Abstract
Background
Complex anal fistula in Crohn’s disease (CD) poses a challenging problem. We sought to evaluate long-term surgical healing of complex anal fistula in CD through the two robust repair options—ligation of the intersphincteric fistula tract (LIFT) and advancement flap (AF).
Methods
A single-center retrospective study was conducted evaluating long-term healing rates in patients with CD with complex anal fistula undergoing LIFT or AF in 2008–2018. Fistula healing was defined as closure of external wounds, cessation of drainage and absence of pain. Short-term and long-term healing rates were compared. Cox proportional hazards model was performed to identify independent predictors of fistula healing.
Results
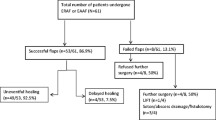
The study cohort included 60 CD patients undergoing LIFT (n = 38) or AF (n = 22). The AF group included 8 dermal flaps. Patients having LIFT were younger (35 years vs 43 years; p = 0.007), more likely to have a seton at the time of repair (92% vs 68%; p = 0.03) and less likely to have had prior repair attempts (34% vs 68%; p = 0.02). Short-term fistula healing occurred in 65% (n = 39) of the overall study cohort. However, at final follow-up, median 36 months (range 6–192 months), only 46% (n = 28) of repaired fistulas were healed. Considering the overall status of the cohort’s perianal health at final follow-up, including both repaired, secondary or novel anal fistulas, only 50% (n = 30) of all patients in the cohort had all fistula sites healed and maintained bowel continuity at final follow-up. On Cox proportional hazards analysis, LIFT independently predicted long-term fistula healing (hazard ratio 2.3; 95% confidence interval 1.1–4.9; p = 0.03). Only a small number of patients (n = 5; 8%) required fecal diversion (n = 3) and/or proctectomy (n = 2).
Conclusions
Repair of complex anal fistula in CD results in modest healing rates. LIFT independently predicts long-term healing. However, these results must be taken in context, considering differences in patient and fistula characteristics between groups. These results ought to be kept in mind when counseling CD patients with complex anal fistula.


Similar content being viewed by others
References
Bubbers EJ, Cologne KG (2016) Management of complex anal fistulas. Clin Colon Rectal Surg 29:43–49
Tan KK, Tan IJ, Lim FS et al (2011) The anatomy of failures following the ligation of intersphincteric tract technique for anal fistula: a review of 93 patients over 4 years. Dis Colon Rectum 54:1368–1372
Steele SR, Kumar R, Feingold DL et al (2011) Standards Practice Task Force of the American Society of Colorectal Surgery. Practice parameters for the management of perianal abscess and fistula-in-ano. Dis Colon Rectum 54:1465–1474
Joo JS, Weiss EG, Nogueras JJ et al (1998) Endorectal advancement AF in perianal Crohn's disease. Am Surg 64:147–150
Soltani A, Kaiser AM (2010) Endorectal advancement AF for cryptoglandular or Crohn's fistula-in-ano. Dis Colon Rectum 53:486–495
Schouten WR, Zimmerman DD, Briel JW (1999) Transanal advancement AF repair of transsphincteric fistulas. Dis Colon Rectum 42:1419–1422 (discussion 22-3)
Ortiz H, Marzo J (2000) Endorectal advancement repair and fistulectomy for high trans-sphincteric and suprasphincteric fistulas. Br J Surg 87:1680–1683
Mizrahi N, Wexner SD, Zmora O et al (2002) Endorectal advancement flap: are there predictors of failure? Dis Colon Rectum 45:1616–1621
Rozalen V, Pares D, Sanchez E et al (2017) Advancement flap technique for anal fistula in patients with Crohn's disease: a systematic review of the literature. Cir Esp 95:558–565
Roper MT, Trinidad SM, Ramamoorthy SL et al (2019) Endorectal advancement flaps for perianal fistulae in Crohn’s disease: careful patient selection leads to optimal outcomes. J Gastrointest Surg 2019;23:2277–2284
Rojanasakul A, Pattanaarun J, Sahakitrungruang C et al (2007) Total anal sphincter saving technique for fistula-in-ano; the ligation of intersphincteric fistula tract. J Med Assoc Thai 90:581–586
Gingold DS, Murrell ZA, Fleshner PR (2014) A prospective evaluation of the ligation of the intersphincteric tract procedure for complex anal fistula in patients with Crohn's disease. Ann Surg 260:1057–1061
