Abstract
Background
This study aimed to determine if the nature of circumferential resection margin (CRM) involvement, either by tumour or lymph nodes, had an impact upon local recurrence and survival in rectal cancer.
Methods
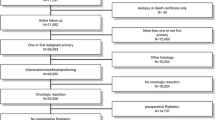
A retrospective analysis of a prospectively collected database was performed. Consecutive patients with stage I-III rectal cancer having curative surgery were included. All specimens were analysed by a single histopathologist. Statistical analysis was performed using chi-squared test and Kaplan–Meier.
Results
Of 265 patients, 29 (11%) had a positive CRM. Compared to patients with a negative CRM, a positive margin due to tumour was associated with a higher 5-year cumulative incidence of local recurrence (43.7% versus 8.8%, p = 0.001) and distant metastases (62% versus 13.6%, p = 0.001) with poorer 5-year cancer-specific survival (32% versus 87.8%, p = 0.001). Although patients with margin positivity due to lymph nodes had a higher rate of distant metastases (41.3% versus 13.6%, p = 0.004) and poorer 5-year cancer-specific survival (59.3% versus 87.8%, p = 0.038), the rate of local recurrence was comparable to that of patients with negative margins (8.3% versus 8.8%, p = 0.694).
Conclusions
Our findings suggest that the nature of CRM involvement may be important in determining prognosis in rectal cancer. Local recurrence is higher only when there is tumour present at the margin. Lymph node involvement of the margin confers similar risk of local recurrence to patients with CRM-negative, node-positive disease. These results need further evaluation in multicentre, prospective studies.


Similar content being viewed by others
References
Parfitt JR, Driman DK (2007) The total mesorectal excision specimen for rectal cancer: a review of its pathological assessment. J Clin Pathol 60(8):849–855
Quirke P, Durdey P, Dixon MF, Williams NS (1986) Local recurrence of rectal adenocarcinoma due to inadequate surgical resection. Histopathological study of lateral tumour spread and surgical excision. Lancet 2(8514):996–999
Birbeck KF, Macklin CP, Tiffin NJ, Parsons W, Dixon MF, Mapstone NP et al (2002) Rates of circumferential resection margin involvement vary between surgeons and predict outcomes in rectal cancer surgery. Ann Surg 235(4):449–457
Bernstein TE, Endreseth BH, Romundstad P, Wibe A, Group NCC (2009) Circumferential resection margin as a prognostic factor in rectal cancer. Br J Surg 96(11):1348–1357
Heald RJ, Ryall RD (1986) Recurrence and survival after total mesorectal excision for rectal cancer. Lancet 1(8496):1479–1482
Sauer R, Becker H, Hohenberger W, Rödel C, Wittekind C, Fietkau R et al (2004) Preoperative versus postoperative chemoradiotherapy for rectal cancer. N Engl J Med 351(17):1731–1740
van Gijn W, Marijnen CA, Nagtegaal ID, Kranenbarg EM, Putter H, Wiggers T et al (2011) Preoperative radiotherapy combined with total mesorectal excision for resectable rectal cancer: 12-year follow-up of the multicentre, randomised controlled TME trial. Lancet Oncol 12(6):575–582
Tilney HS, Tekkis PP, Sains PS, Constantinides VA, Heriot AG, Ireland AoCoGBa (2007) Factors affecting circumferential resection margin involvement after rectal cancer excision. Dis Colon Rectum 50(1):29–36
Youssef H, Collantes EC, Rashid SH, Wong LS, Baragwanath P (2009) Rectal cancer: involved circumferential resection margin—a root cause analysis. Colorectal Dis 11(5):470–474
Rickles AS, Dietz DW, Chang GJ, Wexner SD, Berho ME, Remzi FH et al (2015) High rate of positive circumferential resection margins following rectal cancer surgery: a call to action. Ann Surg 262(6):891–898
Hall NR, Finan PJ, al-Jaberi T, Tsang CS, Brown SR, Dixon MF et al (1998) Circumferential margin involvement after mesorectal excision of rectal cancer with curative intent. Predictor of survival but not local recurrence? Dis Colon Rectum 41(8):979–983
Nikberg M, Kindler C, Chabok A, Letocha H, Shetye J, Smedh K (2015) Circumferential resection margin as a prognostic marker in the modern multidisciplinary management of rectal cancer. Dis Colon Rectum 58(3):275–282
Tilly C, Lefevre JH, Svrcek M, Shields C, Flejou JF, Tiret E, Parc Y (2014) R1 rectal resection: look up and don’t look down. Ann Surg 260(5):794–799
Nagtegaal ID, Marijnen CA, Kranenbarg EK, van de Velde CJ, van Krieken JH, Committee PR et al (2002) Circumferential margin involvement is still an important predictor of local recurrence in rectal carcinoma: not one millimeter but two millimeters is the limit. Am J Surg Pathol 26(3):350–357
Association of Coloproctology of Great Britain and Ireland (2007). Guidelines for the management of colorectal cancer. 3rd edn. https://www.acpgbi.org.uk
Langman G, Patel A, Bowley DM (2015) Size and distribution of lymph nodes in rectal cancer resection specimens. Dis Colon Rectum 58(4):406–414
Adam IJ, Mohamdee MO, Martin IG, Scott N, Finan PJ, Johnston D et al (1994) Role of circumferential margin involvement in the local recurrence of rectal cancer. Lancet 344(8924):707–711
Wibe A, Møller B, Norstein J, Carlsen E, Wiig JN, Heald RJ et al (2002) A national strategic change in treatment policy for rectal cancer–implementation of total mesorectal excision as routine treatment in Norway. A national audit. Dis Colon Rectum 45(7):857–866
Wibe A, Syse A, Andersen E, Tretli S, Myrvold HE, Søreide O et al (2004) Oncological outcomes after total mesorectal excision for cure for cancer of the lower rectum: anterior vs. abdominoperineal resection. Dis Colon Rectum 47(1):48–58
Tekkis PP, Heriot AG, Smith J, Thompson MR, Finan P, Stamatakis JD et al (2005) Comparison of circumferential margin involvement between restorative and nonrestorative resections for rectal cancer. Colorectal Dis 7(4):369–374
Nagtegaal ID, Quirke P (2008) What is the role for the circumferential margin in the modern treatment of rectal cancer? J Clin Oncol 26(2):303–312
Phang PT, McGahan CE, McGregor G, MacFarlane JK, Brown CJ, Raval MJ et al (2010) Effects of change in rectal cancer management on outcomes in British Columbia. Can J Surg 53(4):225–231
Al-Sukhni E, Attwood K, Gabriel E, Nurkin SJ (2016) Predictors of circumferential resection margin involvement in surgically resected rectal cancer: a retrospective review of 23,464 patients in the US National Cancer Database. Int J Surg 28:112–117
Shihab OC, Quirke P, Heald RJ, Moran BJ, Brown G (2010) Magnetic resonance imaging-detected lymph nodes close to the mesorectal fascia are rarely a cause of margin involvement after total mesorectal excision. Br J Surg 97(9):1431–1436
Acknowledgements
We would like to thank the colorectal multidisciplinary teams at Heartlands Hospital and Good Hope Hospital who were responsible for treating the patients investigated in this study.
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This study does not require direct contact with human participants or animals.
Informed consent
For this type of study, informed consent is not required.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Patel, A., Green, N., Sarmah, P. et al. The clinical significance of a pathologically positive lymph node at the circumferential resection margin in rectal cancer. Tech Coloproctol 23, 151–159 (2019). https://doi.org/10.1007/s10151-019-01947-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10151-019-01947-6