Abstract
Background
The aim of this study was to evaluate a C-reactive protein (CRP)-driven monitoring discharge strategy for patients with Crohn’s disease (CD) undergoing laparoscopic ileo-cecal resection (ICR) and if needed, temporary stoma closure (SC).
Methods
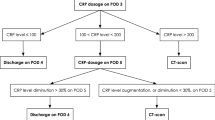
Four hundred and ten patients who underwent laparoscopic ICR for CD: 153 patients (CRP group) between June 2016 and June 2020 at our department, had a CRP-driven monitoring discharge on postoperative day (POD) 3 and were discharged on POD 4 if CRP < 100 mg/L. These patients were matched (according to age, sex, body mass index, type of CD (and stoma or not) to 257 patients who underwent laparoscopic ICR for CD between January 2009 and May 2016, without CRP monitoring (Control group). For SC, 79 patients with CRP monitoring were matched with 88 control patients. Primary outcome was overall length of hospital stay (LHS). Secondary outcomes were discharge on POD 4 for SC and POD 4 and POD 6 for ICR, 3-month postoperative overall morbidity and severe morbidity rates, surgical site infection, readmission rates, and CRP level in cases of morbidity at 3 months.
Results
For ICR without stoma, mean LHS was significantly shorter in the CRP group than in the control group (6.9 ± 2 days vs 8.3 ± 6 days, p = 0.017). Discharge occurred on POD 6 (or before) in 73% of the patients (CRP group) vs 60% (Control group) (p = 0.027). For ICR with stoma, LHS was 8 days for both groups (p = 0.612). For SC, LHS was significantly shorter in the CRP group than in the control group (5.5 ± 3 days vs 7.1 ± 4 days; p = 0.002). Discharge occurred on POD 4 in 62% (CRP group) vs 30% (Control) (p = 0.003). Postoperative 3-month overall and severe morbidity, and rehospitalization rates were similar between groups.
Conclusions
CRP-driven monitoring discharge strategy after laparoscopic ICR for CD is associated with a significant reduction of LHS, without increasing morbidity, reoperation or rehospitalisation rates.

Similar content being viewed by others
References
Fumery M (2018). Épidémiologie et histoire naturelle des maladies inflammatoires chroniques intestinales : 30 ans de registre EPIMAD. EPIMAD, Volume 25, numero 2, Février 2018
Bouguen G, Peyrin-Biroulet L (2011) Surgery for adult Crohn’s disease: what is the actual risk? Gut 9:1178–1181
Yamamoto T, Allan RN, Keighley MRB (2000) Risk factors for intra-abdominal sepsis after surgery in Crohn’s disease. Dis Colon Rectum 43:1141–1145
Alves A, Panis Y, Bouhnik Y, Pocard M, Vicaut E, Valleur P (2007) Risk factors for intra-abdominal septic complications after a first ileocecal resection for Crohn’s disease: a multivariate analysis in 161 consecutive patients. Dis Colon Rectum 50:331–336
Galata C, Kienle P, Weiss C, Seyfried S, Reißfelder C, Hardt J (2019) Risk factors for early postoperative complications in patients with Crohn’s disease after colorectal surgery other than ileocecal resection or right hemicolectomy. Int J Colorectal Dis 34:293–300
Su’a BU, Mikaere HL, Rahiri JL, Bissett IB, Hill AG (2017) Systematic review of the role of biomarkers in diagnosing anastomotic leakage following colorectal surgery. Br J Surg 104:503–12
Straatman J, Harmsen AMK, Cuesta MA, Berkhof J, Jansma EP, van der Peet DL (2015) Predictive value of C-reactive protein for major complications after major abdominal surgery: a systematic review and pooled-analysis. Lau WYJ, éditeur. PLOS One 10:e0132995
Kørner H, Nielsen HJ, Søreide JA, Nedrebø BS, Søreide K, Knapp JC (2009) Diagnostic accuracy of C-reactive protein for intraabdominal infections after colorectal resections. J Gastrointest Surg 13:1599–1606
Warschkow R, Tarantino I, Torzewski M, Näf F, Lange J, Steffen T (2011) Diagnostic accuracy of C-reactive protein and white blood cell counts in the early detection of inflammatory complications after open resection of colorectal cancer: a retrospective study of 1187 patients. Int J Colorectal Dis 26:1405–1413
Singh PP, Zeng ISL, Srinivasa S, Lemanu DP, Connolly AB, Hill AG (2014) Systematic review and meta-analysis of use of serum C-reactive protein levels to predict anastomotic leak after colorectal surgery: use of C-reactive protein levels to predict anastomotic leak after colorectal surgery. Br J Surg 101:339–346
Scepanovic MS, Kovacevic B, Cijan V, Antic A, Petrovic Z, Asceric R et al (2013) C-reactive protein as an early predictor for anastomotic leakage in elective abdominal surgery. Tech Coloproctol 17:541–547
Garcia-Granero A, Frasson M, Flor-Lorente B, Blanco F, Puga R, Carratalá A et al (2013) Procalcitonin and C-reactive protein as early predictors of anastomotic leak in colorectal surgery: a prospective observational study. Dis Colon Rectum 56:475–483
Domínguez-Comesaña E, Estevez-Fernández SM, López-Gómez V, Ballinas-Miranda J, Domínguez-Fernández R (2017) Procalcitonin and C-reactive protein as early markers of postoperative intra-abdominal infection in patients operated on colorectal cancer. Int J Colorectal Dis 32:1771–1774
Cousin F, Ortega-Deballon P, Bourredjem A, Doussot A, Giaccaglia V, Fournel I (2016) Diagnostic accuracy of procalcitonin and C-reactive protein for the early diagnosis of intra-abdominal infection after elective colorectal surgery: a meta-analysis. Ann Surg 264:252–256
