Abstract
Background
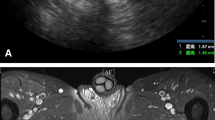
Correct identification of the internal opening is essential in the management of perianal fistulae. The aim of this study was to assess the validity of Goodsall’s Law and the Midline Rule in predicting the path of perianal fistula-in-ano and the location of the internal opening using 3-dimensional endoanal ultrasound.
Methods
An observational study including patients diagnosed with fistula-in-ano, at our institution from January 2006 to December 2020 was performed. Location and distance from the anal verge of the external opening, internal opening, and the path of the fistulous tract were recorded during physical examination and endoanal ultrasound. Goodsall’s and Midline rules were applied to all fistulae according to the location of the external opening. The location of the internal opening as predicted by either rule was then compared to the real location of the internal opening identified during endoanal ultrasound examination.
Results
Nine hundred and nine patients [657 (72.3%) males, mean age 50.78 (49.84–51.72) years] were included. 665 (73.2%) of fistulae were transsphinteric. Concordance between predicted internal opening site and the true internal opening location was 0.601 (good match) for Goodsall’s rule, and 0.416 (moderate match) for the Midline rule. Goodsall’s rule proved to be more predictive in the anterior plane (p < 0.001). Both rules were more likely to make a correct diagnosis in posterior fistulae located 4.5–7.5 mm from the anal verge.
Conclusions
Both Midline and Goodsall’s rules are highly predictive of the course of fistula tracts located in the posterior plane, and are lower for anterior located fistulae, female patients and when the external opening is located further from the anal verge.





Similar content being viewed by others
Availability of data and materials
All data and materials comply with field standards.
Code availability
Not applicable.
References
Garcia-Aguilar J, Belmonte C, Wong WD, Goldberg SM, Madoff RD (1996) Anal fistula surgery. Factors associated with recurrence and incontinence. Dis Colon Rectum 39(7):723–729. https://doi.org/10.1007/BF02054434
Edwards FS (1887) On some of the rarer forms of rectal fistulae. Br Med J 2(1383):13–15. https://doi.org/10.1136/bmj.2.1383.13-a
Goodsall DH, Miles WE (1900) Ano-rectal fistula. In: Goodsall DH, Miles WE (eds) Diseases of the anus and rectum. Longmans, Green & Co, London, pp 92–173
Edwards FS (1908) Disease of the rectum, anus and sigmoid colon, 3rd edn. Churchill, London, p 143
Shouten WR (2008) Abscess, fistula. In: Herold A, Lehur PA, Matzel KE, O’Connell PR (eds) Coloproctology European manual of medicine. Springer, Berlin, p 54
Lunniss PJ, Phillips RKS (2009) Anal fistula: evaluation and management. In: Phillips RKS (ed) Colorectal surgery, 4th edn. Saunders Elsevier, London, p 229
Brunicardi FC (ed) (2015) Schwartz’s principles of surgery, 10th edn. McGraw-Hill, New York, p 1229
Becker A, Koltun L, Sayfan J (2006) Simple clinical examination predicts complexity of perianal fistula. Colorect Dis 8(7):601–604. https://doi.org/10.1111/j.1463-1318.2006.01025.x
Gunawardhana PA, Deen KI (2001) Comparison of hydrogen peroxide instillation with Goodsall’s rule for fistula-in-ano. ANZ J Surg 71(8):472–474. https://doi.org/10.1046/j.1440-1622.2001.02169.x
Coremans G, Dockx S, Wyndaele J, Hendrickx A (2003) Do anal fistulae in Crohn’s disease behave differently and defy Goodsall’s rule more frequently than fistulae that are cryptoglandular in origin? Am J Gastroenterol 98(12):2732–2735. https://doi.org/10.1111/j.1572-0241.2003.08716.x
Zbar AP (2009) David Henry Goodsall: reassessment of the rule. Tech Coloproctol 13(3):185–188. https://doi.org/10.1007/s10151-009-0511-5
Cirocco WC, Reilly JC (1992) Challenging the predictive accuracy of Goodsall’s rule for anal fistulas. Dis Colon Rectum 35(6):537–542. https://doi.org/10.1007/BF02050532
Cirocco WC, Reilly JC (2020) It is time to retire Goodsall’s Rule: the Midline Rule is a more accurate predictor of the true and natural course of anal fistulas. Tech Coloproctol 24(4):317–321. https://doi.org/10.1007/s10151-020-02167-z
Barwood N, Clarke G, Levitt S, Levitt M (1997) Fistula-in-ano: a prospective study of 107 patients. Aust N Z J Surg 67(2–3):98–102. https://doi.org/10.1111/j.1445-2197.1997.tb01911.x
Kuijpers HC, Schulpen T (1985) Fistulography for fistula-in-ano. Is it useful? Dis Colon Rectum 28(2):103–104. https://doi.org/10.1007/BF02552656
Tepes B, Cerni I (2008) The use of different diagnostic modalities in diagnosing fistula-in-ano. Hepatogastroenterology 55(84):912–915
Pomerri F, Dodi G, Pintacuda G, Amadio L, Muzzio PC (2010) Anal endosonography and fistulography for fistula-in-ano. Radiol Med 115(5):771–783. https://doi.org/10.1007/s11547-010-0524-1
Lunniss PJ, Barker PG, Sultan AH et al (1994) Magnetic resonance imaging of fistula-in-ano. Dis Colon Rectum 37(7):708–718. https://doi.org/10.1007/BF02054416
deSouza NM, Gilderdale DJ, Coutts GA, Puni R, Steiner RE (1998) MRI of fistula-in-ano: a comparison of endoanal coil with external phased array coil techniques. J Comput Assist Tomogr 22(3):357–363. https://doi.org/10.1097/00004728-199805000-00004
