Abstract
Background
Surgical strategies for acute perforated diverticulitis with generalised peritonitis remain controversial. This study aimed to meta-analyse trials comparing primary resection and anastomosis (PRA) to Hartmann’s procedure (HP) for Hinchey III/IV diverticulitis.
Methods
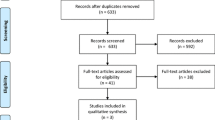
A systematic literature search was conducted to identify observational studies and randomised control trials (RCTs) of patients with Hinchey III/IV diverticulitis undergoing sigmoidectomy that compared PRA to HP. The methodological quality of the included studies was assessed systematically (Newcastle–Ottawa, Jadad and Cochrane risk of bias scores) and a meta-analysis was performed.
Results
After removal of duplicates, 12 studies including 4 RCTs were identified. The analysis included 918 patients, of whom 367 (39.98%) underwent PRA. Both the initial stoma rate (risk ratio [RR] persistent stoma 0.43, 95% confidence interval [CI] 0.26, 0.71, p = 0.001; I2 = 99%, p < 0.0001) and the rate of permanent stoma after combining the first (emergency surgery) and second (stoma reversal) procedures were lower in the PRA group. There was no difference in in 30-day mortality; however, PRA resulted in a reduction in overall mortality as well as major complications after the initial operation (RR 0.67, 95% CI 0.46, 0.97, p = 0.03; I2 = 22%, p = 0.26), stoma reversal (RR 0.48, 95% CI 0.26, 0.92, p = 0.03; I2 = 0%, p = 0.58) and when combining both procedures (RR 0.67, 95% CI 0.51, 0.88, p = 0.005; I2 = 0%, heterogeneity p = 0.58). A subgroup analysis of stoma reversal rates using data from only RCTs were consistent (RR permanent stoma, 0.33, 95% CI 0.13, 0.85, p = 0.02; I2 = 77%, p = 0.004) with the findings of the overall analysis.
Conclusions
This meta-analysis demonstrates that PRA used in the management of haemodynamically stable patients with Hinchey grade III/IV diverticulitis leads to a lower overall persistent stoma rate, with reduced morbidity compared with the traditional management.












Similar content being viewed by others
References
Bharucha AE, Parthasarathy G, Ditah I et al (2015) Temporal trends in the incidence and natural history of diverticulitis: a population-based study. Am J Gastroenterol 110(11):1589–1596
Etzioni DA, Mack TM, Beart RW Jr, Kaiser AM (2009) Diverticulitis in the United States: 1998–2005: changing patterns of disease and treatment. Ann Surg 249(2):210–217
Feingold D, Steele SR, Lee S et al (2014) Practice parameters for the treatment of sigmoid diverticulitis. Dis Colon Rectum 57(3):284–294
Sheth AA, Longo W, Floch MH (2008) Diverticular disease and diverticulitis. Am J Gastroenterol 103(6):1550–1556
Tursi A, Brandimarte G, Giorgetti G, Elisei W, Maiorano M, Aiello F (2008) The clinical picture of uncomplicated versus complicated diverticulitis of the colon. Dig Dis Sci 53(9):2474–2479
Stollman NH, Raskin JB (1999) Diagnosis and management of diverticular disease of the colon in adults. Ad Hoc Practice Parameters. Committee of the American College of Gastroenterology. Am J Gastroenterol 94(11):3110–3121
Hernandez-Guerrero A, Abdo-Francis J, Brito-Lugo P, Dela Torre-Bravo A, Marin-Pineda R, Stoopen-Rometti M (2008) Gastroenterology diagnosis and treatment guidelines of diverticular disease of the colon. Clinical and diagnostic. Rev Gastroenterol Mex 73(4):258–260
Andersen JC, Bundgaard L, Elbrond H, Laurberg S, Walker LR, Stovring J (2012) Danish national guidelines for treatment of diverticular disease. Dan Med J 59(5):C4453
Kruis W, Germer CT, Leifeld L (2014) Diverticular disease: guidelines of the German society for gastroenterology, digestive and metabolic diseases and the German society for general and visceral surgery. Digestion 90(3):190–207
Cuomo R, Barbara G, Pace F et al (2014) Italian consensus conference for colonic diverticulosis and diverticular disease. United Eur Gastroenterol J 2(5):413–442
Shahedi K, Fuller G, Bolus R et al (2013) Long-term risk of acute diverticulitis among patients with incidental diverticulosis found during colonoscopy. Clin Gastroenterol Hepatol 11(12):1609–1613
