Abstract
Purpose
The importance of lateral pelvic lymph node dissection (LLND) for advanced low rectal cancer is gradually being recognized in Europe and the USA, where some patients were affected by uncontrolled lateral pelvic lymph node (LLNs) metastasis, even after total mesorectal excision (TME) with neoadjuvant chemoradiotherapy (CRT). The purpose of this study was thus to compare robotic LLND (R-LLND) with laparoscopic (L-LLND) to clarify the safety and advantages of R-LLND.
Methods
Sixty patients were included in this single-institution retrospective study between January 2013 and July 2022. We compared the short-term outcomes of 27 patients who underwent R-LLND and 33 patients who underwent L-LLND.
Results
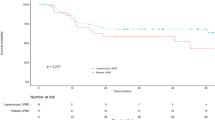
En bloc LLND was performed in significantly more patients in the R-LLND than in the L-LLND group (48.1% vs. 15.2%; p = 0.006). The numbers of LLNs on the distal side of the internal iliac region (LN 263D) harvested were significantly higher in the R-LLND than in the L-LLND group (2 [0–9] vs. 1 [0–6]; p = 0.023). The total operative time was significantly longer in the R-LLND than in the L-LLND group (587 [460–876] vs. 544 [398–859]; p = 0.003); however, the LLND time was not significantly different between groups (p = 0.718). Postoperative complications were not significantly different between the two groups.
Conclusion
The present study clarified the safety and technical feasibility of R-LLND with respect to L-LLND. Our findings suggest that the robotic approach offers a key advantage, allowing significantly more LLNs to be harvested from the distal side of the internal iliac region (LN 263D). Prospective clinical trials examining the oncological superiority of R-LLND are thus necessary in the near future.



Similar content being viewed by others
Data Availability
All data were obtained from medical records.
References
Kapiteijn E, Marijnen CA, Colenbrander AC et al (1998) Local recurrence in patients with rectal cancer diagnosed between 1988 and 1992: a population-based study in West Netherlands. Eur J Surg Oncol 24:528–535
Heald RJ, Husband EM, Ryall RD (1982) The mesorectum in rectal cancer surgery–the clue to pelvic recurrence? Br J Surg 69:613–616
Cedermark B, Dahlberg M, Glimelius B, Påhlman L, Rutqvist LE, Wilking N (1997) Swedish Rectal Cancer Trial. Improved survival with preoperative radiotherapy in resectable rectal cancer. N Engl J Med 336:980–987
Kapiteijn E, Marijnen CA, Nagtegaal ID et al (2001) Dutch Colorectal Cancer Group. Preoperative radiotherapy combined with total mesorectal excision for resectable rectal cancer. N Engl J Med 345:638–646
Sauer R, Becker H, Hohenberger W et al (2004) German Rectal Cancer Study Group. Preoperative versus postoperative chemoradiotherapy for rectal cancer. N Engl J Med 351:1731–1740
Kusters M, Beets GL, van de Velde CJ et al (2009) A comparison between the treatment of low rectal cancer in Japan and the Netherlands, focusing on the patterns of local recurrence. Ann Surg 249:229–235
Kim NK, Kim MJ, Park JK, Park SI, Min JS (2000) Preoperative staging of rectal cancer with MRI: accuracy and clinical usefulness. Ann Surg Oncol 7:732–737
Kim TG, Park W, Choi DH et al (2014) Factors associated with lateral pelvic recurrence after curative resection following neoadjuvant chemoradiotherapy in patients with rectal cancer. Int J Colorectal Dis 29:193–200
Ogura A, Konishi T, Beets GL et al (2019) Lateral Node Study Consortium. Lateral nodal features on restaging magnetic resonance imaging associated with lateral local recurrence in low rectal cancer after neoadjuvant chemoradiotherapy or radiotherapy. JAMA Surg 154:e192172. https://doi.org/10.1001/jamasurg.2019.2172
Hashiguchi Y, Muro K, Saito Y et al (2020) Japanese Society for Cancer of the Colon and Rectum (JSCCR) guidelines 2019 for the treatment of colorectal cancer. Int J Clin Oncol 25:1–42
Fujita S, Mizusawa J, Kanemitsu Y et al (2017) Colorectal Cancer Study Group of Japan Clinical Oncology Group. Mesorectal excision with or without lateral lymph node dissection for clinical stage II/III lower rectal cancer (JCOG0212): a multicenter, randomized controlled, noninferiority trial. Ann Surg 266:201–207
