Abstract
Background
The proposed difficulty scoring system (DSS) may aid in preoperative planning for laparoscopic total mesorectal excision (L-TME) for rectal cancer.
Methods
Fifty-three patients [28 males; 59.0 (31.0–88.0) years of age] treated for rectal cancer at our institution from 2/2011–5/2018 were identified. “Difficult operation” (DO) was defined as the presence of ≥3 factors: operative time ≥320 min, estimated blood loss >250 ml, intraoperative complications, conversion to laparotomy, >2 stapler applications, incomplete TME quality, and/or subjective perceived difficulty. Univariate analysis and multivariate logistic regression model with backward elimination method were used to obtain a DSS which consists of two factors: sex (male = 1 and female = 0) and body mass index (BMI) (≥30 kg/m2 = 1, <30 kg/m2 = 0).
Results
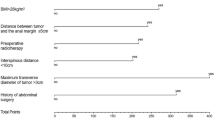
In univariate analysis, sex (p = 0.0217), BMI (p = 0.0026), American Society of Anesthesiologists (ASA) score (p = 0.0372), and magnetic resonance imaging transverse diameter (p = 0.0441) correlated to DO. Multivariate analysis revealed that sex and BMI were the most important risk factors for a DO [area under the receiver operating characteristic curve [AUC] = 0.7761, 95% CI = (0.6443–0.9080)]. Male patients with a BMI ≥ 30 kg/m2 were more likely to experience a DO (77.8%). The simplified DSS did not weaken the discriminating power compared to multivariate logistic regression model (AUC 0.7696 vs. 0.7761, p = 0.7387). L-TME with a DSS of 0, 1, and 2 had a DO rate of 10%, 33.3%, and 77.8%, respectively.
Conclusions
A simplified DSS may be used preoperatively in preparation for L-TME.


Similar content being viewed by others
References
Heald RJ (1979) A new approach to rectal cancer. Br J Hosp Med 22:277–281
Heald RJ, Ryall RD (1986) Recurrence and survival after total mesorectal excision for rectal cancer. Lancet 1:1479–1482
Heald RJ (1988) The 'Holy Plane' of rectal surgery. J R Soc Med 81:503–508
Green BL, Marshall HC, Collinson F et al (2013) Long-term follow-up of the Medical Research Council CLASICC trial of conventional versus laparoscopically assisted resection in colorectal cancer. Br J Surg 100:75–82
Jeong SY, Park JW, Nam BH et al (2014) Open versus laparoscopic surgery for mid-rectal or low-rectal cancer after neoadjuvant chemoradiotherapy (COREAN trial): survival outcomes of an open-label, non-inferiority, randomised controlled trial. Lancet Oncol 15:767–774
Fleshman J, Branda M, Sargent DJ et al (2015) Effect of laparoscopic-assisted resection vs open resection of stage II or III rectal cancer on pathologic outcomes: the ACOSOG Z6051 randomized clinical trial. JAMA 314:1346–1355
Jayne D, Pigazzi A, Marshall H et al (2017) Effect of robotic-assisted vs conventional laparoscopic surgery on risk of conversion to open laparotomy among patients undergoing resection for rectal cancer: the ROLARR randomized clinical trial. JAMA 318:1569–1580
Hermanek P, Junginger T (2005) The circumferential resection margin in rectal carcinoma surgery. Tech Coloproctol 9:193–199 (discussion 199–200)
Quirke P, Steele R, Monson J et al (2009) Effect of the plane of surgery achieved on local recurrence in patients with operable rectal cancer: a prospective study using data from the MRC CR07 and NCIC-CTG CO16 randomised clinical trial. Lancet 373:821–828
Kitz J, Fokas E, Beissbarth T et al (2018) Association of plane of total mesorectal excision with prognosis of rectal cancer: secondary analysis of the CAO/ARO/AIO-04 phase 3 randomized clinical trial. JAMA Surg 153:e18160
Benson AB, Venook AP, Al-Hawary MM et al (2018) Rectal cancer, Version 2.2018, NCCN clinical practice guidelines in oncology. J Natl Compr Canc Netw 16:874–901
Commission on Cancer (1996–2019). American College of Surgeons National Accreditation Program for Rectal Cancer (www.facs.org/quality-programs/cancer/naprc).
D’Souza N, de Neree Tot Babberich MPM, D’Hoore A et al (2019) Definition of the Rectum: an international, expert-based Delphi Consensus. Ann Surg 270(6):955–959
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 24:205–213
Escal L, Nougaret S, Guiu B et al (2018) MRI-based score to predict surgical difficulty in patients with rectal cancer. Br J Surg 105:140–146
Li VK, Wexner SD, Pulido N et al (2009) Use of routine intraoperative endoscopy in elective laparoscopic colorectal surgery: can it further avoid anastomotic failure? Surg Endosc 23:2459–2465
Targarona EM, Balague C, Pernas JC et al (2008) Can we predict immediate outcome after laparoscopic rectal surgery? Multivariate analysis of clinical, anatomic, and pathologic features after 3-dimensional reconstruction of the pelvic anatomy. Ann Surg 247:642–649
Akiyoshi T, Kuroyanagi H, Oya M et al (2009) Factors affecting the difficulty of laparoscopic total mesorectal excision with double stapling technique anastomosis for low rectal cancer. Surgery 146:483–489
Veenhof AA, Engel AF, van der Peet DL et al (2008) Technical difficulty grade score for the laparoscopic approach of rectal cancer: a single institution pilot study. Int J Colorectal Dis 23:469–475
Ferko A, Malý O, Örhalmi J, Dolejš J (2016) CT/MRI pelvimetry as a useful tool when selecting patients with rectal cancer for transanal total mesorectal excision. Surg Endosc 30:1164–1171
Funding
The authors have no relevant financial disclosures.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All the authors declare that have no conflict of interest.
Ethical approval
The study protocol was approved by the ethics review board at our institution.
Informed consent
All patients gave informed consent at the time of their surgery.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Krizzuk, D., Yellinek, S., Parlade, A. et al. A simple difficulty scoring system for laparoscopic total mesorectal excision. Tech Coloproctol 24, 1137–1143 (2020). https://doi.org/10.1007/s10151-020-02285-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10151-020-02285-8