Abstract
Background
Osmotic demyelination syndrome (ODS) is a complication generally associated with overly rapid correction of hyponatremia. Traditionally, nephrologists have been trained to focus solely on limiting the correction rate. However, there is accumulating evidence to suggest that the prevention of ODS is beyond achieving slow correction rates.
Methods
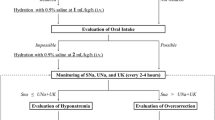
We (1) reviewed the literature for glial intracellular protective alterations during hyperosmolar stress, a state presumed equivalent to the rapid correction of hyponatremia, and (2) analyzed all available hyponatremia-associated ODS cases from PubMed for possible contributing factors including correction rates and concurrent metabolic disturbances involving hypokalemia, hypophosphatemia, hypomagnesemia, and/or hypoglycemia.
Results
In response to acute hyperosmolar stress, glial cells undergo immediate extracellular free water shift, followed by active intracellular Na+, K+ and amino acid uptake, and eventual idiogenic osmoles synthesis. At minimum, protective mechanisms require K+, Mg2+, phosphate, amino acids, and glucose. There were 158 cases of hyponatremia-associated ODS where both correction rates and other metabolic factors were documented. Compared with the rapid correction group (>0.5 mmol/L/h), the slow correction group (≤0.5 mmol/L/h) had a greater number of cases with concurrent hypokalemia (49.4 vs. 33.3 %, p = 0.04), and a greater number of cases with any concurrent metabolic derangements (55.8 vs. 38.3 %, p = 0.03).
Conclusion
Glial cell minimizes volume changes and injury in response to hyperosmolar stress via mobilization and/or utilization of various electrolytes and metabolic factors. The prevention of ODS likely requires both minimization of correction rate and optimization of intracellular response during the correction phase when a sufficient supply of various factors is necessary.


Similar content being viewed by others
References
McDowell ME, Wolf AV, Steer A. Osmotic volume of distribution: idiogenic changes in osmotic pressure associated with administration of hypertonic solutions. Am J Physiol. 1955;180:545–58.
Chan PH, Wong YP, Fishman RA. Hyperosmolality induced GABA release from rat brain slices. J Neurochem. 1978;30:1363–8.
Chan PH, Fishman RA. Elevation of rat brain amino acids, ammonia and idiogenic osmoles induced by hyperosmolality. Brain Res. 1979;161:293–301.
Pollock AS, Arieff AI. Abnormalities of cell volume regulation and their functional consequences. Am J Physiol. 1980;239(3):F195–205.
Heilig CW, Stromski ME, Blumenfeld JD, Lee JP, Gullans SR. Characterization of the major brain osmolytes that accumulate in salt-loaded rats. Am J Physiol (Renal Fluid Electrolyte Physiol). 1989;257:F1108–16.
Lien YHH, Shapiro JI, Chen L. Effects of hypernatremia on organic brain osmoles. J Clin Invest. 1990;85:1427–35.
Ayus JC, Armstrong DL, Arieff AI. Effects of hypernatraemia in the central nervous system and its therapy in rats and rabbits. J Physiol. 1996;492(Pt 1):243–55.
Adler S, Simplaceanu V. Effect of acute hyponatremia on rate brain pH and rat brain buffering. Am J Physiol. 1989;256:F113–9.
De Petris L, Luchetti A, Emma F. Cell volume regulation and transport mechanisms across the blood-brain barrier: implications for the management of hypernatraemic states. Eur J Pediatr. 2001;160:71–7.
Bito LZ, Myers RE. On the physiological response of the cerebral cortex to acute stress (reversible asphyxia). J Physiol (Lond). 1972;221:349–70.
Franchi-Gazzola R, Dall’Asta V, Sala R, et al. The role of the neutral amino acid transporter SNAT2 in cell volume regulation. Acta Physiol (Oxf). 2006;187:273–83.
Thurston JH, Hauhart RE, Dirgo JA, Schulz DW. Effects of acute hyperosmolar NaCl or urea on brain H2O, Na+, K+, carbohydrate, and amino acid metabolism in weanling mice: NaCl induces insulin secretion and hypoglycemia. Metab Brain Dis. 1986;1(2):129–46.
Vallurupalli S, Huesmann G, Gregory J, Jakoby MG IV. Levofloxacin-associated hypoglycaemia complicated by pontine myelinolysis and quadriplegia. Diabetic Med. 2008;25:856–9.
Madey JJ, Hannah JA, Lazaridis C. Central pontine myelinolysis following acute hypoglycemia. Clin Neurol Neurosurg. 2013;115(10):2299–300.
Hasegawa Y, Formato JE, Latour LL, et al. Severe transient hypoglycemia causes reversible change in the apparent diffusion coefficient of water. Stroke. 1996;27:1648–55.
Yan S, Rivkees SA. Hypoglycemia influences oligodendrocyte development and myelin formation. Neuroreport. 2006;17:55–9.
