Abstract
Background
Hyperuricemia and metabolic acidosis have emerged as important risk factors for progression of kidney disease. In this study, we aimed to investigate the effects of allopurinol on metabolic acidosis and endothelial functions in hyperuricemic stage 2–4 chronic kidney disease (CKD) patients.
Methods
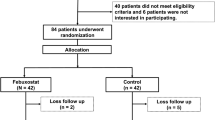
Thirty patients with stage 2–4 CKD and serum uric acid levels over 5.5 mg/dl were included in the study group. They were prescribed 300 mg/day per oral allopurinol treatment for three months. Age- and gender-matched CKD patients (n = 30) with similar clinical characteristics were taken as the control group and were not given allopurinol treatment. Endothelial functions were measured via flow-mediated dilatation (∆FMD %) over the forearm. pH and HCO3 levels in venous blood, Cr clearance and proteinuria levels were calculated in all patients at baseline and in the third month.
Results
Serum uric acid levels significantly decreased in the study group from 7.9 ± 1.6 to 6.4 ± 1.7 (p < 0.001). Cr clearance (from 43.4 ± 20.1 to 51.4 ± 24.9, p = 0.011), serum bicarbonate levels (from 21.4 ± 3.4 to 23.0 ± 3.4, p = 0.007) and ΔFMD % values (from 5.8 ± 2.5 to 6.2 ± 2.7, p = 0.006) increased significantly in the allopurinol group. There were no significant changes except for ∆FMD % values (decreased from 6.27 ± 1.62 to 5.71 ± 1.90, p = 0.005) in the control group. ∆FMD % variations within the two groups were clearly significant in the repeated ANOVA general linear model.
Conclusion
We assume that decreasing uric acid levels with allopurinol treatment seems to be helpful in restoring endothelial functions, preventing metabolic acidosis and slowing down the progression of CKD.

Similar content being viewed by others
References
Goicoechea M, de Vinuesa SG, Verdalles U, Ruiz-Caro C, Ampuero J, Rincón A, et al. Effect of allopurinol in chronic kidney disease progression and cardiovascular risk. Clin J Am Soc Nephrol. 2010;5:1388–93.
Edwards NL. The role of hyperuricemia and gout in kidney and cardiovascular disease. Clev Clin J Med. 2008;75:13–6.
Saito T, Mochizuki T, Uchida K, Tsuchiya K, Nitta K. Metabolic syndrome and risk of progression of chronic kidney disease: a single-center cohort study in Japan. Heart Vessels. 2013;28:323–9.
Sundström J, Sullivan L, D’Agostino RB, Levy D, Kannel WB, Vasan RS. Relations of serum uric acid to longitudinal blood pressure tracking and hypertension incidence. Hypertension. 2005;45:28–33.
Chonchol M, Shlipak MG, Katz R, Sarnak MJ, Newman AB, Siscovick DS, et al. Relationship of uric acid with progression of kidney disease. Am J Kidney Dis. 2007;50:239–47.
Feig DI, Kang DH, Johnson RJ. Uric acid and cardiovascular risk. N Engl J Med. 2008;359:1811–21.
Kanbay M, Yilmaz MI, Sonmez A, Turgut F, Saglam M, Cakir E, et al. Serum uric acid level and endothelial dysfunction in patients with nondiabetic chronic kidney disease. Am J Nephrol. 2011;33:298–304.
Kawashima M, Wada K, Ohta H, Terawaki H, Aizawa Y. Association between asymptomatic hyperuricemia and new-onset chronic kidney disease in Japanese male workers: a long-term retrospective cohort study. BMC Nephrol. 2011;12:1–7.
Miyaoka T, Mochizuki T, Takei T, Tsuchiya K, Nitta K. Serum uric acid levels and long-term outcomes in chronic kidney disease. Heart Vessels. 2013. doi:10.1007/s00380-013-0396-0.
Pai BH, Swarnalatha G, Ram R, Dakshinamurty KV. Allopurinol for prevention of progression of kidney disease with hyperuricemia. Indian J Nephrol. 2013;23:280–6.