Stollman N, Smalley W, Hirano I (2015) American gastroenterological association institute guideline on the management of acute diverticulitis. Gastroenterology 149(7):1944–1949
Zorcolo L, Covotta L, Carlomagno N, Bartolo DC (2003) Safety of primary anastomosis in emergency colo-rectal surgery. Colorectal Dis 5(3):262–269
Bielecki K, Kaminski P, Klukowski M (2002) Large bowel perforation: morbidity and mortality. Tech Coloproctol 6(3):177–182
Krukowski ZH, Matheson NA (1984) Emergency surgery for diverticular disease complicated by generalized and faecal peritonitis: a review. Br J Surg 71(12):921–927
Hinchey EJ, Schaal PG, Richards GK (1978) Treatment of perforated diverticular disease of the colon. Adv Surg 12:85–109
Sher ME, Agachan F, Bortul M, Nogueras JJ, Weiss EG, Wexner SD (1997) Laparoscopic surgery for diverticulitis. Surg Endosc 11(3):264–267
Salem L, Anaya DA, Roberts KE, Flum DR (2005) Hartmann's colectomy and reversal in diverticulitis: a population-level assessment. Dis Colon Rectum 48(5):988–995
Constantinides VA, Heriot A, Remzi F et al (2007) Operative strategies for diverticular peritonitis: a decision analysis between primary resection and anastomosis versus Hartmann's procedures. Ann Surg 245(1):94–103
Dandekar NV, McCann WJ (1969) Primary resection and anastomosis in the management of perforation of diverticulitis of the sigmoid flexure and diffuse peritonitis. Dis Colon Rectum 12(3):172–175
Zeitoun G, Laurent A, Rouffet F et al (2000) Multicentre, randomized clinical trial of primary versus secondary sigmoid resection in generalized peritonitis complicating sigmoid diverticulitis. Br J Surg 87(10):1366–1374
Greif JM, Fried G, McSherry CK (1980) Surgical treatment of perforated diverticulitis of the sigmoid colon. Dis Colon Rectum 23(7):483–487
O'Sullivan GC, Murphy D, O'Brien MG, Ireland A (1996) Laparoscopic management of generalized peritonitis due to perforated colonic diverticula. Am J Surg 171(4):432–434
Myers E, Hurley M, O'Sullivan GC, Kavanagh D, Wilson I, Winter DC (2008) Laparoscopic peritoneal lavage for generalized peritonitis due to perforated diverticulitis. Br J Surg 95(1):97–101
Taylor CJ, Layani L, Ghusn MA, White SI (2006) Perforated diverticulitis managed by laparoscopic lavage. ANZ J Surg 76(11):962–965
Hold M, Denck H, Bull P (1990) Surgical management of perforating diverticular disease in Austria. Int J Colorectal Dis 5(4):195–199
Thaler K, Neumann F, Gero A, Kreuzer W (2000) Utility of appropriate peritonitis grading in the surgical management of perforated sigmoid diverticulitis. Colorectal Dis 2(6):359–363
Schilling MK, Maurer CA, Kollmar O, Buchler MW (2001) Primary vs. secondary anastomosis after sigmoid colon resection for perforated diverticulitis (Hinchey Stage III and IV): a prospective outcome and cost analysis. Dis Colon Rectum 44(5):699–703 (discussion 703–695)
Gooszen AW, Gooszen HG, Veerman W et al (2001) Operative treatment of acute complications of diverticular disease: primary or secondary anastomosis after sigmoid resection. Eur J Surg 167(1):35–39
Regenet N, Pessaux P, Hennekinne S et al (2003) Primary anastomosis after intraoperative colonic lavage vs. Hartmann's procedure in generalized peritonitis complicating diverticular disease of the colon. Int J Colorectal Dis 18(6):503–507
Vermeulen J, Akkersdijk GP, Gosselink MP et al (2007) Outcome after emergency surgery for acute perforated diverticulitis in 200 cases. Digest Surg 24(5):361–366
Trenti L, Biondo S, Golda T et al (2011) Generalized peritonitis due to perforated diverticulitis: Hartmann's procedure or primary anastomosis? Int J Colorectal Dis 26(3):377–384
Alizai PH, Schulze-Hagen M, Klink CD et al (2013) Primary anastomosis with a defunctioning stoma versus Hartmann's procedure for perforated diverticulitis—a comparison of stoma reversal rates. Int J Colorectal Dis 28(12):1681–1688
Liang S, Russek K, Franklin ME Jr (2012) Damage control strategy for the management of perforated diverticulitis with generalized peritonitis: laparoscopic lavage and drainage vs. laparoscopic Hartmann's procedure. Surg Endosc 26(10):2835–2842
