients: results from the RISCAVID study. Nephrol Dial Transplant. 2011;26:2641–8.
Johnson DW, Pascoe EM, Badve SV, et al. A randomized, placebo-controlled trial of pentoxifylline on erythropoiesis-stimulating agent hyporesponsiveness in anemic patients with CKD: the handling erythropoietin resistance with oxpentifylline (HERO) trial. Am J Kidney Dis. 2015;65:49–57.
Koibuchi K, Miyagi M, Arai T, et al. Comparing the efficacy of continuous erythropoietin receptor activator and darbepoetin Alfa treatments in Japanese patients with chronic kidney disease during the predialysis period: a propensity-matched analysis. Nephrology (Carlton). 2015;20(Suppl 4):22–8.
Kawahara K, Minakuchi J, Yokota N, et al. Treatment of renal anaemia with erythropoiesis-stimulating agents in predialysis chronic kidney disease patients: haemoglobin profile during the 6 months before initiation of dialysis. Nephrology (Carlton). 2015;20(Suppl 4):29–32.
Mohanram A, Zhang Z, Shahinfar S, et al. Anemia and end-stage renal disease in patients with type 2 diabetes and nephropathy. Kidney Int. 2004;66:1131–8.
Maggioni AP, Opasich C, Anand I, et al. Anemia in patients with heart failure: prevalence and prognostic role in a controlled trial and in clinical practice. J Card Fail. 2005;11:91–8.
Sabatine MS, Morrow DA, Giugliano RP, et al. Association of hemoglobin levels with clinical outcomes in acute coronary syndromes. Circulation. 2005;111:2042–9.
Tanaka T. Expanding roles of the hypoxia-response network in chronic kidney disease. Clin Exp Nephrol. 2016;20:835–44.
Maxwell PH, Eckardt KU. HIF prolyl hydroxylase inhibitors for the treatment of renal anaemia and beyond. Nat Rev Nephrol. 2016;12:157–68.
Acknowledgements
The following is a list of the institutions that participated in this study: Department of Nephrology (Kensei Yahata, Koichi Seta, Yuko Kikuchi, Mitsuteru Koizumi, Maki Murata), Diabetes Center (Shigeo Kono, Reiko Nakagauchi, Junichiro Kishi, Yuri Kira), Department of Cardiology (Nobutoyo Masunaga, Mitsuru Ishii, Moritake Iguchi, Takashi Unoki, Kensuke Takabayashi, Yasuhiro Hamatani), Department of Endocrinology and Metabolism (Tetsuya Tagami, Mika Tuiki, Maiko Kakita), National Hospital Organization Kyoto Medical Center; Tsuji Clinic (Hikari Tsuji); Soseikai General Hospital (Shogo Murakami, Tomoko Tagawa); Ohishi Naika Clinic (Mariko Ohishi); Tojinkai Hospital (Tetsuya Hashimoto, Toru Takatani); Yoda Clinic (Junzo Yoda); Koide Clinic (Ayako Koide); Shishioka Clinic (Ichio Shishioka); Tsukuda Clinic (Nobuhiro Tsukuda); Haba Clinic (Tetsunori Haba); Kuroda Clinic (Osamu Kuroda); Matsumura Clinic (Satoshi Matsumura); Wada Naika Clinic (Shigeo Wada); Ito Clinic (Yoshiaki Ohmori); Kitani Clinic (Keiko Kitani); Kimura Clinic (Fumiaki Kimura); Sugano Clinic (Hiroko Tanaka); Taniguchi Clinic (Yoko Taniguchi); Tamagaki Naika Clinic (Toshiyuki Tamagaki); Furuke Clinic (Keizo Furuke); Matsushita Clinic (Norio Matsushita).
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
The authors have declared that no conflicts of interest exist.
Ethical approval
All the procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee at which the studies were conducted (IRB approval number 12–43) and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
The study participants treated at Kyoto Medical Center provided written informed consent, and those treated at other hospitals or clinics had the opportunity to refuse inclusion in this study by posting their details.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The members of the Kyoto Fushimi Renal Anemia study investigators are listed in acknowledgements.
Electronic supplementary material
Below is the link to the electronic supplementary material.
About this article
Cite this article
Yahata, K., Seta, K., Kikuchi, Y. et al. Treatment for renal anemia and outcomes in non-dialysis patients with chronic kidney disease: the current status of regional medicine according to the Kyoto Fushimi Renal Anemia (KFRA) study. Clin Exp Nephrol 23, 1211–1220 (2019). https://doi.org/10.1007/s10157-019-01767-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10157-019-01767-w