Adamina M, Steffen T, Tarantino I, Beutner U, Schmied BM, Warschkow R (2015) Meta-analysis of the predictive value of C-reactive protein for infectious complications in abdominal surgery. Br J Surg 102:590–598
Facy O, Paquette B, Orry D, Binquet C, Masson D, Bouvier A et al (2016) Diagnostic accuracy of inflammatory markers as early predictors of infection after elective colorectal surgery: results from the IMACORS study. Ann Surg 263:961–966
Hain E, Maggiori L, Laforest A, FrontaliProst à la DenisePanis AJY (2019) Hospital stay for temporary stoma closure is shortened by C-reactive protein monitoring: a prospective case-matched study. Tech Coloproctology 23:453–459
Cazelles A, Giacca M, Monsinjon M, Hain E, Frontali A, Panis Y (2021) Monitoring of C-reactive protein decreases length of stay after laparoscopic total mesorectal excision for cancer: a prospective case-matched study in 236 patients. Colorectal dis 23:1158–1166
Benoit O, Faron M, Margot N, Creavin B, Debove C, Tiret E, Parc Y, Lefevre JH (2019) C-reactive protein values after colorectal resection: can we discharge a patient with a C-reactive protein value >100? A retrospective cohort study. Dis Colon Rectum 62:88–96
Carvello M, Di Candido F, Greco M, Foppa C, Maroli A, Fiorino G, Cecconi M, Danese S, Spinelli A (2020) The trend of C-reactive protein allows a safe early discharge after surgery for Crohn’s disease. Updat Surg 72:985–989
Van de Overstraeten AB, Van Hoef S, Vermeire S, Ferrante M, Fieuws S, Wolthuis A, Van Assche G, D’Hoore A (2015) Postoperative inflammatory response in Crohn’s patients: a comparative study. J Crohn’s Colitis 9:1127–1131
Goyer P, Alves A, Bretagnol F, Bouhnik Y, Valleur P, Panis Y (2009) Impact of complex Crohn’s disease on the outcome of laparoscopic ileocecal resection: a comparative clinical study in 124 patients. Dis Colon Rectum 52:205–210
Adamina M, Bonovas S, Raine T, Spinelli A, Warusavitarne J, Armuzzi A, Bachmann O, Bager P, Biancone L, Bokemeyer B, Bossuyt P, Burisch J, Collins P, Doherty G, El-Hussuna A, Ellul P, Fiorino G, Frei-Lanter C, Furfaro F, Gingert C, Gionchetti P, Gisbert JP, Gomollon F, González Lorenzo M, Gordon H, Hlavaty T, Juillerat P, Katsanos K, Kopylov U, Krustins E, Kucharzik T, Lytras T, Maaser C, Magro F, Marshall JK, Myrelid P, Pellino G, Rosa I, Sabino J, Savarino E, Stassen L, Torres J, Uzzan M, Vavricka S, Verstockt B, Zmora O (2020) ECCO guidelines on therapeutics in Crohn’s disease: surgical treatment. J Crohns Colitis 14:155–168
Shigeta K, Okabayashi K, Hasegawa H, Tsuruta M, Seishima R, Kitagawa Y (2016) Meta-analysis of laparoscopic surgery for recurrent Crohn’s disease. Surg Today 46:970–978
Dasari BV, McKay D, Gardiner K (2011) Laparoscopic versus open surgery for small bowel Crohn’s disease. Cochrane colorectal cancer group, éditeur. Cochrane Database Syst Rev 19:CD006956
Correia MITD, Waitzberg DL (2003) The impact of malnutrition on morbidity, mortality, length of hospital stay and costs evaluated through a multivariate model analysis. Clin Nutr Edinb Scotl 22:235–239
Norman K, Pichard C, Lochs H, Pirlich M (2008) Prognostic impact of disease-related malnutrition. Clin Nutr 27:5–15
Hu W-H, Cajas-Monson LC, Eisenstein S, Parry L, Cosman B, Ramamoorthy S (2015) Preoperative malnutrition assessments as predictors of postoperative mortality and morbidity in colorectal cancer: an analysis of ACS-NSQIP. Nutr J 14:91
Forsmo HM, Pfeffer F, Rasdal A, Sintonen H, Körner H, Erichsen C (2016) Pre- and postoperative stoma education and guidance within an enhanced recovery after surgery (ERAS) programme reduces length of hospital stay in colorectal surgery. Int J Surg 36:121–126
Rashidi L, Long K, Hawkins M, Menon R, Bellevue O (2016) Stoma creation: does onset of ostomy care education delay hospital length of stay? Am J Surg 211:954–957
European Society of Coloproctology (ESCP) collaborating group (2019) Patients with Crohn’s disease have longer post-operative in-hospital stay than patients with colon cancer but no difference in complications’ rate. World J Gastrointest Surg 11:261–270
Funding
The authors declare that they have no financial disclosure.
Author information
Authors and Affiliations
Contributions
CG: writing – original draft; data acquisition, analysis and interpretation. CDP: review and editing. AF, MM, MG: review; YP: conception and design of the study, writing – review and editing; supervision; project administration, final approval of the version to be submitted.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest. No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
Ethical approval
The study was approved by the Ethics Committee of the “Hôpital Beaujon – Assistance Publique des Hôpitaux de Paris (APHP)”.
Informed consent
Informed consent was obtained for the surgical procedure prior to their participation.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Guyard, C., de Ponthaud, C., Frontali, A. et al. C-reactive protein monitoring after ileocecal resection and stoma closure reduces length of hospital stay: a prospective case-matched study in 410 patients with Crohn’s disease. Tech Coloproctol 26, 443–451 (2022). https://doi.org/10.1007/s10151-022-02590-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10151-022-02590-4