Karoui M, Champault A, Pautrat K, Valleur P, Cherqui D, Champault G (2009) Laparoscopic peritoneal lavage or primary anastomosis with defunctioning stoma for Hinchey 3 complicated diverticulitis: results of a comparative study. Dis Colon Rectum 52(4):609–615
Angenete E, Thornell A, Burcharth J et al (2016) Laparoscopic lavage is feasible and safe for the treatment of perforated diverticulitis with purulent peritonitis: the first results from the randomized controlled trial DILALA. Ann Surg 263(1):117–122
Schultz JK, Yaqub S, Wallon C et al (2015) Laparoscopic lavage vs primary resection for acute perforated diverticulitis: the SCANDIV randomized clinical trial. JAMA 314(13):1364–1375
Vennix S, Musters GD, Mulder IM et al (2015) Laparoscopic peritoneal lavage or sigmoidectomy for perforated diverticulitis with purulent peritonitis: a multicentre, parallel-group, randomised, open-label trial. Lancet 386(10000):1269–1277
Marshall JR, Buchwald PL, Gandhi J et al (2017) Laparoscopic lavage in the management of Hinchey grade III diverticulitis: a systematic review. Ann Surg 265(4):670–676
Cirocchi R, Di Saverio S, Weber DG et al (2017) Laparoscopic lavage versus surgical resection for acute diverticulitis with generalised peritonitis: a systematic review and meta-analysis. Tech Coloproctol 21(2):93–110
Shaikh FM, Stewart PM, Walsh SR, Davies RJ (2017) Laparoscopic peritoneal lavage or surgical resection for acute perforated sigmoid diverticulitis: a systematic review and meta-analysis. Int J Surg 38:130–137
Acuna SA, Wood T, Chesney TR et al (2018) Operative strategies for perforated diverticulitis: a systematic review and meta-analysis. Dis Colon Rectum 61(12):1442–1453
Cirocchi R, Afshar S, Shaban F et al (2018) Perforated sigmoid diverticulitis: Hartmann's procedure or resection with primary anastomosis—a systematic review and meta-analysis of randomised control trials. Tech Coloproctol 22(10):743–753
Shaban F, Carney K, McGarry K, Holtham S (2018) Perforated diverticulitis: To anastomose or not to anastomose? A systematic review and meta-analysis. Int J Surg 58:11–21
Gachabayov M, Oberkofler CE, Tuech JJ, Hahnloser D, Bergamaschi R (2018) Resection with primary anastomosis vs nonrestorative resection for perforated diverticulitis with peritonitis: a systematic review and meta-analysis. Colorectal Dis 20(9):753–770
Lambrichts DPV, Vennix S, Musters GD et al (2019) Hartmann's procedure versus sigmoidectomy with primary anastomosis for perforated diverticulitis with purulent or faecal peritonitis (LADIES): a multicentre, parallel-group, randomised, open-label, superiority trial. Lancet Gastroenterol Hepatol 20:20
Lee JM, Bai PCJ, El Hechi M et al (2019) Hartmann's procedure vs primary anastomosis with diverting loop ileostomy for acute diverticulitis: nationwide analysis of 2,729 emergency surgery patients. J Am Coll Surg 20:20
Moher D, Liberati A, Tetzlaff J, Altman DG (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ 339:b2535
Stroup DF, Berlin JA, Morton SC et al (2000) Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis of observational studies in epidemiology (MOOSE) group. JAMA 283(15):2008–2012
Dindo D, Demartines N, Clavien P-A (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240(2):205–213
Higgins JP, Altman DG, Gotzsche PC et al (2011) The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ 343:d5928
Guyatt G, Oxman AD, Akl EA et al (2011) GRADE guidelines: 1. Introduction-GRADE evidence profiles and summary of findings tables. J Clin Epidemiol 64(4):383–394
Hozo SP, Djulbegovic B, Hozo I (2005) Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol 5:13
Luo D, Wan X, Liu J, Tong T (2018) Optimally estimating the sample mean from the sample size, median, mid-range, and/or mid-quartile range. Stat Methods Med Res 27(6):1785–1805
Wan X, Wang W, Liu J, Tong T (2014) Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res Methodol 14(1):135
