Abstract
Background
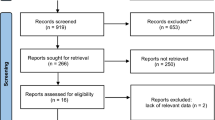
The optimal time of rectal resection after long-course chemoradiotherapy (CRT) remains unclear. A feasibility study was undertaken for a multi-centre randomized controlled trial evaluating the impact of the interval after chemoradiotherapy on the technical complexity of surgery.
Methods
Patients with rectal cancer were randomized to either a 6- or 12-week interval between CRT and surgery between June 2012 and May 2014 (ISRCTN registration number: 88843062). For blinded technical complexity assessment, the Observational Clinical Human Reliability Analysis technique was used to quantify technical errors enacted within video recordings of operations. Other measured outcomes included resection completeness, specimen quality, radiological down-staging, tumour cell density down-staging and surgeon-reported technical complexity.
Results
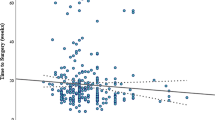
Thirty-one patients were enrolled: 15 were randomized to 6 and 16–12 weeks across 7 centres. Fewer eligible patients were identified than had been predicted. Of 23 patients who underwent resection, mean 12.3 errors were observed per case at 6 weeks vs. 10.7 at 12 weeks (p = 0.401). Other measured outcomes were similar between groups.
Conclusions
The feasibility of measurement of operative performance of rectal cancer surgery as an endpoint was confirmed in this exploratory study. Recruitment of sufficient numbers of patients represented a challenge, and a proportion of patients did not proceed to resection surgery. These results suggest that interval after CRT may not substantially impact upon surgical technical performance.


Similar content being viewed by others
References
Francois Y, Nemoz CJ, Baulieux J et al (1999) Influence of the interval between preoperative radiation therapy and surgery on downstaging and on the rate of sphincter-sparing surgery for rectal cancer: the Lyon R90-01 randomized trial. J Clin Oncol 17:2396
Foster JD, Jones EL, Falk S, Copper EJ, Francis NK (2013) Timing of surgery after long-course neoadjuvant chemoradiotherapy for rectal cancer: a systematic review of the literature. Dis Colon Rectum 56:921–930
Miskovic D, Ni M, Wyles SM, Parvaiz A, Hanna GB (2012) Observational clinical human reliability analysis (OCHRA) for competency assessment in laparoscopic colorectal surgery at the specialist level. Surg Endosc 26:796–803
Talebpour M, Alijani A, Hanna GB, Moosa Z, Tang B, Cuschieri A (2009) Proficiency-gain curve for an advanced laparoscopic procedure defined by observation clinical human reliability assessment (OCHRA). Surg Endosc 23:869–875
Wilson PJ (2015) Use of human reliability analysis to evaluate surgical technique for rectal cancer. Ph.D. Thesis, University of Dundee, 2012. http://discovery.dundee.ac.uk/portal/files/1299820/Wilson_phd_2012.pdf
Joice P, Hanna GB, Cuschieri A (1998) Errors enacted during endoscopic surgery—a human reliability analysis. Appl Ergon 29:409–414
Tang B, Hanna GB, Cuschieri A (2005) Analysis of errors enacted by surgical trainees during skills training courses. Surgery 138:14–20
Miskovic D, Foster JD, Agha A et al (2015) Standardisation of laparoscopic total mesorectal excision for rectal cancer—a structured international expert consensus. Ann Surg 261:716–722
Foster JD, Miskovic D, Allison AS et al (2016) Application of objective clinical human reliability analysis (OCHRA) in assessment of technical performance in laparoscopic rectal cancer surgery. Tech Coloproctol. doi:10.1007/s10151-016-1444-4
Wittekind C, Compton C, Quirke P et al (2009) A uniform residual tumor (R) classification: integration of the R classification and the circumferential margin status. Cancer 115:3483–3488
