Abstract
Background
Minimally invasive surgery is associated with several patient-related benefits, including reduced length of hospital stay and reduced blood loss. Robotic-assisted surgery offers many advantages when compared with standard laparoscopic procedures, including a stable three-dimensional binocular camera platform, motion smoothing and motion scaling, improved dexterity and ergonomics. There are limited data on the effectiveness of the dual-console DaVinci Xi platform for teaching resident surgeons. The goal of this study was to examine preliminary outcomes following the introduction of a dual-console robotic platform in our institution.
Methods
A retrospective review of our prospectively maintained patient database was performed. The first ten dual-console resident-performed procedures in colorectal surgery were compared with matched cases performed on a single console by the trainer. Patient demographics, operative times and patient outcomes were compared.
Results
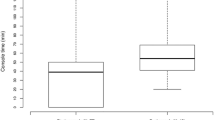
Twenty patients were included in this study. There was no significant difference in console time (p = 0.46) or total operative time (p = 0.52) when residents and trainers were compared. Patient outcomes were equivalent, with no difference in length of stay, morbidity or mortality.
Conclusions
The DaVinci Xi dual-console platform is a safe and effective platform for training junior surgeons. The dual-console system has the potential to alter surgical training pathways.


Similar content being viewed by others
References
Becker A, Pradel L, Kluth L et al (2015) Laparoscopic versus open partial nephrectomy for clinical T1 renal masses: no impact of surgical approach on perioperative complications and long-term postoperative quality of life. World J Urol 33(3):421–426
Guillou PJ, Quirke P, Thorpe H et al (2005) Short-term endpoints of conventional versus laparoscopic-assisted surgery in patients with colorectal cancer (MRC CLASICC trial): multicentre, randomised controlled trial. Lancet 365(9472):1718–1726
Bonjer HJ, Deijen CL, Haglind E, COLOR II Study Group (2015) A randomized trial of laparoscopic versus open surgery for rectal cancer. N Engl J Med 373(2):194
Green BL, Marshall HC, Collinson F et al (2014) Long-term follow-up of the Medical Research Council CLASICC trial of conventional versus laparoscopically assisted resection in colorectal cancer. Br J Surg 100(1):75–82
Kuhry E, Schwenk WF, Gaupset R, Romild U, Bonjer HJ (2008) Long-term results of laparoscopic colorectal cancer resection. Cochrane Database Syst Rev 16(2):CD003432
Schootman M, Hendren S, Ratnapradipa K, Stringer L, Davidson NO (2016) Adoption of robotic technology for treating colorectal cancer. Dis Colon Rectum 59(11):1011–1018
Denoya P, Wang H, Sands D, Nogueras J, Weiss E, Wexner SD (2010) Short-term outcomes of laparoscopic total mesorectal excision following neoadjuvant chemoradiotherapy. Surg Endosc 24(4):933–938
Sara S, Poncet G, Voirin D, Laverriere MH, Anglade D, Faucheron JL (2010) Can adequate lymphadenectomy be obtained by laparoscopic resection in rectal cancer? Results of a case-control study in 200 patients. J Gastrointest Surg 14(8):1244–1247
Zhang X, Wei Z, Bie M, Peng X, Chen C (2016) Robot-assisted versus laparoscopic-assisted surgery for colorectal cancer: a meta-analysis. Surg Endosc 30(12):5601–5614
Martinez-Perez A, Carra MC, Brunetti F, de’Angelis N (2017) Pathologic outcomes of laparoscopic vs open mesorectal excision for rectal cancer: a systematic review and meta-analysis. JAMA Surg 152(4):e165665
Bosker R, Groen H, Hoff C, Totte E, Ploeg R, Pierie JP (2013) Early learning effect of residents for laparoscopic sigmoid resection. J Surg Educ 70(2):200–205
Major P, Wysocki M, Dworak J, Pędziwiatr M, Małczak P, Budzyński A (2016) Are bariatric operations performed by residents safe and efficient? Surg Obes Relat Dis 13(4):614–621
Kiran RP, Ahmed Ali U, Coffey JC, Vogel JD, Pokala N, Fazio VW (2012) Impact of resident participation in surgical operations on postoperative outcomes: national surgical quality improvement program. Ann Surg 256(3):469–475