Kaminski JP, Zaghiyan K, Fleshner P (2017) Increasing experience of ligation of the intersphincteric fistula tract for patients with Crohn's disease: what have we learned? Colorectal Dis 19:750–755
World Medical Association (2012) Declaration of Helsinki-ethical principles for medical research involving human subjects. https://www.wma.net/en/30publications/10policies/b3/. Accessed 30 Sept 2012
Marchesa P, Hull TL, Fazio VW (1998) Advancement sleeve flaps for treatment of severe perianal Crohn's disease. Br J Surg 85(12):1695–1698
Makowiec F, Jehle EC, Becker HD et al (1995) Clinical course after transanal advancement flap repair of perianal fistula in patients with Crohn's disease. Br J Surg 82:603–606
Mushaya C, Bartlett L, Schulze B et al (2012) Ligation of intersphincteric fistula tract compared with advancement flap for complex anorectal fistulas requiring initial seton drainage. Am J Surg 204:283–289
Madbouly KM, El Shazly W, Abbas KS et al (2014) Ligation of intersphincteric fistula tract versus mucosal advancement flap in patients with high transsphincteric fistula-in-ano: a prospective randomized trial. Dis Colon Rectum 57:1202–1208
Van Praag E, Stellingwerf M, Van Der Bilt J et al (2019) Ligation of the intersphincteric fistula tract vs. endorectal advancement flap for high perianal fistulas in Crohn's disease: a retrospective cohort study. J Crohns Colitis. https://doi.org/10.1093/ecco-jcc/jjz181
Stellingwerf ME, van Praag EM, Tozer PJ et al (2019) Systematic review and meta-analysis of endorectal advancement flap and ligation of the intersphincteric fistula tract for cryptoglandular and Crohn’s high perianal fistulas. BJS open 3:231–241
Uribe N, Millan M, Minguez M et al (2007) Clinical and manometric results of endorectal advancement flaps for complex anal fistula. Int J Colorectal Dis 22:259–264
Chen HJ, Sun GD, Zhu P et al (2017) Effective and long-term outcome following ligation of the intersphincteric fistula tract (LIFT) for transsphincteric fistula. Int J Colorectal Dis 32:583–585
Sun XL, Wen K, Chen YH et al (2019) Long-term outcomes and quality of life following ligation of the intersphincteric fistula tract for high transsphincteric fistulas. Colorectal Dis 21:30–37
Sileri P, Giarratano G, Franceschilli L et al (2014) Ligation of the intersphincteric fistula tract (LIFT): a minimally invasive procedure for complex anal fistula: 2-year results of a prospective multicentric study. Surg Innov 21:476–480
Vogel JD, Johnson EK, Morris AM et al (2016) Clinical practice guidelines for the management of anorectal abscess, fistula-in-ano, and rectovaginal fistula. Dis Colon Rectum 59:1117–1133
Funding
None declared. The authors have no relevant disclosures and source of financial support was none. The authors have no disclosures of funding for this work from any of the following organizations: National Institute of Health (NIH); Wellcome Trust; Howard Hughes Medical Institute (HHMI); and others.
Author information
Authors and Affiliations
Contributions
Per the International Committee of Medical Journal Editors (ICMJE) guidelines. Angela Mujukian: Substantial contributions to acquisition, analysis, or interpretation of data, original drafting; revision for critically important intellectual content, final approval of the version to be published, accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. Adam Truong: substantial contributions to acquisition, analysis, or interpretation of data, revision for critically important intellectual content, final approval of the version to be published, accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. Phillip Fleshner: substantial contributions to conception and design of the work, revision for critically important intellectual content, final approval of the version to be published, accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. Karen Zaghiyan: substantial contributions to conception and design of the work; acquisition, analysis or interpretation of data, drafting and revision for critically important intellectual content, final approval of the version to be published, accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Mujukian, A., Truong, A., Fleshner, P. et al. Long-term healing after complex anal fistula repair in patients with Crohn’s disease. Tech Coloproctol 24, 833–841 (2020). https://doi.org/10.1007/s10151-020-02238-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10151-020-02238-1