Abstract
Background
RAS/BRAF mutations of colorectal cancer (CRC) play a crucial role in carcinogenesis and cancer progression and need to be considered for the therapeutic strategy choice. We used next-generation-sequencing (NGS) technology to assess RAS/BRAF mutation differences between primary CRC and corresponding pulmonary metastases (PMs).
Methods
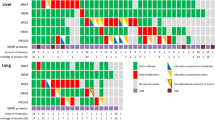
We examined the mutation statuses of the KRAS 12/13/61/146, NRAS 12/13/61/146, and BRAF 600 codons in genomic DNA from fresh-frozen or formalin-fixed paraffin-embedded tissues derived from 34 primary lesions and 52 corresponding PMs from 36 patients with CRC.
Results
We found RAS mutations in 76% (26/34) of primary CRC lesions and in 86% (31/36) of PMs. While 27% (7/26) of the primary CRC RAS mutations were heterogeneous, all the RAS mutations in PMs were homogeneous. Of the mutations in PMs, 71% (22/31) were KRAS G>A transitions, of which 82% (18/22) were KRAS G12D or G13D. The RAS mutation discordance between primary tumors and PMs was 12.1% (4/33). RAS mutations with the same genotyping were detected in all synchronous and metachronous PMs from 9 patients. We found no BRAF mutations in either primary or pulmonary tissues.
Conclusion
Our NGS analysis suggests that RAS mutations of PM of patients with CRC are more common than initially thought. The presence of KRAS mutations in CRC specimens, especially G12D or G13D mutations, seems to promote PM formation.




Similar content being viewed by others
References
Elbjeirami WM, Sughayer MA (2012) KRAS mutations and subtyping in colorectal cancer in Jordanian patients. Oncol Lett 4(4):705–710. https://doi.org/10.3892/ol.2012.785
De Roock W, Claes B, Bernasconi D et al (2010) Effects of KRAS, BRAF, NRAS, and PIK3CA mutations on the efficacy of cetuximab plus chemotherapy in chemotherapy-refractory metastatic colorectal cancer: a retrospective consortium analysis. Lancet Oncol 11(8):753–762. https://doi.org/10.1016/S1470-2045(10)70130-3
Heinemann V, von Weikersthal LF, Decker T et al (2014) FOLFIRI plus cetuximab versus FOLFIRI plus bevacizumab as first-line treatment for patients with metastatic colorectal cancer (FIRE-3): a randomised, open-label, phase 3 trial. Lancet Oncol 15(10):1065–1075. https://doi.org/10.1016/S1470-2045(14)70330-4
Renaud S, Romain B, Falcoz PE et al (2015) KRAS and BRAF mutations are prognostic biomarkers in patients undergoing lung metastasectomy of colorectal cancer. Br J Cancer 112(4):720–728. https://doi.org/10.1038/bjc.2014.499
Yoshino T, Muro K, Yamaguchi K et al (2015) Clinical validation of a multiplex kit for RAS mutations in colorectal cancer: Results of the RASKET (RAS KEy Testing) prospective, multicenter study. EBioMed 2(4):317–323. https://doi.org/10.1016/j.ebiom.2015.02.007
Gao J, Wu H, Wang L et al (2016) Validation of targeted next-generation sequencing for RAS mutation detection in FFPE colorectal cancer tissues: comparison with Sanger sequencing and ARMS-Scorpion real-time PCR. BMJ Open 6(1):e009532. https://doi.org/10.1136/bmjopen-2015-009532
Altimari A, de Biase D, De Maglio G et al (2013) 454 next generation-sequencing outperforms allele-specific PCR, Sanger sequencing, and pyrosequencing for routine KRAS mutation analysis of formalin-fixed, paraffin-embedded samples. Onco Targets Ther 6:1057–1064. https://doi.org/10.2147/OTT.S42369
Gonzalez de Castro D, Angulo B, Gomez B et al (2012) A comparison of three methods for detecting KRAS mutations in formalin-fixed colorectal cancer specimens. Br J Cancer 107(2):345–351. https://doi.org/10.1038/bjc.2012.259
Atsumi J, Hanami T, Enokida Y et al (2015) Eprobe-mediated screening system for somatic mutations in the KRAS locus. Oncol Rep 33(6):2719–2727. https://doi.org/10.3892/or.2015.3883
Ikota H, Nobusawa S, Arai H et al (2015) Evaluation of IDH1 status in diffusely infiltrating gliomas by immunohistochemistry using anti-mutant and wild type IDH1 antibodies. Brain Tumor Pathol 32(4):237–244. https://doi.org/10.1007/s10014-015-0222-8