Patel UB, Taylor F, Blomqvist L et al (2011) Magnetic resonance imaging-detected tumor response for locally advanced rectal cancer predicts survival outcomes: MERCURY experience. J Clin Oncol 29:3753–3760
Nagtegaal ID, van de Velde CJ, van der Worp E, Kapiteijn E, Quirke P, van Krieken JH, Cooperative Clinical Investigators of the Dutch Colorectal Cancer Group (2002) Macroscopic evaluation of rectal cancer resection specimen: clinical significance of the pathologist in quality control. J Clin Oncol 20:1729–1734
Williams GT, Quirke P, Shepherd NA (2007) Minimum dataset for colorectal cancer. Histopathology reports, 2nd edn. Royal College of Pathologists, London
West NP, Dattani M, McShane P et al (2010) The proportion of tumour cells is an independent predictor for survival in colorectal cancer patients. Br J Cancer 102:1519–1523
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240:205–213
Shapiro SS, Wilk MB (1965) An analysis of variance test for normality (complete samples). Biometrika 52:591–611
Tang B, Hanna GB, Bax NM, Cuschieri A (2004) Analysis of technical surgical errors during initial experience of laparoscopic pyloromyotomy by a group of Dutch pediatric surgeons. Surg Endosc 18:1716–1720
Tang B, Hanna GB, Joice P, Cuschieri A (2004) Identification and categorization of technical errors by Observational Clinical Human Reliability Assessment (OCHRA) during laparoscopic cholecystectomy. Arch Surg 139:1215–1220
Tang B, Hanna GB, Carter F, Adamson GD, Martindale JP, Cuschieri A (2006) Competence assessment of laparoscopic operative and cognitive skills: Objective Structured Clinical Examination (OSCE) or Observational Clinical Human Reliability Assessment (OCHRA). World J Surg 30:527–534
Ahmed K, Miskovic D, Darzi A, Athanasiou T, Hanna GB (2011) Observational tools for assessment of procedural skills: a systematic review. Am J Surg 202:469–480
Dolinsky CM, Mahmoud NN, Mick R et al (2007) Effect of time interval between surgery and preoperative chemoradiotherapy with 5-fluorouracil or 5-fluorouracil and oxaliplatin on outcomes in rectal cancer. J Surg Oncol 96:207–212
Wolthuis AM, Penninckx F, Haustermans K et al (2012) Impact of interval between neoadjuvant chemoradiotherapy and TME for locally advanced rectal cancer on pathologic response and oncologic outcome. Ann Surg Oncol 19:2833–2841
Evans J, Tait D, Swift I et al (2011) Timing of surgery following preoperative therapy in rectal cancer: the need for a prospective randomized trial? Dis Colon Rectum 54:1251–1259
Garcia-Aguilar J, Smith DD, Avila K, Bergsland EK, Chu P, Krieg RM, Timing of Rectal Cancer Response to Chemoradiation Consortium (2011) Optimal timing of surgery after chemoradiation for advanced rectal cancer: preliminary results of a multicenter, nonrandomized phase II prospective trial. Ann Surg 254:97–102
Lefevre JH, Rousseau A, Svrcek M, Parc Y, Simon T, Tiret E, French Research Group of Rectal Cancer Surgery (GRECCAR) (2013) A multicentric randomized controlled trial on the impact of lengthening the interval between neoadjuvant radiochemotherapy and surgery on complete pathological response in rectal cancer (GRECCAR-6 trial): rationale and design. BMC Cancer 13:417
Treasure T, Lang-Lazdunski L, Waller D et al (2011) Extra-pleural pneumonectomy versus no extra-pleural pneumonectomy for patients with malignant pleural mesothelioma: clinical outcomes of the Mesothelioma and Radical Surgery (MARS) randomised feasibility study. Lancet Oncol 12:763–772
Boulind CE, Ewings P, Bulley SH et al (2013) Feasibility study of analgesia via epidural versus continuous wound infusion after laparoscopic colorectal resection. Br J Surg 100:395–402
