Abstract
Background
Natural orifice translumenal endoscopic surgery (NOTES) has always made more sense in the colorectal field where the target organ for entry houses the pathology. To address the question whether an adequate total mesorectal excision (TME) for rectal cancer can be performed from a transanal bottoms-up approach, we performed a case-matched study.
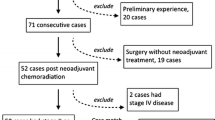
Methods
Starting in 2009, transanal TME (taTME) surgery was selectively used for rectal cancer after neoadjuvant therapy and prospectively entered into a database. Between March 2012 and February 2014, 17 consecutive taTME rectal cancer patients were identified and case-matched to multiport laparoscopic TME (MP TME) based on age, body mass index, uT stage, radiation dose, level in the rectum, and procedure. Perioperative outcomes, morbidity, mortality, local recurrence, completeness of TME, and radial and distal margins were analyzed. Statistically significant differences were identified using Student’s t test.
Results
There were 12 transanal abdominal transanal (TATA)/5 abdominoperineal resection procedures in each group. Data regarding overall/taTME/MP TME are as follows: % positive-circumferential margin: 2.9/0/5.9 % (p = 0.32). Distal margin: 0/0/0 %. Complete or near-complete TME: 97.1/100/94.1 % (p = 0.32). Incomplete TME 2.9/0/5.9 % (p = 0.32). Local recurrence: 2.9/5.9/0 % (p = 0.32). There were no perioperative mortalities. Morbidity in each group: 26.4/23.5/29.4 % (p = 0.79). There were no differences in perioperative or postoperative outcomes except days to clear liquids (1/2 days, p = 0.03) and largest incision length (1.3/2.6 cm, p = 0.05).
Conclusions
We demonstrated no differences in perioperative/postoperative outcomes or pathologic TME outcomes of transanal or bottoms-up TME compared to standard laparoscopic TME. TaTME is a promising progressive approach to NOTES and deserves additional evaluation.
Similar content being viewed by others
References
Marwan K, Staples MP, Thursfield V, Bell SW (2010) The rate of abdominoperineal resections for rectal cancer in the state of Victoria, Australia: a population-based study. Dis Colon Rectum 53:1645–1651
Enríquez-Navascués JM, Borda N, Lizerazu A et al (2011) Patterns of local recurrence in rectal cancer after a multidisciplinary approach. World J Gastroenterol 17:1674–1684
Heald RJ, Ryall RD (1986) Recurrence and survival after total mesorectal excision for rectal cancer. Lancet 327:1479–1482
MacFarlane JK, Ryall RD, Heald RJ (1993) Mesorectal excision for rectal cancer. Lancet 341:457
Quirke P, Steele R, Monson J et al (2009) Effect of the plane of surgery achieved on local recurrence in patients with operable rectal cancer: a prospective study using data from the MRC CR07 and NCIC-CTG CO16 randomised clinical trial. Lancet 373:821
Wibe A, Eriksen MT, Syse A, Myrvold HE, Søreide O, Norwegian Rectal Cancer Group (2003) Total mesorectal excision for rectal cancer: what can be achieved by a national audit? Colorectal Dis 5:471–477
Sebag-Montefiore D, Stephens RJ, Steele R et al (2009) Preoperative radiotherapy versus selective postoperative chemoradiotherapy in patients with rectal cancer (MRC CR07 and NCIC-CTG C016): a multicenter, randomized trial. Lancet 373:811–820
Folkesson J, Birgisson H, Pahlman L, Cedermark B, Glimelius B, Gunnarsson U (2005) Swedish rectal cancer trial: long lasting benefits from radiotherapy on survival and local recurrence rate. J Clin Oncol 23:5644–5650
Marks JH, Frenkel JL, D’Andrea AP, Greenleaf CE (2011) Maximizing rectal cancer results: TEM and TATA techniques to expand sphincter preservation. Surg Oncol Clin N Am 20:501–520
Ricciardi R, Roberts PL, Read TE, Marcello PW, Schoetz DJ, Baxter NN (2012) Variability in reconstructive procedures following rectal cancer surgery in the United States. Dis Colon Rectum 53:874–880
Kang CY, Halabi WJ, Luo R, Pigazzi A, Nguyen NT, Stamos MJ (2012) Laparoscopic colorectal surgery: a better look into the latest trends. Arch Surg 147:724–731
Moghadamyeghaneh Z, Carmichael JC, Mills S, Pigazzi A, Nguyen NT, Stamos MJ (2015) Variations in laparoscopic colectomy utilization in the United States. Dis Colon Rectum 58:950–956
Staudacher C, Vignali A (2010) Laparoscopic surgery for rectal cancer: the state of the art. World J Gastrointest Surg 2:275–282
Fleshman J, Branda M, Sargent DJ et al (2015) Effect of laparoscopic-assisted resection vs open resection of stage II or III rectal cancer on pathologic outcomes: the ACOSOG Z6051 randomized clinical trial. JAMA 314:1346–1355
Marks G, Mohiuddin M, Rakinic J (1991) New hope and promise for sphincter preservation in the management of cancer of the rectum. Semin Oncol 18:388–398
Marks G, Bannon J, Marks J (1996) Transanal-abdominal Transanal radical proctosigmoidectomy with coloanal anastomosis for distal rectal cancer. In: Baker R, Fisher J, Nyhus L (eds) Mastery of surgery, 3rd edn. Little, Brown and Company Inc, Boston, pp 1524–1534