Ogura A, Konishi T, Cunningham C et al. Neoadjuvant (chemo)radiotherapy with total mesorectal excision only is not sufficient to prevent lateral local recurrence in enlarged nodes: results of the multicenter lateral node study of patients with low cT3/4 rectal cancer. J Clin Oncol 37:33–43
Georgiou P, Tan E, Gouvas N et al (2009) Extended lymphadenectomy versus conventional surgery for rectal cancer: a meta-analysis. Lancet Oncol 10:1053–1062
Yamaguchi T, Kinugasa Y, Shiomi A, Tomioka H, Kagawa H (2016) Robotic-assisted laparoscopic versus open lateral lymph node dissection for advanced lower rectal cancer. Surg Endosc 30:721–728
Nagayoshi K, Ueki T, Manabe T et al (2016) Laparoscopic lateral pelvic lymph node dissection is achievable and offers advantages as a minimally invasive surgery over the open approach. Surg Endosc 30:1938–1947
Morohashi H, Sakamoto Y, Miura T et al (2021) Short-term outcomes of robotic-assisted laparoscopic versus laparoscopic lateral lymph node dissection for advanced lower rectal cancer. Surg Endosc 35:5001–5008
Shiomi A, Kinugasa Y, Yamaguchi T, Tomioka H, Kagawa H (2014) Robot-assisted rectal cancer surgery: short-term outcomes for 113 consecutive patients. Int J Colorectal Dis 29:1105–1111
Ishizaki T, Mazaki J, Enomoto M et al (2022) A new technique for robotic lateral pelvic lymph node dissection for advanced low rectal cancer with emphasis on en bloc resection and inferior vesical vessel preservation. Surg Endosc 236:7789–7793
Ishizaki T, Mazaki J, Enomoto M et al (2022) Intracorporeal delta-shaped anastomosis without suturing technique in laparoscopic colectomy using a linear stapling device with bioabsorbable polyglycolic acid sheet. Tech Coloproctol 26:593–594
Cheeseman SL, Joel SP, Chester JD et al (2002) A “modified de Gramont” regimen of fluorouracil, alone and with oxaliplatin, for advanced colorectal cancer. Br J Cancer 87:393–399
Cassidy J, Clarke S, Díaz-Rubio E et al (2008) Randomized phase III study of capecitabine plus oxaliplatin compared with fluorouracil/folinic acid plus oxaliplatin as first-line therapy for metastatic colorectal cancer. J Clin Oncol 26:2006–2012
Zhou S, Jiang Y, Pei W, Zhou H, Liang J, Zhou Z (2021) Neoadjuvant chemoradiotherapy followed by lateral pelvic lymph node dissection for rectal cancer patients: a retrospective study of its safety and indications. J Surg Oncol 124:354–360
Torous VF, Oliva E (2021) On the new (version 9) American Joint Committee on Cancer tumor, node, metastasis staging for cervical cancer—a commentary. Cancer Cytopathol 129:581–582
Sakai Y, Kitano S (2015) Practice guidelines on endoscopic surgery for qualified surgeons by the endoscopic surgical skill qualification system. Asian J Endosc Surg 8:103–113
Sugihara K, Kusunoki M, Watanabe T, Sakai Y, Sekimoto M, Ajioka Y (2018) Japanese classification of colorectal carcinoma. In: Japanese Research Society for Cancer of the Colon and Rectum, 3rd ed. Kanehara Shuppan, Tokyo
Yamaguchi T, Konishi T, Kinugasa Y et al (2017) Laparoscopic versus open lateral lymph node dissection for locally advanced low rectal cancer: a subgroup analysis of a large multicenter cohort study in Japan. Dis Colon Rectum 60:954–964
Kagawa H, Kinugasa Y, Shiomi A et al (2015) Robotic-assisted lateral lymph node dissection for lower rectal cancer: short-term outcomes in 50 consecutive patients. Surg Endosc 29:995–1000
Kanemitsu Y, Komori K, Shida D et al (2017) Potential impact of lateral lymph node dissection (LLND) for low rectal cancer on prognoses and local control: a comparison of 2 high-volume centers in Japan that employ different policies concerning LLND. Surgery 162:303–314
Matsumoto A, Arita K (2017) A technique of laparoscopic lateral pelvic lymph node dissection based on vesicohypogastric fascia and ureterohypogastric nerve fascia for advanced low rectal cancer. Surg Endosc 31:945–948
