Abstract
Purpose
Previous studies have demonstrated excellent overall outcomes in patients who underwent low-dose-rate brachytherapy (LDR-BT) in intermediate-risk, localized prostate cancer (PCa). We thus investigated the appropriate length of time before completing prostate-specific antigen (PSA) monitoring after treatment.
Patients and Methods
Between 2003 and 2014, 710 localized, intermediate-risk PCa patients underwent LDR-BT with or without supplemental external beam radiotherapy (EBRT). Data from 567 of those patients was analyzed in this study. Neoadjuvant hormonal therapy (NHT) was administered to 315 patients (55.6 %) and NHT with adjuvant hormonal therapy (AHT) to 59 patients (10.4 %), as per the protocol of a prospective randomized controlled trial (SHIP0804). We stratified patients by posttreatment PSA levels at specific times and assessed the factors for association with biochemical recurrence (BCR) and for clinical progression (CP).
Results
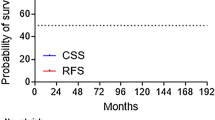
The median follow-up was 109 months (range, 60-205 months). Of 529 patients who were BCR-free at 3 years after treatment, 56 subsequently developed BCR, and 47 developed CP. PSA at 3 and 5 years after treatment were significantly correlated with long-term oncological outcomes. No patients with 5-year PSA levels ≤0.1 ng/mL subsequently developed BCR or CP.
Conclusion
Discontinuation of PSA monitoring could be discussed with patients with intermediate-risk PCa as a reasonable option if PSA levels remain ≤0.1 ng/mL at 5 years after LDR-BT, either alone or with other combined modalities, as subsequent recurrences are quite rare.



Similar content being viewed by others
Reference
Mottet, N. et al. (2021) EAU-EANM-ESTRO-ESUR-SIOG Guidelines on Prostate Cancer-2020 Update. Part 1: Screening, Diagnosis, and Local Treatment with Curative Intent. European urology 79(2), 243-262. https://doi.org/10.1016/j.eururo.2020.09.042.
Serrano, N. A. & Anscher, M. S. Favorable vs Unfavorable Intermediate-Risk Prostate Cancer: A Review of the New Classification System and Its Impact on Treatment Recommendations. Oncology (Williston Park, N.Y.) 30, 229-236 (2016).
Urabe F et al (2021) Prognostic value of PSA bounce in prostate cancer following definitive radiation therapy: a systematic review and meta-analysis. Prostate Cancer Prost Dis. https://doi.org/10.1038/s41391-021-00372-x
Skove SL et al (2017) Timing of prostate-specific antigen nadir after radical prostatectomy and risk of biochemical recurrence. Urology 108:129–134. https://doi.org/10.1016/j.urology.2017.07.009
Soyano T et al (2021) Time to achieve a prostate-specific antigen nadir of ≤0.2 ng/mL and related factors after permanent prostate brachytherapy. Brachytherapy 20(1):29–37. https://doi.org/10.1016/j.brachy.2020.07.006
Critz, F. A. et al. (1999) Post-treatment PSA < or = 0.2 ng/mL defines disease freedom after radiotherapy for prostate cancer using modern techniques. Urology. 54(6), 968-971. https://doi.org/10.1016/s0090-4295(99)00346-5
Ko, E. C., Stone, N. N. & Stock, R. G. (2012) PSA nadir of <05 ng/mL following brachytherapy for early-stage prostate adenocarcinoma is associated with freedom from prostate-specific antigen failure. International journal of radiation oncology, biology, physics 83(2), 600-607. https://doi.org/10.1016/j.ijrobp.2011.07.009.
McLaren, D. B. et al. The Importance of Prostate-specific Antigen (PSA) Nadir and Early Identification of PSA Relapse after 10 Years of Prostate Iodine 125 Seed Brachytherapy in Edinburgh. Clinical oncology (Royal College of Radiologists (Great Britain)) 27, 519-526, doi:https://doi.org/10.1016/j.clon.2015.05.003 (2015).
Mohler, J. L. et al. Prostate Cancer, Version 2.2019, NCCN Clinical Practice Guidelines in Oncology. Journal of the National Comprehensive Cancer Network : JNCCN 17, 479-505, doi:https://doi.org/10.6004/jnccn.2019.0023 (2019).