Buchanan GN, Halligan S, Bartram CI, Williams AB, Tarroni D, Cohen CR (2004) Clinical examination, endosonography, and MR imaging in preoperative assessment of fistula in ano: comparison with outcome-based reference standard. Radiology 233(3):674–681. https://doi.org/10.1148/radiol.2333031724
Gustafsson UM, Kahvecioglu B, Aström G, Ahlström H, Graf W (2001) Endoanal ultrasound or magnetic resonance imaging for preoperative assessment of anal fistula: a comparative study. Colorect Dis 3(3):189–197. https://doi.org/10.1046/j.1463-1318.2001.00241.x
Garg P, Singh P, Kaur B (2017) Magnetic resonance imaging (MRI): operative findings correlation in 229 fistula-in-ano patients. World J Surg 41(6):1618–1624. https://doi.org/10.1007/s00268-017-3886-x
Navarro-Luna A, García-Domingo MI, Rius-Macías J, Marco-Molina C (2004) Ultrasound study of anal fistulas with hydrogen peroxide enhancement. Dis Colon Rectum 47(1):108–114. https://doi.org/10.1007/s10350-003-0015-8
West RL, Dwarkasing S, Felt-Bersma RJ et al (2004) Hydrogen peroxide-enhanced three-dimensional endoanal ultrasonography and endoanal magnetic resonance imaging in evaluating perianal fistulas: agreement and patient preference. Eur J Gastroenterol Hepatol 16(12):1319–1324. https://doi.org/10.1097/00042737-200412000-00014
Buchanan GN, Bartram CI, Williams AB, Halligan S, Cohen CR (2005) Value of hydrogen peroxide enhancement of three-dimensional endoanal ultrasound in fistula-in-ano. Dis Colon Rectum 48(1):141–147. https://doi.org/10.1007/s10350-004-0752-3
Garcés Albir M, García Botello S, Esclápez Valero P et al (2010) Evaluación de las fístulas perianales mediante ecografía endoanal tridimensional y correlación con los hallazgos intraoperatorios [Evaluation of three-dimensional endoanalendosonography of perianal fistulas and correlationwithsurgicalfindings] [publishedcorrectionappears in Cir Esp. 2010 Sep;88(3):206]. Cir Esp 87(5):299–305. https://doi.org/10.1016/j.ciresp.2010.02.006
Garcés-Albir M, García-Botello SA, Espi A et al (2016) Three-dimensional endoanal ultrasound for diagnosis of perianal fistulas: reliable and objective technique. World J Gastrointest Surg 8(7):513–520. https://doi.org/10.4240/wjgs.v8.i7.513
Murad-Regadas SM, RegadasFilho FSP, Holanda EC, Veras LB, Vilarinho ADS, Lopes MS (2018) Can three-dimensional anorectal ultrasonography be included as a diagnostic tool for the assessment of anal fistula before and after surgical treatment? Arq Gastroenterol 55(Suppl 1):18–24. https://doi.org/10.1590/S0004-2803.201800000-42
Mantoo S, Mandovra P, Goh S (2020) Using preoperative three-dimensional endoanal ultrasound to determine operative procedure in patients with perianal fistulas [published online ahead of print, 2020 Jan 28]. Colorect Dis. https://doi.org/10.1111/codi.14993
Parks AG, Gordon PH, Hardcastle JD (1976) A classification of fistula-in-ano. Br J Surg 63(1):1–12. https://doi.org/10.1002/bjs.1800630102
Leenders LAM, Stijns J, van Loon YT, Van Tilborg F, Wasowicz DK, Zimmerman DDE (2021) The complexity of cryptoglandular fistula-in-ano can be predicted by the distance of the external opening to the anal verge; implications for preoperative imaging? Tech Coloproctol 25(1):109–115. https://doi.org/10.1007/s10151-020-02353-z (Epub 2020 Nov 12)
Garcés-Albir M, García-Botello SA, Esclapez-Valero P et al (2012) Quantifying the extent of fistulotomy. How much sphincter can we safely divide? A three-dimensional endosonographic study. Int J Colorect Dis 27(8):1109–1116. https://doi.org/10.1007/s00384-012-1437-3
GarcésAlbir M, García-Botello SA, Pla-Martí V, Martín-Arévalo J, Moro-Valdezate D, Espi A, Ortega J (2020) Rectal advancement flaps for the treatment of transphincteric perianal fistulas: a three-dimensional endoanal ultrasound and quality of life assessment. Rev EspEnferm Dig 112(11):860–863. https://doi.org/10.17235/reed.2020.7187/2020
Funding
The authors did not receive any funding for this research.
Author information
Authors and Affiliations
Contributions
SGB: conceptualization; investigation; methodology; writing-original draft. JMA: investigation; methodology; data collection; writing-original draft. RMF: investigation; methodology; data collection. DMV: supervisión; data collection. VPM: conceptualization; investigation. AEM: investigation; methodology; supervision.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they do not have any conflicts of interest.
Ethics approval
Institutional board and ethics approval were obtained for this work.
Consent to participate
This is an observational study. The INCLIVA Research Ethics Committee has confirmed that no ethical approval is required. Informed consent was obtained from all individual participants included in the study.
Consent for publication
Patients signed informed consent regarding publishing their data and photographs.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Garcia-Botello, S., Martín-Arévalo, J., Martí-Fernández, R. et al. Three-dimensional endoanal ultrasound to assess the validity of Goodsall’s Rule and the Midline Rule in predicting the path of perianal fistula-in-ano and the location of the internal opening. Tech Coloproctol 26, 351–361 (2022). https://doi.org/10.1007/s10151-022-02592-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10151-022-02592-2