Abstract
Background
The single progesterone receptor (PR)-positive phenotype (estrogen receptor (ER)-/PR + , sPR positive) is an infrequent and independent biological entity. However, the prognosis of patients with sPR-positive and her-2-negative phenotype is still controversial, and it is not always easy to decide treatment strategies for them.
Methods
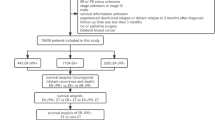
Patients during 2010–2014 were identified from Surveillance, Epidemiology, and End Results (SEER) database. The Kaplan–Meier method was used to evaluate cancer-specific survival (CSS). The propensity score matching (PSM) method was used to balance differences of characteristics in groups. The Life-Table method was used to calculate 5-year CSS rates and the annual hazard rate of death (HRD).
Results
A total of 97,527 patients were included, and only 745 (0.76%) patients were sPR-positive phenotype. The majority of sPR-positive breast cancer were basal-like subtype. Survival analysis showed that the sPR-positive breast cancer had similar prognosis comparing to double hormonal receptor-negative (ER-/PR-, dHoR-negative) breast cancer, and had the highest HRD during the initial 1–2 years of follow-up, then maintained the HRD of almost zero during the late years of follow-up.
Conclusions
The patients with sPR-positive and her-2-negative breast cancer, similar to dHoR-negative breast cancer, had a worse survival, and could benefit from chemotherapy significantly. However, the escalating endocrine therapy was not recommended for sPR-positive patients. The patients with sPR positive should be excluded from future clinical trials concerning endocrine therapy.




Similar content being viewed by others
References
Wl M (1973) Estrogen receptors in human breast cancer. J Clin Invest 52(1):73–77. https://doi.org/10.1172/Jci107175
Aaltomaa S, Lipponen P, Eskelinen M et al (1991) Hormone receptors as prognostic factors in female breast cancer. Ann Med. 23(6):643–8. https://doi.org/10.3109/07853899109148097
May E, Mouriesse H, May-Levin F et al (1990) Human breast cancer: identification of populations with a high risk of early relapse in relation to both oestrogen receptor status and C-Erbb-2 overexpression. British J Cancer. 62(3):430–5. https://doi.org/10.1038/Bjc.1990.312
Jm R, Lv B, Aj K et al (1985) Disease-Free Interval and estrogen receptor activity in tumor tissue of patients with primary breast cancer: analysis after long-term follow-up. Breast Cancer Res Treatm 6(2):123–130. https://doi.org/10.1007/Bf02235743.PubmedPmid:4052639
Chevallier B, Heintzmann F, Mosseri V et al (1988) Prognostic value of estrogen and progesterone receptors in operable breast-cancer - results of a univariate and multivariate-analysis. Cancer Am Cancer Soc. 62(12):2517–24. https://doi.org/10.1002/1097-0142
Alanko A, Heinonen E, Scheinin T et al (1985) Significance of estrogen and progesterone receptors, disease-free interval, and site of 1st metastasis on survival of breast-cancer patients. Cancer-Am Cancer Soc. 56(7):1696–700. https://doi.org/10.1002/1097-0142
Nadji M, Gomez-Fernandez C, Ganjei-Azar P et al (2005) Immunohistochemistry of estrogen and progesterone receptors reconsidered: experience with 5,993 breast cancers. Am JClin Pathol 123(1):21–7. https://doi.org/10.1309/4wv79n2ghj3x1841
Bardou VJ, Arpino G, Elledge RM et al (2003) Progesterone receptor status significantly improves outcome prediction over estrogen receptor status alone for adjuvant endocrine therapy in two large breast cancer databases. J Clin Oncol. 21(10):1973–9. https://doi.org/10.1200/Jco.2003.09.099
Ravdin PM, Green S, Dorr TM et al (1992) Prognostic-significance of progesterone-receptor levels in estrogen receptor-positive patients with metastatic breast-cancer treated with tamoxifen - results of a prospective southwest-oncology-group study. J Clin Oncol. 10(8):1284–91. https://doi.org/10.1200/Jco.1992.10.8.1284
Ck O, Mg Y, Wa K et al (1980) The value of estrogen and progesterone receptors in the treatment of breast-cancer. Cancer-Am Cancer Soc 46(12):2884–2888. https://doi.org/10.1002/1097-0142
