Abstract
Purpose
Rectal cancer surgery presents challenges in achieving good oncological results and preserving functional outcomes. Different surgical approaches, including open, laparoscopic, robotic and transanal techniques, have been employed, but there is a lack of consensus on the optimal approach, particularly in terms of functional results. This study aims to assess bowel function and to compare outcomes of patients that had undergone surgery for mid-low rectal cancer across different surgical approaches.
Method
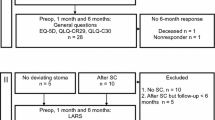
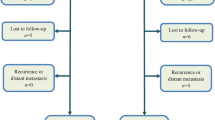
This is an international, multicentre, prospective cohort study. Inclusion criteria are patients diagnosed with rectal cancer below the peritoneal reflection, eligible for different surgical approaches for total mesorectal excision (TME). Data will be collected using validated questionnaires assessing bowel, sexual and urinary function, and quality of life (QOL). Secondary outcomes include short-term postoperative results. Data will be collected at baseline and 6, 12 and 24 months after index surgery or stoma reversal surgery.
Conclusion
This study will provide insights into the impact of different approaches for TME on bowel, sexual and urinary function, and overall QOL of patients undergoing rectal cancer surgery. The findings will provide important information to optimise the surgical strategy and to improve patient care in this population.
Trial registration
ClinicalTrials.gov, NCT04936581 (registered 23 June 2021).

Similar content being viewed by others
Data availability
The datasets used and/or analysed during the current study will be available from the corresponding author on request.
References
Guillou PJ, Quirke P, Thorpe H et al (2005) Short-term endpoints of conventional versus laparoscopic-assisted surgery in patients with colorectal cancer (MRC CLASICC trial): multicentre, randomised controlled trial. Lancet 365:1718–1726
Bonjer HJ, Deijen CL, Haglind E, COLOR II Study Group (2015) A randomized trial of laparoscopic versus open surgery for rectal cancer. N Engl J Med 2015(373):194
Heald RJ (1988) The ‘Holy Plane’ of rectal surgery. J R Soc Med 81:503–508
European Society of Coloproctology (ESCP) collaborating group (2018) An international multicentre prospective audit of elective rectal cancer surgery; operative approach versus outcome, including transanal total mesorectal excision (taTME). Colorectal Dis 20(Suppl 6):33–46
Sylla P, Rattner DW, Delgado S, Lacy AM (2010) NOTES transanal rectal cancer resection using transanal endoscopic microsurgery and laparoscopic assistance. Surg Endosc 24:1205–1210
Wasmuth HH, Faerden AE, Myklebust TÅ et al (2020) Transanal total mesorectal excision for rectal cancer has been suspended in Norway. Br J Surg 107:121–130
Van Der Heijden JAG, Qaderi SM, Verhoeven R et al (2012) Transanal total mesorectal excision and low anterior resection syndrome. Br J Surg 108(8):991–997
Sun R, Dai Z, Zhang Y, Lu J, Zhang Y, Xiao Y (2021) The incidence and risk factors of low anterior resection syndrome (LARS) after sphincter-preserving surgery of rectal cancer: a systematic review and meta-analysis. Support Care Cancer 1:3. https://doi.org/10.1007/s00520-021-06326-2
Burch J, Taylor C, Wilson A, Norton C (2021) Symptoms affecting quality of life after sphincter-saving rectal cancer surgery: a systematic review. Eur J Oncol Nurs 52:101934
Christensen P, Im Baeten C, Espín-Basany E et al (2021) Management guidelines for low anterior resection syndrome-the MANUEL project. Colorectal Dis 23:461–475
Li K, He X, Tong S, Zheng Y (2021) Risk factors for sexual dysfunction after rectal cancer surgery in 948 consecutive patients: a prospective cohort study. Eur J Surg Oncol 47:2087–2092
Calvert M, Kyte D, Mercieca-Bebber R, Slade A, Chan A-W, King MT (2018) Guidelines for inclusion of patient-reported outcomes in clinical trial protocols the SPIRIT-PRO Extension. JAMA 319:483–494
Keane C, Fearnhead NS, Bordeianou L et al. International consensus definition of low anterior resection syndrome. https://doi.org/10.1111/codi.14957
Emmertsen KJ, Laurberg S (2012) Low anterior resection syndrome score: development and validation of a symptom-based scoring system for bowel dysfunction after low anterior resection for rectal cancer. Ann Surg 255:922–928
Vaizey CJ, Carapeti E, Cahill JA, Kamm MA (1999) Prospective comparison of faecal incontinence grading systems. Gut 44:77–80
