Abstract
Background
Evidence on early closure (EC) of defunctioning stoma (DS) after colorectal surgery shows a favorable effect when patients are carefully selected. Therefore, a clinical pathway adapted to the implementation of an EC strategy was developed in our center. The aim of this study was to carry out a comparative analysis of time until DS closure and DS-related morbidity before and after the implementation of an EC protocol (ECP).
Methods
This study is a before-and-after comparative analysis. Patients were divided into two cohorts according to the observational period: patients from the period before the ECP implementation (January 2015–December 2019) [Period 1] and those from the period after that (January 2020–December 2022) [Period 2]. All consecutive patients subjected to elective DS closure within both periods were eligible. Early closure was defined as the reversal within 30 days from DS creation. Patients excluded from EC or those not closed within 30 days since primary surgery were analyzed as late closure (LC). Baseline characteristics and DS-related morbidity were recorded.
Results
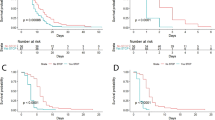
A total of 145 patients were analyzed. Median time with DS was shorter in patients after ECP implementation [42 (21–193) days versus 233 (137–382) days, p < 0.001]. This reduction in time to closure did not impact the DS closure morbidity and resulted in less DS morbidity (68.8% versus 49.2%, p = 0.017) and fewer stoma nurse visits (p = 0.029).
Conclusions
The ECP was able to significantly reduce intervals to restoration of bowel continuity in patients with DS, which in turn resulted in a direct impact on the reduction of DS morbidity without negatively affecting DS closure morbidity.



Similar content being viewed by others
Data availability
The datasets generated and analyzed during the current study are available from the corresponding author on reasonable request.
References
Mu Y, Zhao L, He H, Zhao H, Li J (2021) The efficacy of ileostomy after laparoscopic rectal cancer surgery: a meta-analysis. World J Surg Onc 19(1):318
Matthiessen P, Hallböök O, Rutegård J, Simert G, Sjödahl R (2007) Defunctioning stoma reduces symptomatic anastomotic leakage after low anterior resection of the rectum for cancer: a randomized multicenter trial. Ann Surg 246(2):207–214
Yang M, McClure JA, Wanis KN, Vogt KN, Van Koughnett JAM, Ott MC et al. (2022) From formation to closure: aggregate morbidity and mortality associated with defunctioning loop ileostomies. Dis Colon Rectum 65(9):1135–1142
Vogel I, Reeves N, Tanis PJ, Bemelman WA, Torkington J, Hompes R et al. (2021) Impact of a defunctioning ileostomy and time to stoma closure on bowel function after low anterior resection for rectal cancer: a systematic review and meta-analysis. Tech Coloproctol 25(7):751–760
Robertson J, Linkhorn H, Vather R, Jaung R, Bissett IP (2015) Cost analysis of early versus delayed loop ileostomy closure: a case-matched study. Dig Surg 32(3):166–172
Herrle F, Sandra-Petrescu F, Weiss C, Post S, Runkel N, Kienle P (2016) Quality of life and timing of stoma closure in patients with rectal cancer undergoing low anterior resection with diverting stoma: a multicenter longitudinal observational study. Dis Colon Rectum 59(4):281–290
Rubio-Perez I (2014) Increased postoperative complications after protective ileostomy closure delay: an institutional study. WJGS 6(9):169
Climent M, Frago R, Cornellà N, Serrano M, Kreisler E, Biondo S (2022) Prognostic factors for complications after loop ileostomy reversal. Tech Coloproctol 26(1):45–52
Barenboim A, Geva R, Tulchinsky H (2022) Revised risk factors and patient characteristics for failure to close a defunctioning ileostomy following low anterior resection for locally advanced rectal cancer. Int J Colorectal Dis 37(7):1611–1619
Hoshino N, Hida K, Fukui Y, Takahashi Y, Nakayama T, Obama K (2022) Relationship between diverting stoma and adjuvant chemotherapy in patients with rectal cancer: a nationwide study using the national database of health insurance claims and specific health checkups of Japan. Int J Clin Oncol 27(3):545–552
Cheng HH, Shao YC, Lin CY, Chiang TW, Chen MC, Chiu TY et al. (2023) Impact of chemotherapy on surgical outcomes in ileostomy reversal: a propensity score matching study from a single centre. Tech Coloproctol. https://doi.org/10.1007/s10151-023-02790-6
Podda M, Coccolini F, Gerardi C, Castellini G, Wilson MSJ, Sartelli M et al. (2022) Early versus delayed defunctioning ileostomy closure after low anterior resection for rectal cancer: a meta-analysis and trial sequential analysis of safety and functional outcomes. Int J Colorectal Dis 37(4):737–756
Vogel I, Vaughan-Shaw PG, Gash K, Withers KL, Carolan-Rees G, Thornton M et al. (2022) Improving the time to ileostomy closure following an anterior resection for rectal cancer in the UK. Colorectal Dis 24(1):120–127
Dukes’ Club Research Collaborative, Chambers A, Stearns A, Walsh A, Rankin A, Khan A et al. (2021) Factors impacting time to ileostomy closure after anterior resection: the UK closure of ileostomy timing cohort study (CLOSE-IT). Colorectal Dis 23(5):1109–1119