Oberkofler CE, Rickenbacher A, Raptis DA et al (2012) A multicenter randomized clinical trial of primary anastomosis or Hartmann's procedure for perforated left colonic diverticulitis with purulent or fecal peritonitis. Ann Surg 256(5):819–826 (discussion 826–817)
Bridoux V, Regimbeau JM, Ouaissi M et al (2017) Hartmann's procedure or primary anastomosis for generalized peritonitis due to perforated diverticulitis: a prospective multicenter randomized trial (DIVERTI). J Am Coll Surg 225(6):798–805
Binda GA, Karas JR, Serventi A et al (2012) Primary anastomosis vs nonrestorative resection for perforated diverticulitis with peritonitis: a prematurely terminated randomized controlled trial. Colorect Dis 14(11):1403–1410
Richter S, Lindemann W, Kollmar O, Pistorius GA, Maurer CA, Schilling MK (2006) One-stage sigmoid colon resection for perforated sigmoid diverticulitis (Hinchey stages III and IV). World J Surg 30(6):1027–1032
Downing A, Morris EJ, Richards M et al (2015) Health-related quality of life after colorectal cancer in England: a patient-reported outcomes study of individuals 12 to 36 months after diagnosis. J Clin Oncol 33(6):616–624
Banerjee S, Leather AJ, Rennie JA, Samano N, Gonzalez JG, Papagrigoriadis S (2005) Feasibility and morbidity of reversal of Hartmann's. Colorectal Dis 7(5):454–459
Aziz O, Constantinides V, Tekkis PP et al (2006) Laparoscopic versus open surgery for rectal cancer: a meta-analysis. Ann Surg Oncol 13(3):413–424
Tilney HS, Sains PS, Lovegrove RE, Reese GE, Heriot AG, Tekkis PP (2007) Comparison of outcomes following ileostomy versus colostomy for defunctioning colorectal anastomoses. World J Surg 31(5):1142–1151
Caille C, Collard M, Moszkowicz D, AlDJ P, Maggiori L, Panis Y (2019) Reversal of Hartmann's procedure in patients following failed colorectal or coloanal anastomosis: an analysis of 45 consecutive cases. Colorectal Dis 20:20
Levack MM, Savitt LR, Berger DL et al (2012) Sigmoidectomy syndrome? Patients' perspectives on the functional outcomes following surgery for diverticulitis. Dis Colon Rectum 55(1):10–17
Jimenez-Rodriguez RM, Segura-Sampedro JJ, Rivero-Belenchon I et al (2017) Is the interval from surgery to ileostomy closure a risk factor for low anterior resection syndrome? Colorectal Dis 19(5):485–490
Stollman N, Raskin JB (2004) Diverticular disease of the colon. Lancet 363(9409):631–639
Breitenstein S, Kraus A, Hahnloser D, Decurtins M, Clavien PA, Demartines N (2007) Emergency left colon resection for acute perforation: primary anastomosis or Hartmann's procedure? A case-matched control study. World J Surg 31(11):2117–2124
Wong WD, Wexner SD, Lowry A et al (2000) Practice parameters for the treatment of sigmoid diverticulitis—supporting documentation. The Standards Task Force. The American Society of Colon and Rectal Surgeons. Dis Colon Rectum 43(3):290–297
Binda G, Karas J, Serventi A, Bergamaschi R, Amato A (2011) Primary anastomosis versus Hartmann's for perforated diverticulitis: a randomized controlled trial [Journal: Conference Abstract]. Colorectal Dis 13:5. https://doi.org/10.1111/j.1463-1318.2011.02704.x
Boyd-Carson H, Doleman B, Herrod PJJ et al (2019) Association between surgeon special interest and mortality after emergency laparotomy. Br J Surg 106(7):940–948
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no external funding or conflict of interests to declare.
Ethical Approval
This article does not contain any studies with human participants or animals performed by any of the authors. Institutional review board approval was not required due to the studies meta-analytic and retrospective nature.
Informed consent
For this type of study formal consent is not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ryan, O.K., Ryan, É.J., Creavin, B. et al. Systematic review and meta-analysis comparing primary resection and anastomosis versus Hartmann’s procedure for the management of acute perforated diverticulitis with generalised peritonitis. Tech Coloproctol 24, 527–543 (2020). https://doi.org/10.1007/s10151-020-02172-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10151-020-02172-2