Abstract
Background
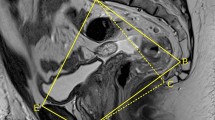
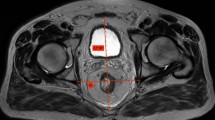
The difficulty of performing total mesorectal excision (TME) for rectal cancer partly relies on the surgeon’s subjective assessment of the individual patient’s pelvic anatomy and tumour characteristics, which generally influences the choice of platform used (open, laparoscopic, robotic or trans-anal surgery). Recent studies have found associations between several anatomical pelvic measurements and surgical difficulty. The aim of this study was to systematically review existing data reporting the use of magnetic resonance imaging (MRI)-based pelvic measurements to predict technical difficulty and outcomes of TME, and determine whether pelvimetry could optimise patient-specific selection of a particular surgical approach.
Methods
MEDLINE, Embase and Cochrane Library databases were systematically searched for studies reporting MRI-based pelvic measurements in patients undergoing surgery for rectal cancer, and the effect of these measurements on surgical difficulty.
Results
Eleven studies reporting the association between MRI-pelvimetry measurements and rectal cancer surgical outcomes were included. Indicators for surgical difficulty used in the included studies were involved circumferential resection margin, longer operative time, incomplete TME, higher blood loss, anastomotic leak, conversion to open surgery and overall complications. Bony pelvic measurements which were associated with increased surgical difficulty in more than one study were a smaller interspinous distance, a smaller intertubercle distance, a smaller pelvic inlet and larger pubic tubercle height. Two studies identified larger mesorectal fat area as a predictor of surgical difficulty.
Conclusions
Bony pelvic measurements may predict surgical difficulty during TME, however, use of different indicators of difficulty limit comparison between studies. Early data suggest MRI soft tissue measurements may predict surgical difficulty and warrants further investigation.





Similar content being viewed by others
References
Wibe A, Rendedal PR, Svensson E, Norstein J, Eide TJ, Myrvold HE et al (2002) Prognostic significance of the circumferential resection margin following total mesorectal excision for rectal cancer. Br J Surg 89(3):327–334
Kitz J, Fokas E, Beissbarth T, Strobel P, Wittekind C, Hartmann A et al (2018) Association of plane of total mesorectal excision with prognosis of rectal cancer: secondary analysis of the CAO/ARO/AIO-04 phase 3 randomized clinical trial. JAMA Surg 153(8):e181607
Taylor FG, Quirke P, Heald RJ, Moran BJ, Blomqvist L, Swift IR et al (2014) Preoperative magnetic resonance imaging assessment of circumferential resection margin predicts disease-free survival and local recurrence: 5-year follow-up results of the MERCURY study. J Clin Oncol 32(1):34–43
Lenhard M, Johnson T, Weckbach S, Nikolaou K, Friese K, Hasbargen U (2009) Three-dimensional pelvimetry by computed tomography. Radiol Med 114(5):827–834
Boyle KM, Petty D, Chalmers AG, Quirke P, Cairns A, Finan PJ et al (2005) MRI assessment of the bony pelvis may help predict resectability of rectal cancer. Colorectal Dis 7(3):232–240
Salerno G, Daniels IR, Brown G, Norman AR, Moran BJ, Heald RJ (2007) Variations in pelvic dimensions do not predict the risk of circumferential resection margin (CRM) involvement in rectal cancer. World J Surg 31(6):1313–1320
Baik SH, Kim NK, Lee KY, Sohn SK, Cho CH, Kim MJ et al (2008) Factors influencing pathologic results after total mesorectal excision for rectal cancer: analysis of consecutive 100 cases. Ann Surg Oncol 15(3):721–728
Boyle KM, Chalmers AG, Finan PJ, Sagar PM, Burke D (2009) Morphology of the mesorectum in patients with primary rectal cancer. Dis Colon Rectum 52(6):1122–1129
Killeen T, Banerjee S, Vijay V, Al-Dabbagh Z, Francis D, Warren S (2010) Magnetic resonance (MR) pelvimetry as a predictor of difficulty in laparoscopic operations for rectal cancer. Surg Endosc 24(12):2974–2979
Kim JY, Kim YW, Kim NK, Hur H, Lee K, Min BS et al (2011) Pelvic anatomy as a factor in laparoscopic rectal surgery: a prospective study. Surg Laparosc Endosc Percutan Tech 21(5):334–339
Baek SJ, Kim CH, Cho MS, Bae SU, Hur H, Min BS et al (2015) Robotic surgery for rectal cancer can overcome difficulties associated with pelvic anatomy. Surg Endosc 29(6):1419–1424
Atasoy G, Arslan NC, Elibol FD, Sagol O, Obuz F, Sokmen S (2018) Magnetic resonance-based pelvimetry and tumor volumetry can predict surgical difficulty and oncologic outcome in locally advanced mid-low rectal cancer. Surg Today 48(12):1040–1051
Escal L, Nougaret S, Guiu B, Bertrand MM, de Forges H, Tetreau R et al (2018) MRI-based score to predict surgical difficulty in patients with rectal cancer. Br J Surg 105(1):140–146
de’Angelis N, Pigneur F, Martinez-Perez A, Vitali GC, Landi F, Torres-Sanchez T, et al. (2018) Predictors of surgical outcomes and survival in rectal cancer patients undergoing laparoscopic total mesorectal excision after neoadjuvant chemoradiation therapy: the interest of pelvimetry and restaging magnetic resonance imaging studies. Oncotarget. 9(38):25315-31
Yamaoka Y, Yamaguchi T, Kinugasa Y, Shiomi A, Kagawa H, Yamakawa Y et al (2019) Mesorectal fat area as a useful predictor of the difficulty of robotic-assisted laparoscopic total mesorectal excision for rectal cancer. Surg Endosc 33(2):557–566
de’Angelis N, Pigneur F, Martinez-Perez A, Vitali GC, Landi F, Gomez-Abril SA, et al. (2019) Assessing surgical difficulty in locally advanced mid-low rectal cancer: the accuracy of two MRI-based predictive scores. Colorectal Dis. 21(3):277–86.
Funding
Jonathan Hong is the recipient of the Mitchell J Notaras Fellowship in Colorectal Surgery.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
Not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix S1–Medline (OVID: 1946-present)
Appendix S1–Medline (OVID: 1946-present)
-
1.
(MRI or MR* or magnetic resonance).tw
-
2.
Magnetic Resonance Imaging/
-
3.
((pelvis or pelvic) adj3 (measure* or anatom* or distan* or imag* or volume* or area*)).tw
-
4.
Pelvimetry/
-
5.
Rectal Neoplasma/
-
6.
(rect* adj3 (cancer* or malign* or excis* or resect* or neoplas* or surg*)).tw
-
7.
(mesorect* adj3 (excision* or resect* or surg* or dissect*)).tw
-
8.
5 OR 6 OR 7
-
9.
3 OR 4
-
1.
1 OR 2
-
11.
8 AND 9 AND 10
Rights and permissions
About this article
Cite this article
Hong, J.SY., Brown, K.G.M., Waller, J. et al. The role of MRI pelvimetry in predicting technical difficulty and outcomes of open and minimally invasive total mesorectal excision: a systematic review. Tech Coloproctol 24, 991–1000 (2020). https://doi.org/10.1007/s10151-020-02274-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10151-020-02274-x