Zumsteg ZS et al (2013) A new risk classification system for therapeutic decision making with intermediate-risk prostate cancer patients undergoing dose-escalated external-beam radiation therapy. European urol 64:895–902. https://doi.org/10.1016/j.eururo.2013.03.033
Miki K et al (2010) Transperineal prostate brachytherapy, using I-125 seed with or without adjuvant androgen deprivation, in patients with intermediate-risk prostate cancer: study protocol for a phase III, multicenter, randomized, controlled trial. BMC cancer 10:572. https://doi.org/10.1186/1471-2407-10-572
Kimura T et al (2014) Mid-term outcome of permanent prostate iodine-125 brachytherapy in Japanese patients. Int J Urol: Off J Japanese Urol Assoc 21:473–478. https://doi.org/10.1111/iju.12347
Tabata R et al (2016) Do androgen deprivation and the biologically equivalent dose matter in low-dose-rate brachytherapy for intermediate-risk prostate cancer? Cancer Med 5:2314–2322. https://doi.org/10.1002/cam4.820
Stock RG, Stone NN, Cesaretti JA, Rosenstein BS (2006) Biologically effective dose values for prostate brachytherapy: effects on PSA failure and posttreatment biopsy results. Int J Radiat Oncol Biol Phys 64:527–533. https://doi.org/10.1016/j.ijrobp.2005.07.981
Roach M 3rd et al (2006) Defining biochemical failure following radiotherapy with or without hormonal therapy in men with clinically localized prostate cancer: recommendations of the RTOG-ASTRO Phoenix Consensus Conference. Intl J Rad Oncol Biol Phys 65:965–974. https://doi.org/10.1016/j.ijrobp.2006.04.029
Xiao GQ, Huan Y, Stone N, Stock R, Unger PD (2009) Histological patterns and associated PSA levels for prostatic adenocarcinoma following brachytherapy. Pathol Res Prac 205:843–846. https://doi.org/10.1016/j.prp.2009.07.009
Stock RG, Klein TJ, Cesaretti JA, Stone NN (2009) Prognostic significance of 5-year PSA value for predicting prostate cancer recurrence after brachytherapy alone and combined with hormonal therapy and/or external beam radiotherapy. Int J Rad Oncol Biol Phys 74:753–758. https://doi.org/10.1016/j.ijrobp.2008.08.049
Lo AC et al (2014) Prostate-specific antigen at 4 to 5 years after low-dose-rate prostate brachytherapy is a strong predictor of disease-free survival. Int J Rad Oncol Biol Phys 88:87–93. https://doi.org/10.1016/j.ijrobp.2013.10.010
Niwa N et al (2018) Selection of patients who would not require long-term prostate-specific antigen monitoring after low-dose-rate brachytherapy. Brachytherapy 17:899–905. https://doi.org/10.1016/j.brachy.2018.08.018
Morris, W. J., Pickles, T. & Keyes, M. Using a surgical prostate-specific antigen threshold of >0.2 ng/mL to define biochemical failure for intermediate- and high-risk prostate cancer patients treated with definitive radiation therapy in the ASCENDE-RT randomized control trial. Brachytherapy 17, 837-844, doi:https://doi.org/10.1016/j.brachy.2018.08.008 (2018).
Crook JM et al (2020) A biochemical definition of cure after brachytherapy for prostate cancer. Radiother oncol: J European Soc Therap Radiol Oncol 149:64–69. https://doi.org/10.1016/j.radonc.2020.04.038
Kimura S et al (2020) Performance of [(68)Ga] Ga-PSMA 11 PET for detecting prostate cancer in the lymph nodes before salvage lymph node dissection: a systematic review and meta-analysis. Prostate Cancer Prostatic Dis 23:1–10. https://doi.org/10.1038/s41391-019-0156-z
Raveenthiran S et al (2019) The use of (68)Ga-PET/CT PSMA to determine patterns of disease for biochemically recurrent prostate cancer following primary radiotherapy. Prostate Cancer Prostatic Dis 22:385–390. https://doi.org/10.1038/s41391-019-0163-0
Gulley JL et al (2005) A prospective analysis of the time to normalization of serum androgens following 6 months of androgen deprivation therapy in patients on a randomized phase III clinical trial using limited hormonal therapy. J urol 173:1567–1571. https://doi.org/10.1097/01.ju.0000154780.72631.85
Kaku H et al (2006) Time course of serum testosterone and luteinizing hormone levels after cessation of long-term luteinizing hormone-releasing hormone agonist treatment in patients with prostate cancer. Prostate 66:439–444. https://doi.org/10.1002/pros.20341
Acknowledgements
This study was supported in part by a grant of SHIP0804 (NCT00664456). English-language editorial support was provided by Seaman Medical, Inc., Bellingham WA, USA.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
About this article
Cite this article
Urabe, F., Kimura, T., Sasaki, H. et al. How long is long enough to secure disease control after low-dose-rate brachytherapy in combination with other modalities in intermediate-risk, localized prostate cancer?. Int J Clin Oncol 27, 184–193 (2022). https://doi.org/10.1007/s10147-021-02040-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10147-021-02040-5