Marks J, Mizrahi B, Dalane S, Nweze I, Marks G (2010) Laparoscopic transanal abdominal transanal resection with sphincter preservation for rectal cancer in the distal 3 cm of the rectum after neoadjuvant therapy. Surg Endosc 24:2700–2707
Marks JH, Frenkel JL, Greenleaf CE, D’Andrea AP (2014) Transanal endoscopic microsurgery with entrance into the peritoneal cavity: Is it safe? Dis Colon Rectum 57:1176–1182
Albert MR, Atallah SB, deBeche-Adams TC, Izfar S, Larach SW (2013) Transanal minimally invasive surgery (TAMIS) for local excision of benign neoplasms and early-stage rectal cancer: efficacy and outcomes in the first 50 patients. Dis Colon Rectum 56:301–307
Marks JH (2009) Transanal proctectomy using TEM endoscope: initial experience. Unpublished raw data
de Lacy AM, Rattner DW, Adelsdorfer C et al (2013) Transanal natural orifice transluminal endoscopic surgery (NOTES) rectal resection: “down-to-up” total mesorectal excision (TME)–short-term outcomes in the first 20 cases. Surg Endosc 27:3165–3172
Washington K, Berlin J, Branton P, Cancer Committee, College of American Pathologists et al (2008) Protocol for the examination of specimens from patients with primary carcinomas of the colon and rectum. Arch Pathol Lab Med 132:1182–1193
National Comprehensive Cancer Network (2016) NCCN clinical practice guidelines in oncology: rectal cancer. V.1.2016
Glynne-Jones R, Mawdsley S, Novell JR (2006) The clinical significance of the circumferential resection margin following preoperative pelvic chemo-radiotherapy in rectal cancer: why we need a common language. Colorectal Dis 8:800–807
Haggar F, Boushey R (2009) Colorectal cancer epidemiology: incidence, mortality, survival and risk factors. Clin Colon Rectal Surg 22:191–197
Onaitis MW, Noone RB, Hartwig M et al (2001) Neoadjuvant chemoradiation for rectal cancer: analysis of clinical outcomes from a 13-year institutional experience. Ann Surg 233:778–785
Marks GJ, Marks JH, Mohiuddin M, Brady L (1998) Radical sphincter preservation surgery with coloanal anastomosis following high-dose external irradiation for the very low lying rectal cancer. Recent Results Cancer Res 146:161–174
Marks G, Mohiuddin M, Masoni L et al (1992) High-dose preoperative radiation therapy as the key to extending sphincter preservation surgery for cancer of the distal rectum. Surg Oncol Clin N Am 1:71–85
Marks G, Mohiuddin M, Goldstein SD (1988) Sphincter preservation for cancer of the distal rectum using high dose preoperative radiation. Int J Radiat Oncol Biol Phys 15:1065–1068
Mohammed S, Anaya DA, Awad SS, Albo D, Berger DH, Artinyan A (2015) Sphincter preservation rates after radical resection for rectal cancer in the United States veteran population: opportunity for improvement in early disease. Ann Surg Oncol 22:216–223
Buess G, Theiss R, Günther M, Hutterer F, Pichlmaier H (1985) Endoscopic surgery in the rectum. Endoscopy 17:31–35
Buess G, Kipfmuller K, Ibald R et al (1988) Clinical results of transanal endoscopic microsurgery. Surg Endosc 2:245–250
Atallah S, Albert M, Larach S (2010) Transanal minimally invasive surgery: a giant leap forward. Surg Endosc 24:2200–2205
Steele SR, Maykel JA, Champagne BJ, Orangio GR (2014) Complexities in colorectal surgery: decision-making and management. Springer, New York
Zhou X, Su M, Hu K et al (2016) CT pelvimetry and clinicopathological parameters in evaluation of the technical difficulties in performing open rectal surgery for mid-low rectal cancer. Oncol Lett 11:31–38
Nagtegaal ID, van de Velde CJ, van der Worp E, Kapiteijn E, Quirke P, van Krieken JH, Cooperative Clinical Investigators of the Dutch Colorectal Cancer Group (2002) Macroscopic evaluation of rectal cancer resection specimen: clinical significance of the pathologist in quality control. J Clin Oncol 20:1729–1734
Parfitt JR, Driman DK (2007) The total mesorectal excision specimen for rectal cancer: a review of its pathological assessment. J Clin Pathol 60:849–855
Marks JH, Valsdottir EB, Rather AA, Nweze IC, Newman DA, Chernick MR (2010) Fewer than 12 lymph nodes can be expected in a surgical specimen after high-dose chemoradiation therapy for rectal cancer. Dis Colon Rectum 53:1023–1029
Stevenson AL, Solomon MJ, Lumley JW et al (2015) Effect of laparoscopic-assisted resection vs open resection on pathological outcomes in rectal cancer: the ALaCaRT randomized clinical trial. JAMA 314:1356–1363
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
The study was carried out to appropriate ethical standards.
Informed consent
Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
Rights and permissions
About this article
Cite this article
Marks, J.H., Montenegro, G.A., Salem, J.F. et al. Transanal TATA/TME: a case-matched study of taTME versus laparoscopic TME surgery for rectal cancer. Tech Coloproctol 20, 467–473 (2016). https://doi.org/10.1007/s10151-016-1482-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10151-016-1482-y