Abstract
Background
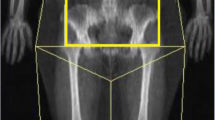
Obese patients have higher complication rates after pelvic surgery. Laparoscopic rectal surgery may not be possible in the obese individual due to mesorectal, total pelvic and general visceral fat volumes. Very low energy diets reduce visceral fat but the changes within the pelvis and mesorectum are unknown. The aim of the present study was to quantify the proportion of fat lost from total pelvic and mesorectal fat with a very low energy diet (VLED) and define simple, accessible measurements that correlate with expected volume reduction.
Methods
A study was conducted on proportion change in mesorectal and intrapelvic fat volumes in patients on a VLED prior to bariatric surgery at the Alfred Hospital in Melbourne. The VLED was a standardized 4-week meal replacement. Proportion change in mesorectal and intrapelvic fat volumes were measured. Patients had standardized pre-diet and post-diet magnetic resonance imaging (MRI) of the pelvis. Body mass index, weight and girth measures were obtained. Adipose quantification analysis was performed using Q-Fat.
Results
Nine patients were included in this study, who were preparing for bariatric (not colorectal) surgery (5 females, median age 42 years, range 27–59 years) pre-protocol body mass index was 55.8 (range 39.5–60.6 kg/m2); median weight was 163 kg. Median mesorectal fat reduction was 29.9% (range 11.6–66.6%). Linear regression showed a relationship between the amount of mesorectal fat reduction and two variables: patient height and the distance from S1 to the posterior aspect of the rectum on MRI. The relationship predicted response to the diet (R2 67%, p = 0.040).
Conclusions
Very low energy diets result in a clinically significant reduction in mesorectal fat with a lesser change in total pelvic fat, suggesting that very low energy diets may be useful for preparation for pelvic surgery in the obese. The distance from S1 to the posterior rectum correlates well with mesorectal reduction, making this a valuable clinical tool when volumetric analysis is not possible. This analysis is limited to the quantification of the effect of the diet and cannot comment on the safety of this approach before pelvic cancer surgery.


Similar content being viewed by others
Change history
26 September 2019
Due to substantial contributions by Dr. Phillip Malouf and Dr. Stephen Bell
References
Organisation WH (2016) Obesity and overweight. World Health Organisation. http://www.who.int/mediacentre/factsheets/fs311/en/2016. Accessed 1 June 2018
Kang J, Baek SE, Kim T et al (2012) Impact of fat obesity on laparoscopic total mesorectal excision: more reliable indicator than body mass index. Int J Colorectal Dis 27(4):497–505. https://doi.org/10.1007/s00384-011-1333-2
Benoist S, Panis Y, Alves A et al (2000) Impact of obesity on surgical outcomes after colorectal resection. Am J Surg 179:275–281
Gendall KA, Raniga S, Kennedy R et al (2007) The impact of obesity on outcome after major colorectal surgery. Dis Colon Rectum 50(12):2223–2237. https://doi.org/10.1007/s10350-007-9051-0
Mrak K, Eberl T, Fritz J et al (2012) Influence of body mass index on postoperative complications after rectal resection for carcinoma. South Med J 105(10):493–499. https://doi.org/10.1097/SMJ.0b013e3182666f09
Rickles AS, Iannuzzi JC, Mironov O et al (2013) Visceral obesity and colorectal cancer: are we missing the boat with BMI? J Gastrointest Surg 17(1):133–143. https://doi.org/10.1007/s11605-012-2045-9 (discussion p 43)
Poulsen M, Ovesen H (2012) Is laparoscopic colorectal cancer surgery in obese patients associated with an increased risk? Short-term results from a single center study of 425 patients. J Gastrointest Surg 16(8):1554–1558. https://doi.org/10.1007/s11605-012-1928-0
Christiansen T, Paulsen SK, Bruun JM et al (2009) Comparable reduction of the visceral adipose tissue depot after a diet-induced weight loss with or without aerobic exercise in obese subjects: a 12-week randomized intervention study. Eur J Endocrinol 160(5):759–767. https://doi.org/10.1530/EJE-08-1009
Mark CL, Phillips ML, Slavotinek JP et al (2006) Change in liver size and fat content after treatment with Optifast® very low calorie diet. Obes Surg 16:697–701
Nestle. The Optifast very low calorie diet program. http://nestlehelthscience.com.au
Chen B, Zhang Y, Zhao S, Yang T, Wu Q, Jin C, He Y, Wang Z (2016) The impact of general/visceral obesity on completion of mesorectum and perioperative outcomes of laparoscopic TME for rectal cancer: a STARD-compliant article. Medicine (Baltimore) 95(36):e4462
Yamaoka Y, Yamaguchi T, Kinugasa Y, Shiomi A, Kagawa H, Yamakawa Y, Furutani A, Manabe S, Torii K, Koido K, Mori K (2019) Mesorectal fat area as a useful predictor of the difficulty of robotic-assisted laparoscopic total mesorectal excision for rectal cancer. Surg Endosc 33(2):557–566
Warrier S, Bell S, Solomon M et al (2015) ADIPOSe ver 1.3 April 2015 LS. In: Bell S (ed) ADIPOSe trial protocol V2.1, June 2015 (unpublished)
Acknowledgements
The authors acknowledge the contribution of Mr Michael Sellenger, Radiographer in charge of the Alfred Hospital MRI unit.
Funding
This project was entirely funded by a Grant from the Colorectal society of Australia and New Zealand Foundation (CSSANZ). This paper has been accepted as a poster presentation at ASCRS June 10–14, 2017, Seattle, USA.
Author information
Authors and Affiliations
Contributions
All listed authors contributed to design methodology, draft review, final approval for submission and all authors are accountable for the integrity of the work.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
Ethics approval was obtained.
Informed consent
All patients gave appropriate informed consent.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Bell, S., Malouf, P., Johnson, N. et al. Pelvic fat volume reduction with preoperative very low energy diet (VLED): implications for rectal cancer surgery in the obese. Tech Coloproctol 23, 887–892 (2019). https://doi.org/10.1007/s10151-019-02074-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10151-019-02074-y