Suh WS, Gun ET, Hambu AM, Chan PH, Swanson RA. Hypoglycemic neuronal death is triggered by glucose reperfusion and activation of neuronal NADPH oxidase. J Clin Invest. 2007;117:910–8.
Thompson PD, Gledhill RF, Quinn NP, Rossor MN, Stanley P, Coomes EN. Neurological complications associated with parenteral treatment: central pontine myelinolysis and Wenicke’s encephalopathy. Br Med J. 1986;292(6521):684–5.
Sanders GT, Huijgen HJ, Sanders R. Magnesium in disease: a review with special emphasis on the serum ionized magnesium. Clin Chem Lab Med. 1999;37:1011–33.
King JD, Rosner MH. Osmotic demyelination syndrome. Am J Med Sci. 2010;339(6):561–7.
Adams RD, Victor M, Mancall EL. Central pontine myelinolysis: a hitherto undescribed disease occurring in alcoholic and malnourished patients. AMA Arch Neurol Psychiatry. 1959;81(2):154–72.
Khan LU, Ahmed J, Khan S, Macfie J. Refeeding syndrome: a literature review. Gastroenterol Res Pract 2011; Article ID 410971.
Lohr JW. Osmotic demyelination syndrome following correction of hyponatremia: association with hypokalemia. Am J Med. 1994;96(5):408–13.
Ruiz S, Alzieu M, Niquet L, Vergne S, Lathuile D, Campistron J. Severe hyponatraemia and central pontine myelinolysis: be careful with other factors! Ann Fr Anesth Reanim. 2009;28(1):96–9.
Turnbull J, Lumsden D, Siddigui A, Lin JP, Lim M. Osmotic demyelination syndrome associated with hypophosphataemia: 2 cases and a review of literature. Acta Paediatr. 2013;102:164–8.
Michell AW, Burn DJ, Reading PJ. Central pontine myelinolysis temporally related to hypophosphataemia. J Neurol Neurosurg Psychiatry. 2003;74:820.
Leens C, Mukendi R, Foret F, Hacourt A, Devuyst O, Colin IM. Central and extrapontine myelinolysis in a patient in spite of a careful correction of hyponatremia. Clin Nephrol. 2011;55(3):248–53.
Ramaekers VT, Reul J, Kusenbach G, Thron A, Heimann Gn. Central pontine myelinolysis associated with acquired folate depletion. Neuropediatrics. 1997;28(2):126–30.
Kishimoto Y, Ikeda K, Murata K, Kawabe K, Hirayama T, Iwasaki Y. Rapid development of central pontine myelinolysis after recovery from wernicke encephalopathy: a non-alcoholic case without hyponatremia. Intern Med. 2012;51(12):1599–603 Epub 2012 Jun 15.
An JY, Park SK, Han SR, Song IU. Central pontine and extrapontine myelinolysis that developed during alcohol withdrawal, without hyponatremia, in a chronic alcoholic. Intern Med. 2010;49(6):615–8 Epub 2010 Mar 15.
Brown RS. Potassium homeostasis and clinical implications. Am J Med. 1984;77(5A):3–10.
Ashrafian A, Davey P. A review of the causes of central pontine myelinosis: yet another apoptotic illness? Eur J Neurol. 2001;8(2):103–9.
Rose BD (ed): Clinical physiology of acid-base and electrolyte disorders (ed 4). New York, NY: McGraw-Hill; 1994. p. 679.
Edelman IS, Leibman J, O’meara MP, Birkenfeld LW. Interrelations between serum sodium concentration, serum osmolarity and total exchangeable sodium, total exchangeable potassium and total body water. J Clin Invest. 1958;37(9):1236–56.
Laragh JH. The effect of potassium chloride on hyponatremia. J Clin Invest. 1954;33(5):807–18.
Pham PC, Chen PV, Pham PT. Over-correction of hyponatremia: where do we go wrong? Am J Kidney Dis. 2000;36(2):E12.
Madhusooman S, Bogunovic OJ, Moise D, Brenner R, Markowitz S, Sotelo J. Hyponatremia associated with psychotropic medications: a review of the literature and spontaneous reports. Advers Drug React Toxicol Rev. 2002;21:17–29.
Wilkinson TJ, Begg EJ, Winter AC, Sainsbury R. Incidence of risk factors for hyponatraemia following treatment with fluoxetine or paroxetine in elderly people. Br J Clin Pharmacol. 1999;47:211–7.
Almond CSD, Shin AY, Fortescue EB, et al. Hyponatremia among runners in the Bostom Marathon. N Engl J Med. 2005;352:1550–6.
Conflict of interest
The authors declare no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Pham, PM.T., Pham, PA.T., Pham, S.V. et al. Correction of hyponatremia and osmotic demyelinating syndrome: have we neglected to think intracellularly?. Clin Exp Nephrol 19, 489–495 (2015). https://doi.org/10.1007/s10157-014-1021-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10157-014-1021-y