Schroth W, Winter S, Buttner F et al (2016) Clinical outcome and global gene expression data support the existence of the estrogen receptor-negative/progesterone receptor-positive invasive breast cancer phenotype. Breast Cancer Res Treatm 155(1):85–97. https://doi.org/10.1007/S10549-015-3651-5
Ethier JL, Ocana A, Rodriguez Lescure A et al (2018) Outcomes of single versus double hormone receptor-positive breast cancer a geicam/9906 sub-study. Eur J Cancer. 94:199–205. https://doi.org/10.1016/J.Ejca.2018.02.018
Kuroda H, Muroi N, Hayashi M et al (2019) Oestrogen receptor-negative/progesterone receptor-positive phenotype of invasive breast carcinoma in japan: re-evaluated using immunohistochemical staining. Breast Cancer. 26(2):249–54. https://doi.org/10.1007/S12282-018-0898-9
Cserni G, Francz M, Kalman E et al (2011) Estrogen receptor negative and progesterone receptor positive breast carcinomas-How frequent are they? Pathol Oncol Res. 17(3):663–8. https://doi.org/10.1007/S12253-011-9366-Y
De Maeyer L, Van Limbergen E, De Nys K et al (2008) Does estrogen receptor negative/progesterone receptor positive breast carcinoma exist? J Clin Oncol. 26(2):335–6. https://doi.org/10.1200/Jco.2007.14.8411
Shen T, Brandwein-Gensler M, Hameed O et al (2015) Characterization of estrogen receptor-negative/progesterone receptor-positive breast cancer. Hum Pathol. 46(11):1776–84. https://doi.org/10.1016/J.Humpath.2015.07.019
Rhodes A, Jasani B (2009) the oestrogen receptor-negative/progesterone receptor-positive breast tumour: a biological entity or a technical artefact? J Clin Pathol 62(1):95–96. https://doi.org/10.1136/Jcp.2008.060723.PubmedPmid:19103868
Itoh M, Iwamoto T, Matsuoka J et al (2014) Estrogen receptor (Er) Mrna expression and molecular subtype distribution in er-negative/progesterone receptor-positive breast cancers. Breast Cancer Res Treatm 143(2):403–409. https://doi.org/10.1007/S10549-013-2763-Z
Borras M, Lacroix M, Legros N et al (1997) Estrogen receptor-negative/progesterone receptor-positive Evsa-T mammary tumor cells: a model for assessing the biological property of this peculiar phenotype of breast cancers. Cancer Lett 120(1):23–30. https://doi.org/10.1016/S0304-3835(97)00285-1
Rakha EA, El-Sayed ME, Green AR et al (2007) Biologic And clinical characteristics of breast cancer with single hormone receptor positive phenotype. J Clin Oncol. 25(30):4772–8. https://doi.org/10.1200/Jco.2007.12.2747
Chan M, Chang MC, Gonzalez R et al (2015) Outcomes Of estrogen receptor negative and progesterone receptor positive breast cancer. Plos One. 10(7):E0132449. https://doi.org/10.1371/Journal.Pone.0132449
Yu KD, Jiang YZ, Hao S et al (2015) Molecular essence and endocrine responsiveness of estrogen receptor-negative, progesterone receptor-positive, and her2-negative breast cancer. BMC Med 13:254. https://doi.org/10.1186/S12916-015-0496-Z
Fu J, Zhong C, Wu L et al (2019) Young patients with hormone receptor-positive breast cancer have a higher long-term risk of breast cancer specific death. J Breast Cancer 22(1):96–108. https://doi.org/10.4048/Jbc.2019.22.E13
Noone AM, Lund JL, Mariotto A et al (2016) Comparison Of seer treatment data with medicare claims. Med Care. 54(9):E55-64. https://doi.org/10.1097/Mlr.0000000000000073
Ta H, Hl W, Sg H et al (2004) Breast cancer patients with progesterone receptor Pr-A-rich tumors have poorer disease-free survival rates. Clin Cancer Res 10(8):2751–2760. https://doi.org/10.1158/1078-0432.Ccr-03-0141
Martin MB, Saceda M, Lindsey RK (1993) Regulation Of Estrogen Receptor Expression In Breast Cancer. Adv Exp Med Biol. 330:143–53. https://doi.org/10.1007/978-1-4615-2926-2_11
Sg K, Hm J, Thijssen Jh et al (1993) Wild type and alternatively spliced estrogen receptor messenger RNA in human meningioma tissue and Mcf7 breast cancer cells. J Steroid Biochem Mol Biol 45(4):227–233. https://doi.org/10.1016/0960-0760(93)90336-U
Fan Y, Ding X, Xu B et al (2015) Prognostic significance of single progesterone receptor positivity: a comparison study of estrogen receptor negative/progesterone receptor positive/her2 negative primary breast cancer with triple negative breast cancer. Medicine. 94(46):E2066. https://doi.org/10.1097/Md.0000000000002066