Dull MB, Gier CP, Carroll JT, Hutchison DD, Hobbs DJ, Gavel JC et al (2016) Resident impact on operative duration for elective general surgical procedures. Am J Surg 213(3):456–459
Nijhof HW, Silvis R, Vuylsteke RCLM, Oosterling SJ, Rijna H, Stockmann HBAC (2016) Training residents in laparoscopic colorectal surgery: is supervised surgery safe? Surg Endosc 31(6):2602–2606
Wexner T, Rosales-Velderrain A, Wexner SD, Rosenthal RJ (2016) Does implementing a general surgery residency program and resident involvement affect patient outcomes and increase care-associated charges? Am J Surg 214(1):147–151
Jimenez-Rodriguez RM, Rubio-Dorado-Manzanares M, Díaz-Pavón JM et al (2016) Learning curve in robotic rectal cancer surgery: current state of affairs. Int J Colorectal Dis 31(12):1807–1815
Guend H, Widmar M, Patel S et al (2016) Developing a robotic colorectal cancer surgery program: understanding institutional and individual learning curves. Surg Endosc 31(7):2820–2828
Foo CC, Law WL (2016) The learning curve of robotic-assisted low rectal resection of a novice rectal surgeon. World J Surg 40(2):456–462
Coffey JC, Lavery I, Sehgal R (2017) Mesenteric principles of gastrointestinal surgery: basic and applied science, 1st edn. CRC Press, London, p 357
Ladapo JA, Horwitz JR, Weinstein MC, Gazelle GS, Cutler DM (2009) Adoption and spread of new imaging technology: a case study. Health Aff (Millwood) 28(6):w1122–w1132
McHugh M, Osei-Anto A, Klabunde CN, Galen BA (2011) Adoption of CT colonography by US hospitals. J Am Coll Radiol 8(3):169–174
Silva-Velazco J, Dietz DW, Stocchi L et al (2017) Considering value in rectal cancer surgery: an analysis of costs and outcomes based on the open, laparoscopic, and robotic approach for proctectomy. Ann Surg 265(5):960–968
Jolley J, Lomelin D, Simorov A, Tadaki C, Oleynikov D (2016) Resident involvement in laparoscopic procedures does not worsen clinical outcomes but may increase operative times and length of hospital stay. Surg Endosc 30(9):3783–3791
Rothman JP, Burcharth J, Pommergaard HC, Bardram L, Rosenberg J (2015) Less surgical experience has no impact on mortality and morbidity after laparoscopic cholecystectomy: a prospective cohort analysis. Surg Laparosc Endosc Percutan Tech 25(6):492–495
Mikhail E, Salemi JL, Hart S, Imudia AN (2016) Comparing single and dual console systems in the robotic surgical training of graduating OB/GYN residents in the United States. Minim Invasive Surg. doi:10.1155/2016/5190152
Morgan MS, Shakir NA, Garcia-Gil M et al (2015) Single-versus dual-console robot-assisted radical prostatectomy: impact on intraoperative and postoperative outcomes in a teaching institution. World J Urol 33(6):781–786
Smith AL, Scott EM, Krivak TC, Olawaiye AB, Chu T, Richard SD (2013) Dual-console robotic surgery: a new teaching paradigm. J Robot Surg 7(2):113–118
Park IJ, Choi GS, Lim KH, Kang BM, Jun SH (2009) Multidimensional analysis of the learning curve for laparoscopic resection in rectal cancer. J Gastrointest Surg 13(2):275–281
Tekkis PP, Senagore AJ, Delaney CP, Fazio VW (2005) Evaluation of the learning curve in laparoscopic colorectal surgery: comparison of right-sided and left-sided resections. Ann Surg 242(1):83–91
Fergo C, Burcharth J, Pommergaard HC, Kildebro N, Rosenberg J (2017) Three-dimensional laparoscopy vs 2-dimensional laparoscopy with high-definition technology for abdominal surgery: a systematic review. Am J Surg 213(1):159–170
Coffey JC, O’Leary DP (2016) The mesentery: structure, function, and role in disease. Lancet Gastroenterol Hepatol 1(3):238–247
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
Ethical approval was provided by the local ethics committee.
Informed consent
All patients gave consent for inclusion.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary material 1 (MP4 98819 kb)
Rights and permissions
About this article
Cite this article
Bolger, J.C., Broe, M.P., Zarog, M.A. et al. Initial experience with a dual-console robotic-assisted platform for training in colorectal surgery. Tech Coloproctol 21, 721–727 (2017). https://doi.org/10.1007/s10151-017-1687-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10151-017-1687-8