Park BK, Lee SJ, Hur BY et al (2018) Feasibility of selective lateral node dissection based on magnetic resonance imaging in rectal cancer after preoperative chemoradiotherapy. J Surg Res 232:227–233
Furuhata T, Okita K, Nishidate T et al (2015) Clinical feasibility of laparoscopic lateral pelvic lymph node dissection following total mesorectal excision for advanced rectal cancer. Surg Today 45:310–314
Nakamura T, Watanabe M (2013) Lateral lymph node dissection for lower rectal cancer. World J Surg 37:1808–1813
Manabe T, Koga Y, Kubo H et al (2019) Adverse effects on the postoperative urinary function after combined resection of inferior vesical artery in laparoscopic lateral pelvic lymph node dissection: retrospective analysis of consecutive 95 series. Surg Laparosc Endosc Percutan Tech 29:493–497
Yabuki Y, Sasaki H, Hatakeyama N, Murakami G (2005) Discrepancies between classic anatomy and modern gynecologic surgery on pelvic connective tissue structure: harmonization of those concepts by collaborative cadaver dissection. Am J Obstet Gynecol 193:7–15
Yamaoka Y, Kagawa H, Shiomi A et al (2021) Robotic-assisted surgery may be a useful approach to protect urinary function in the modern era of diverse surgical approaches for rectal cancer. Surg Endosc 35:1317–1323
Song SH, Choi GS, Kim HJ et al (2021) Long-term clinical outcomes of total mesorectal excision and selective lateral pelvic lymph node dissection for advanced low rectal cancer: a comparative study of a robotic versus laparoscopic approach. Tech Coloproctol 25:413–423
Jayne D, Pigazzi A, Marshall H et al (2017) Effect of robotic-assisted vs conventional laparoscopic surgery on risk of conversion to open laparotomy among patients undergoing resection for rectal cancer: the ROLARR randomized clinical trial. JAMA 318:1569–1580
Matsuyama T, Endo H, Yamamoto H et al (2021) Outcomes of robot-assisted versus conventional laparoscopic low anterior resection in patients with rectal cancer: propensity-matched analysis of the National Clinical Database in Japan. BJS Open 5:zrab083. https://doi.org/10.1093/bjsopen/zrab083
Sugishita T, Tsukamoto S, Imaizumi J et al (2022) Evaluation of the learning curve for robot-assisted rectal surgery using the cumulative sum method. Surg Endosc 36:5947–5955
Foo CC, Law WL (2016) The learning curve of robotic-assisted low rectal resection of a novice rectal surgeon. World J Surg 40:456–462
Nishizawa Y, Fujii S, Saito N et al (2012) Differences in tissue degeneration between preoperative chemotherapy and preoperative chemoradiotherapy for colorectal cancer. Int J Colorectal Dis 27:1047–1053
Sekido Y, Nishimura J, Fujino S et al (2020) Predicting lateral pelvic lymph node metastasis based on magnetic resonance imaging before and after neoadjuvant chemotherapy for patients with locally advanced lower rectal cancer. Surg Today 50:292–297
Fokas E, Allgäuer M, Polat B et al (2019) Randomized phase II trial of chemoradiotherapy plus induction or consolidation chemotherapy as total neoadjuvant therapy for locally advanced rectal cancer: CAO/ARO/AIO-12. J Clin Oncol 37:3212–3222
Acknowledgements
We would like to thank Editage (https://www.editage.jp) for English language editing.
Funding
This study has not received specific funding from any funding agency, public, for-profit or non-profit.
Author information
Authors and Affiliations
Contributions
Study conception and design: TI; Data acquisition: TI, JM; Data interpretation: TI, RU, TT, KK; Drafting the manuscript: TI; Supervision of the manuscript: YN.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to declare regarding this study.
Ethical approval
Ethical approval statements has already been mentioned in patients and study design.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ishizaki, T., Mazaki, J., Kasahara, K. et al. Robotic versus laparoscopic approach for minimally invasive lateral pelvic lymph node dissection of advanced lower rectal cancer: a retrospective study comparing short-term outcomes. Tech Coloproctol 27, 579–587 (2023). https://doi.org/10.1007/s10151-023-02818-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10151-023-02818-x