Abstract
Background
To elucidate the clinicopathological features, hospital-based care volume and prognoses associated with primary retroperitoneal sarcoma (PRS).
Methods
Clinical data on PRS cases, diagnosed from 2008 to 2009 (cohort A) and from 2012 to 2015 (cohort B), were obtained from the national hospital-based cancer registry in Japan. Since data on survival, 5 years after PRS diagnosis, were available only for cohort A, patient prognoses were analyzed in this group alone.
Results
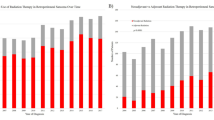
The numbers of participating hospitals were 154 in cohort A and 537 in cohort B. In total, 380 and 2011 patients with PRS were identified in cohorts A and B, respectively. The incidence of PRS among all the registered urogenital malignancies was 0.52% (2391/462,866). Liposarcoma was the most commonly observed PRS subtype (55.8%), followed by leiomyosarcoma (19.0%). In cohort A, the 5-year overall survival (OS) was 40.4%. The 5-year OS associated with stage I (n = 107), stages II and III (n = 61), and stage IV (n = 59) disease were 59%, 39%, and 6%, respectively. Only two institutions treated over ten patients per year in each cohort. When institutions were divided by hospital care volume (8 hospitals with ≥ = 3 cases and 149 with < 3 cases/year), there were any statistic differences in the OS.
Conclusions
We presented the distribution and prognoses associated with PRS using a real-world large cohort database. Centralization for PRS management was not established in Japan, while the prognosis did not significantly depend on the treatment volume of hospitals.




Similar content being viewed by others
References
Katz D, Palmerini E, Pollack SM (2018) More than 50 subtypes of soft tissue sarcoma: paving the path for histology-driven treatments. Am Soc Clin Oncol Educ Book 38:925–938
Gutierrez JC, Perez EA, Franceschi D et al (2007) Outcomes for soft-tissue sarcoma in 8249 cases from a large state cancer registry. J Surg Res 141:105–114
Russo P, Brady MS, Conlon K et al (1992) Adult urological sarcoma. J Urol 147:1032–1036
Wibmer C, Leithner A, Zielonke N et al (2010) Increasing incidence rates of soft tissue sarcomas? A population-based epidemiologic study and literature review. Ann Oncol 21:1106–1111
Ogura K, Higashi T, Kawai A (2017) Statistics of soft-tissue sarcoma in Japan: report from the bone and soft tissue tumor registry in Japan. J Orthop Sci 22:755–764
Ikoma N, Torres KE, Lin HY et al (2017) Recurrence patterns of retroperitoneal leiomyosarcoma and impact of salvage surgery. J Surg Oncol 116:313–319
Gronchi A, Lo VS, Fiore M et al (2009) Aggressive surgical policies in a retrospectively reviewed single-institution case series of retroperitoneal soft tissue sarcoma patients. J Clin Oncol 27:24–30
Dotan ZA, Tal R, Golijanin D et al (2006) Adult genitourinary sarcoma: the 25-year memorial sloan-kettering experience. J Urol 176:2033–2038
Bhangu AA, Beard JA, Grimer RJ (2004) Should soft tissue sarcomas be treated at a specialist centre? Sarcoma 8:1–6
Hoekstra HJ, Haas RLM, Verhoef C et al (2017) Adherence to guidelines for adult (non-GIST) soft tissue sarcoma in the Netherlands: a plea for dedicated sarcoma centers. Ann Surg Oncol 24:3279–3288
Trans-Atlantic RPS Working Group (2015) Management of primary retroperitoneal sarcoma (RPS) in the adult: a consensus approach from the Trans-Atlantic RPS working group. Ann Surg Oncol 22:256–263
Styring E, Billing V, Hartman L et al (2012) Simple guidelines for efficient referral of soft-tissue sarcomas: a population-based evaluation of adherence to guidelines and referral patterns. J Bone Jt Surg Am 94:1291–1296
Higashi T, Nakamura F, Shibata A et al (2014) The national database of hospital-based cancer registries: a nationwide infrastructure to support evidence-based cancer care and cancer control policy in Japan. Jpn J Clin Oncol 44:2–8
Kalaiselvan R, Malik AK, Rao R et al (2019) Impact of centralization of services on outcomes in a rare tumour: retroperitoneal sarcomas. Eur J Surg Oncol 45:249–253
Gutierrez JC, Perez EA, Moffat FL et al (2007) Should soft tissue sarcomas be treated at high-volume centers? An analysis of 4205 patients. Ann Surg 245:952–958
Inoue I, Nakamura F, Matsumoto K et al (2017) Cancer in adolescents and young adults: national incidence and characteristics in Japan. Cancer Epidemiol 51:74–80
Okuyama A, Higashi T (2018) Patterns of cancer treatment in different age groups in Japan: an analysis of hospital-based cancer registry data, 2012–2015. Jpn J Clin Oncol 48:417–425
NICE Guidance on Cancer Studies (2006) Improving outcomes for people with sarcoma national institute for health and clinical excellence, CSG9. Accessed 25 Jan 2016.
Sandrucci S, Naredi P, Bonvalot S (2019) Centers of excellence or excellence networks: the surgical challenge and quality issues in rare cancers. Eur J Surg Oncol 45:19–21
Keung EZ, Chiang YJ, Cormier JN et al (2018) Treatment at low-volume hospitals is associated with reduced short-term and long-term outcomes for patients with retroperitoneal sarcoma. Cancer 124:4495–4503
Funding
The Cancer Research and Development Fund of National Cancer Centre, Japan, supported this work.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest statement
No author has any conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
About this article
Cite this article
Kimura, T., Kawai, K., Kandori, S. et al. Impact of centralization in primary retroperitoneal sarcoma treatment: analysis using hospital-based cancer registry data in Japan. Int J Clin Oncol 25, 1687–1694 (2020). https://doi.org/10.1007/s10147-020-01709-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10147-020-01709-7