Kanbay M, Ozkara A, Selcoki Y, Isik B, Turgut F, Bavbek N, et al. Effect of treatment of hyperuricemia with allopurinol on blood pressure, creatinine clearance, and proteinuria in patients with normal renal functions. Int Urol Nephrol. 2007;39:1227–33.
Ruggiero C, Cherubini A, Ble A, Bos AJ, Maggio M, Dixit VD, et al. Uric acid and inflammatory markers. Eur J Heart. 2006;27:1174–81.
Khosla UM, Zharikov S, Finch JL, Nakagawa T, Roncal C, Mu W, et al. Hyperuricemia induces endothelial dysfunction. Kidney Int. 2005;67:1739–42.
George J, Carr E, Davies J, Belch JJ, Struthers A. High-dose allopurinol improves endothelial function by profoundly reducing vascular oxidative stress and not by lowering uric acid. Circulation. 2006;114:2508–16.
Gustafsson D, Unwin R. The pathophysiology of hyperuricaemia and its possible relationship to cardiovascular disease, morbidity and mortality. BMC Nephrol. 2013;14:164.
Sincer I, Kurtoglu E, Calıskan M, Akkaya E, Vuruskan E, Küçükosmanoglu M, et al. Significant correlation between uric acid levels and flow-mediated dilatation in patients with masked hypertension. Clin Exp Hypertens. 20 Feb 2014 [Epub ahead of print]. doi:10.3109/10641963.2013.827694.
Williams B, Hattersley J, Layward E, Walls J. Metabolic acidosis and skeletal muscle adaptation to low-protein diets in chronic uremia. Kidney Int. 1991;40:779–86.
de Brito-Ashurst I, Varagunam M, Raftery MJ, Yaqoob MM. Bicarbonate supplementation slows progression of CKD and improves nutritional status. J Am Soc Nephrol. 2009;20:2075–84.
Phisitkul S, Khanna A, Simoni J, Broglio K, Sheather S, Rajab MH, et al. Amelioration of metabolic acidosis in individuals with low GFR reduces kidney endothelin production, reduces kidney injury, and better preserves GFR. Kidney Int. 2010;77:617–23.
Gao H, Lew SQ, Bosch JP. Moderate metabolic acidosis and its effects on serum parameters in hemodialysis patients. Nephron. 2000;86:135–8.
Moviat M, Terpstra AM, Ruitenbeek W, Kluijtmans LA, Pickkers P, van der Hoeven JG. Contribution of various metabolites to the unmeasured anions in critically ill patients with metabolic acidosis. Crit Care Med. 2008;36:752–8.
Forni LG, McKinnon W, Lord GA, Treacher DF, Peron JM, Hilton PJ. Circulating anions usually associated with the Krebs cycle in patients with metabolic acidosis. Crit Care. 2005;9:R591–5.
Vazquez-Mellado J, Morales EM, Pacheco-Tena C, Burgos-Vargas R. Relation between adverse events associated with allopurinol and renal function in patients with gout. Ann Rheum Dis. 2001;60:981–3.
Paisansinsup T, Breitenstein MK, Schousboe JT. Association between adverse reactions to allopurinol and exposures to high maintenance doses: implications for management of patients using allopurinol. J Clin Rheumatol. 2013;19:180–6.
Dalbeth N, Kumar S, Stamp L, Gow P. Dose adjustment of allopurinol according to creatinine clearance does not provide adequate control of hyperuricemia in patients with gout. J Rheumatol. 2006;33:1646–50.
Conflict of interest
We have no financial disclosures to declare and no conflicts of interest to report.
Author information
Authors and Affiliations
Corresponding author
Additional information
Trial registration number: ACTRN12614000320651, Australian New Zealand Clinical Trials Registry (ANZCTR).
About this article
Cite this article
Bayram, D., Tuğrul Sezer, M., İnal, S. et al. The effects of allopurinol on metabolic acidosis and endothelial functions in chronic kidney disease patients. Clin Exp Nephrol 19, 443–449 (2015). https://doi.org/10.1007/s10157-014-1012-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10157-014-1012-z