Perou CM, Sorlie T, Eisen MB et al (2000) Molecular portraits of human breast tumours. Nature. 406(6797):747–52. https://doi.org/10.1038/35021093
Yin D, Wang YL, Wang YF et al (2015) Correlation between clinical pathology of luminal b breast cancer and determination of estrogen receptor, progesterone receptor and her2 expression combined with nuclear morphology. J Biol Regul Homeost Agents. 29(3):579–87
Liu S, Chapman JA, Burnell MJ et al (2015) Prognostic And predictive investigation of Pam50 intrinsic subtypes in the Ncic Ctg Ma.21 phase Iii chemotherapy trial. Breast Cancer Res Treatm 149(2):439–48. https://doi.org/10.1007/S10549-014-3259-1
Prat A, Parker JS, Fan C et al (2012) Pam50 assay and the three-gene model for identifying the major and clinically relevant molecular subtypes of breast cancer. Breast Cancer Res Treatm 135(1):301–6. https://doi.org/10.1007/S10549-012-2143-0
Carey LA, Dees EC, Sawyer L et al (2007) The triple negative paradox: primary tumor chemosensitivity of breast cancer subtypes. Clin Cancer Res 13(8):2329–34. https://doi.org/10.1158/1078-0432.Ccr-06-1109
Prat A, Perou CM (2011) Deconstructing the molecular portraits of breast cancer. Mol Oncol. 5(1):5–23. https://doi.org/10.1016/J.Molonc.2010.11.003
Sorlie T, Tibshirani R, Parker J et al (2003) Repeated observation of breast tumor subtypes in independent gene expression data sets. Proc Natl Acad Sci U S A. 100(14):8418–23. https://doi.org/10.1073/Pnas.0932692100
Haibe-Kains B, Desmedt C, Loi S et al (2012) A three-gene model to robustly identify breast cancer molecular subtypes. J Natl Cancer Institute. 104(4):311–25. https://doi.org/10.1093/Jnci/Djr545
Chia SK, Bramwell VH, Tu D et al (2012) A 50-gene intrinsic subtype classifier for prognosis and prediction of benefit from adjuvant tamoxifen. Clin Cancer Res 18(16):4465–72. https://doi.org/10.1158/1078-0432.Ccr-12-0286
Sanchez-Munoz A, Plata-Fernandez Y, Fernandez M et al (2014) Tumor histological subtyping determined by hormone receptors and Her2 status defines different pathological complete response and outcome to dose-dense neoadjuvant chemotherapy in breast cancer patients. Clin Transl Oncol 16(6):548–554. https://doi.org/10.1007/S12094-013-1116-Z
Iwata H, Sato N, Masuda N et al (2011) Docetaxel followed by fluorouracil/epirubicin/cyclophosphamide as neoadjuvant chemotherapy for patients with primary breast cancer. Jpn J Clin Oncol 41(7):867–875. https://doi.org/10.1093/Jjco/Hyr081.PubmedPmid:21719750
Rouzier R, Perou CM, Symmans WF et al (2005) Breast cancer molecular subtypes respond differently to preoperative chemotherapy. Clin Cancer Res 11(16):5678–85. https://doi.org/10.1158/1078-0432.Ccr-04-2421
Bardou VJ, Arpino G, Elledge RM et al (2003) Progesterone receptor status significantly improves outcome prediction over estrogen receptor status alone for adjuvant endocrine therapy in two large breast cancer databases. J Clin Oncol. 21(10):1973–9. https://doi.org/10.1200/Jco.2003.09.099
Davies C, Godwin J, Gray R et al (2011) Relevance of breast cancer hormone receptors and other factors to the efficacy of adjuvant tamoxifen: patient-level meta-analysis of randomised trials. Lancet (London, England). 378(9793):771–84. https://doi.org/10.1016/S0140-6736(11)60993-8
Funding
The study was supported by the Grant from the major program of the Jinhua Municipal Science & Technology Bureau (Grant number 2019-3-004) and the key program of the Jinhua Municipal Science & Technology Bureau (Grant number 2014-3-008).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
All authors have declared no conflicting interests.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
About this article
Cite this article
Zheng, H., Ge, C., Lin, H. et al. Estrogen receptor-negative/progesterone receptor-positive and her-2-negative breast cancer might no longer be classified as hormone receptor-positive breast cancer. Int J Clin Oncol 27, 1145–1153 (2022). https://doi.org/10.1007/s10147-022-02158-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10147-022-02158-0