Rosen RC, Riley A, Wagner G, Osterloh IH, Kirkpatrick J, Mishra A (1997) The international index of erectile function (IIEF): a multidimensional scale for assessment of erectile dysfunction. Urology 49:822–830
Rosen R, Brown C, Heiman J et al (2000) The female sexual function index (FSFI): a multidimensional self-report instrument for the assessment of female sexual function. J Sex Marital Ther 26:191–208
Barry MJ, Fowler FJ, O’Leary MP et al (1992) The American Urological Association symptom index for benign prostatic hyperplasia. The Measurement Committee of the American Urological Association. J Urol 148:1549–1557
Bjordal K, de Graeff A, Fayers PM et al (2000) A 12 country field study of the EORTC QLQ-C30 (version 3.0) and the head and neck cancer specific module (EORTC QLQ-H&N35) in head and neck patients. EORTC quality of life group. Eur J Cancer 36:1796–1807
Gujral S, Conroy T, Fleissner C et al (2007) Assessing quality of life in patients with colorectal cancer: an update of the EORTC quality of life questionnaire. Eur J Cancer 43:1564–1573
Bryant CLC, Lunniss PJ, Knowles CH, Thaha MA, Chan CLH (2012) Anterior resection syndrome. Lancet Oncol 13:e403–e408
Sun W, Dou R, Chen J et al (2019) Impact of long-course neoadjuvant radiation on postoperative low anterior resection syndrome and quality of life in rectal cancer: post hoc analysis of a randomized controlled trial. Ann Surg Oncol 26:746–755
Croese AD, Lonie JM, Trollope AF, Vangaveti VN, Ho Y-H (2018) A meta-analysis of the prevalence of low anterior resection syndrome and systematic review of risk factors. Int J Surg 56:234–241
van der Heijden JW, Koëter T et al (2020) Functional complaints and quality of life after transanal total mesorectal excision: a meta-analysis. Br J Surg. https://doi.org/10.1002/bjs.11566
Choy KW, Yang TWW, Prabhakaran S, Heriot AG, Kong JC, Warrier SK (2021) Comparing functional outcomes between transanal total mesorectal excision (taTME) and laparoscopic total mesorectal excision (LaTME) for rectal cancer: a systematic review and meta-analysis. Int J Colorectal Dis. https://doi.org/10.1007/s00384-021-03849-2
Li X, Wang T, Yao L et al (2017) The safety and effectiveness of robot-assisted versus laparoscopic TME in patients with rectal cancer. Medicine 96:e7585
Kim JY, Kim N-K, Lee KY, Hur H, Min BS, Kim JH (2012) A comparative study of voiding and sexual function after total mesorectal excision with autonomic nerve preservation for rectal cancer: laparoscopic versus robotic surgery. Ann Surg Oncol 19:2485–2493
Kim HJ, Choi G-S, Park JS, Park SY, Yang CS, Lee HJ (2018) The impact of robotic surgery on quality of life, urinary and sexual function following total mesorectal excision for rectal cancer: a propensity score-matched analysis with laparoscopic surgery. Colorectal Dis 20:O103–O113
Park SY, Choi G-S, Park JS, Kim HJ, Ryuk J-P, Yun S-H (2014) Urinary and erectile function in men after total mesorectal excision by laparoscopic or robot-assisted methods for the treatment of rectal cancer: a case-matched comparison. World J Surg 38:1834–1842
Andolfi C, Umanskiy K (2019) Appraisal and current considerations of robotics in colon and rectal surgery. J Laparoendosc Adv Surg Tech A 29:152–158
Alimova I, Chernyshov S, Nagudov MA, Rybakov E (2021) Comparison of oncological and functional outcomes and quality of life after transanal or laparoscopic total mesorectal excision for rectal cancer: a systematic review and meta-analysis. Tech Coloproctol. https://doi.org/10.1007/s10151-021-02420-z
Funding
No funding.
Author information
Authors and Affiliations
Consortia
Contributions
PT and CP contributed equally in analysing the data and writing the manuscript. The rest of the authors critically revised the paper for important intellectual content. All authors have contributed to the work and agreed on the final version.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving humans were in accordance with ethical standards of the institutional research committee and the 1964 Helsinki declaration and its later amendments.
Informed consent
Informed consent was obtained from all participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Tejedor, P., Arredondo, J., Pellino, G. et al. Patient Reported Outcomes following Cancer of the Rectum (PROCaRe): protocol of a prospective multicentre international study. Tech Coloproctol 27, 1345–1350 (2023). https://doi.org/10.1007/s10151-023-02865-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10151-023-02865-4