Avery KN, Metcalfe C, Berrisford R et al (2014) The feasibility of a randomized controlled trial of esophagectomy for esophageal cancer–the ROMIO (Randomized Oesophagectomy: Minimally Invasive or Open) study: protocol for a randomized controlled trial. Trials 15:200
Jones EL, Williams-Yesson BA, Hackett RC, Staniszewska SH, Evans D, Francis NK (2015) Quality of reporting on patient and public involvement within surgical research: a systematic review. Ann Surg 261:243–350
Acknowledgments
Patient recruitment and data collection were performed by clinical teams and research nurses at the participating research sites. We would like to thank the following clinicians, research nurses and administrators whose hard work is much appreciated: Louise Saunders, Katrina Kirby, Ann Lyons (North Bristol); Clare Adams, Mark Coleman, Laura Evenden, Hilary Rowley, Ellie Shepherd (Plymouth); Erica Beaumont, Joanne Taylor, Paul Mackey, Ian Eyre-Brooke (Taunton); Hema Arumugam, Darren Beech, Richard Ellis, Melanie Feldman, Philip Harvey, Kirsty Maclean, Nick Morley (Truro); Karen Bobruk, Rebecca Houlihan, Katrina Hurley, Catherine Philpott, Jonathan Randall, Mike Thomas (University Hospitals Bristol); Nitya Chandratreya, Deborah Coles, Harvey Dymond, Krishna Kandaswamy, Hugh Lloyd-Jones, Vivienne Pixton (Weston Super-Mare); additionally Brendan Moran and Siobhan Creanor for participating on the Steering Committee; Steve Gore, Nicky Marks, Joanna Allison, Andrea Bradshaw, Katie Spurdle, Hannah Thurlow and Tressy Pitt-Kerby for their help, support and assistance in undertaking this study. The TCD calculations were assisted by Emma Tinkler-Hundal, Dan Bottomley, Mike Hale, Dave Turner and Martin Waterhouse. Pathology and Tumour Biology at the University of Leeds is supported by Yorkshire Cancer Research, the Pathological Society of Great Britain and Ireland, the Academy of Medical Sciences, the Experimental Cancer Medicines Centre and the Medical Research Council.
The names of the "STARRCAT Investigators" Group are as follows: - Mr. Ponnandai Arumugam, Department of Surgery, Royal Cornwall Hospital, Truro, UK. - Mr. Anthony Dixon, Department of Surgery, North Bristol NHS Trust, Bristol, UK. - Mr. Tom Edwards, Department of Surgery, Musgrove Park Hospital, Taunton, UK. - Mr. Robert Longman, Department of Surgery, University Hospitals Bristol, Bristol, UK. - Dr. David Sherriff, Department of Oncology, Derriford Hospital, Plymouth, UK. - Mr. Reuben West, Department of Surgery, Weston General Hospital, Weston-Super-Mare, UK. - Mr. Andrew Allison, Department of Surgery, Yeovil District Hospital, Yeovil, UK. - Mr. Jonathan Ockrim, Department of Surgery, Yeovil District Hospital, Yeovil, UK.
Funding
This work was supported by the UK National Institute for Health Research, through the Research for Patient Benefit Program (Grant PB-PG-1010-23326). The funding body did not have any role in the planning of the study, recruitment, data collection or analysis.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
The study was approved by the South West England (Exeter) Research Ethics Committee (reference 12/SW/0112) and locally at recruiting centres. Patient representatives were consulted during trial design and protocol development and were active members of the study management group and steering committee.
Informed consent
Written informed consent was obtained prior to randomization and commencing CRT.
Rights and permissions
About this article
Cite this article
Foster, J.D., Ewings, P., Falk, S. et al. Surgical timing after chemoradiotherapy for rectal cancer, analysis of technique (STARRCAT): results of a feasibility multi-centre randomized controlled trial. Tech Coloproctol 20, 683–693 (2016). https://doi.org/10.1007/s10151-016-1514-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10151-016-1514-7