O’Sullivan NJ, Temperley HC, Nugent TS, Low EZ, Kavanagh DO, Larkin JO et al. (2022) Early vs. standard reversal ileostomy: a systematic review and meta-analysis. Tech Coloproctol 26(11):851–862
Danielsen AK, Park J, Jansen JE, Bock D, Skullman S, Wedin A et al. (2017) Early closure of a temporary ileostomy in patients with rectal cancer: a multicenter randomized controlled trial. Ann Surg 265(2):284–290
Hajibandeh S, Hajibandeh S, Kennedy-Dalby A, Rehman S, Zadeh RA (2018) Purse-string skin closure versus linear skin closure techniques in stoma closure: a comprehensive meta-analysis with trial sequential analysis of randomised trials. Int J Colorectal Dis 33(10):1319–1332
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240(2):205–213
NBOCA-annual-report-2017-v2.pdf
Menahem B, Lubrano J, Vallois A, Alves A (2018) Early closure of defunctioning loop ileostomy: is it beneficial for the patient? A meta-analysis. World J Surg 42(10):3171–3178
Walma MS, Kornmann VNN, Boerma D, de Roos MAJ, van Westreenen HL (2015) Predictors of fecal incontinence and related quality of life after a total mesorectal excision with primary anastomosis for patients with rectal cancer. Ann Coloproctol 31(1):23
Park J, Angenete E, Bock D, Correa-Marinez A, Danielsen AK, Gehrman J et al. (2020) Cost analysis in a randomized trial of early closure of a temporary ileostomy after rectal resection for cancer (EASY trial). Surg Endosc 34(1):69–76
Caminsky NG, Moon J, Morin N, Alavi K, Auer RC, Bordeianou LG et al. (2023) Patient and surgeon preferences for early ileostomy closure following restorative proctectomy for rectal cancer: why aren’t we doing it? Surg Endosc 37(1):669–682
Lindner S, Eitelbuss S, Hetjens S, Gawlitza J, Hardt J, Seyfried S et al. (2021) Less is more—the best test for anastomotic leaks in rectal cancer patients prior to ileostomy reversal. Int J Colorectal Dis 36(11):2387–2398
Chand M, Nash GF, Talbot RW (2008) Timely closure of loop ileostomy following anterior resection for rectal cancer. Eur J Cancer Care. https://doi.org/10.1111/j.1365-2354.2008.00972.x
Panis Y (2021) Early stoma closure after rectal resection for cancer: still a matter of debate? Dis Colon Rectum 64(11):1303–1304
Bakx R, Busch ORC, Van Geldere D, Bemelman WA, Slors JFM, Van Lanschot JJB (2003) Feasibility of early closure of loop ileostomies: a pilot study. Dis Colon Rectum 46(12):1680–1684
Alves A, Panis Y, Lelong B, Dousset B, Benoist S, Vicaut E (2008) Randomized clinical trial of early versus delayed temporary stoma closure after proctectomy. Br J Surg 95(6):693–698
Dimitriou N, Panteleimonitis S, Dhillon A, Boyle K, Norwood M, Hemingway D et al. (2015) Is the routine use of a water-soluble contrast enema prior to closure of a loop ileostomy necessary? A review of a single institution experience. World J Surg Onc 13(1):331
Elsner AT, Brosi P, Walensi M, Uhlmann M, Egger B, Glaser C et al. (2021) Closure of temporary ileostomy 2 versus 12 weeks after rectal resection for cancer: a word of caution from a prospective, randomized controlled multicenter trial. Dis Colon Rectum 64(11):1398–1406
Kitaguchi D, Enomoto T, Ohara Y, Owada Y, Hisakura K, Akashi Y et al. (2020) Exploring optimal examination to detect occult anastomotic leakage after rectal resection in patients with diverting stoma. BMC Surg 20(1):53
Koc MA, Akyol C, Gokmen D, Aydin D, Erkek AB, Kuzu MA (2023) Effect of prehabilitation on stoma self-care, anxiety, depression, and quality of life in patients with stomas: a randomized controlled trial. Dis Colon Rectum 66(1):138–147
Calderillo-Ruíz G, López-Basave HN, Muñoz-Montaño WR, Díaz-Romero MC, Carbajal-López B, Castillo-Morales C et al. (2023) Impact of ileostomy in the adjuvant treatment and outcome of colon cancer. Int J Colorectal Dis 38(1):158
Acknowledgements
We thank Manuel Gómez Gutiérrez from Instituto de Investigación Sanitaria Princesa (IIS-IP) for professional English editing of the manuscript.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by LBT, LDB, and ACB. The first draft of the manuscript was written by LBT and CCS and all authors commented on the different versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
Authors declare no conflicts of interest.
Ethical approval
All the procedures performed complied with the rules of the institutional and/or national research ethics committees and with the Declaration of Helsinki of 1964 and its later modifications or similar ethics rules. The study was approved by the Clinical Research Ethics Committee (CREC) of our institution (registry number 4390) in February 2021.
Informed consent
The authors declare that informed consent was obtained from all individual participants for whom identifying information is included in this article.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Blanco Terés, L., Cerdán Santacruz, C., Correa Bonito, A. et al. Early diverting stoma closure is feasible and safe: results from a before-and-after study on the implementation of an early closure protocol at a tertiary referral center. Tech Coloproctol 28, 32 (2024). https://doi.org/10.1007/s10151-023-02905-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10151-023-02905-z