Shahsiah R, DeKoning J, Samie S et al (2017) Validation of a next generation sequencing panel for detection of hotspot cancer mutations in a clinical laboratory. Pathol Res Pract 213(2):98–105. https://doi.org/10.1016/j.prp.2016.11.016
Yaeger R, Cowell E, Chou JF et al (2015) RAS mutations affect pattern of metastatic spread and increase propensity for brain metastasis in colorectal cancer. Cancer 121(8):1195–1203. https://doi.org/10.1002/cncr.29196
Kim MJ, Lee HS, Kim JH et al (2012) Different metastatic pattern according to the KRAS mutational status and site-specific discordance of KRAS status in patients with colorectal cancer. BMC Cancer 12:347. https://doi.org/10.1186/1471-2407-12-347
Schweiger T, Hegedus B, Nikolowsky C et al (2014) EGFR, BRAF and KRAS status in patients undergoing pulmonary metastasectomy from primary colorectal carcinoma: a prospective follow-up study. Ann Surg Oncol 21(3):946–954. https://doi.org/10.1245/s10434-013-3386-7
Renaud S, Seitlinger J, Lawati YA et al (2018) Anatomical resections improve survival following lung metastasectomy of colorectal cancer harboring KRAS mutations. Ann Surg. https://doi.org/10.1097/SLA.0000000000002829
Tie J, Lipton L, Desai J et al (2011) KRAS mutation is associated with lung metastasis in patients with curatively resected colorectal cancer. Clin Cancer Res 17(5):1122–1130. https://doi.org/10.1158/1078-0432.CCR-10-1720
Harle A, Filhine-Tresarrieu P, Husson M et al (2016) Rare RAS mutations in metastatic colorectal cancer detected during routine RAS genotyping using next generations. Target Oncol 11(3):363–370. https://doi.org/10.1007/s11523-015-0404-7
Hagemann IS, Devarakonda S, Lockwood CM et al (2015) Clinical next-generation sequencing in patients with non-small cell lung cancer. Cancer 121(4):631–639. https://doi.org/10.1002/cncr.29089
Cejas P, Lopez-Gomez M, Aguayo C et al (2009) KRAS mutations in primary colorectal cancer tumors and related metastases: a potential role in prediction of lung metastasis. PLoS ONE 4(12):e8199. https://doi.org/10.1371/journal.pone.0008199
Baldus SE, Schaefer KL, Engers R et al (2010) Prevalence and heterogeneity of KRAS, BRAF, and PIK3CA mutations in primary colorectal adenocarcinomas and their corresponding metastases. Clin Cancer Res 16(3):790–799. https://doi.org/10.1158/1078-0432.CCR-09-2446
Zou SM, Li WH, Wang WM et al (2018) The gene mutational discrepancies between primary and paired metastatic colorectal carcinoma detected by next-generation sequencing. J Cancer Res Clin Oncol. https://doi.org/10.1007/s00432-018-2742-1
Alix-Panabieres C, Pantel K (2014) Challenges in circulating tumour cell research. Nat Rev Cancer 14(9):623–631. https://doi.org/10.1038/nrc3820
Piyush T, Rhodes JM, Yu LG (2017) MUC1 O-glycosylation contributes to anoikis resistance in epithelial cancer cells. Cell Death Discov 3:17044. https://doi.org/10.1038/cddiscovery.2017.44
Wu G, Maharjan S, Kim D et al (2018) A novel monoclonal antibody targets Mucin1 and attenuates growth in pancreatic cancer model. Int J Mol Sci 19:7. https://doi.org/10.3390/ijms19072004
Hiraki M, Maeda T, Mehrotra N et al (2018) Targeting MUC1-C suppresses BCL2A1 in triple-negative breast cancer. Signal Transduct Target Ther 3:13. https://doi.org/10.1038/s41392-018-0013-x
Lan YT, Jen-Kou L, Lin CH et al (2015) Mutations in the RAS and PI3K pathways are associated with metastatic location in colorectal cancers. J Surg Oncol 111(7):905–910. https://doi.org/10.1002/jso.23895
Kadota K, Yeh YC, D'Angelo SP et al (2014) Associations between mutations and histologic patterns of mucin in lung adenocarcinoma: invasive mucinous pattern and extracellular mucin are associated with KRAS mutation. Am J Surg Pathol 38(8):1118–1127. https://doi.org/10.1097/PAS.0000000000000246
Morris VK, Lucas FA, Overman MJ et al (2014) Clinicopathologic characteristics and gene expression analyses of non-KRAS 12/13, RAS-mutated metastatic colorectal cancer. Ann Oncol 25(10):2008–2014. https://doi.org/10.1093/annonc/mdu252
Acknowledgements
We are grateful for the experimental support we received from Mr. Tatsuya Yamazaki, Mr. Masaki Shinohara, and Ms. Yuriha Iwata. We would also like to thank RIKEN GeNAS for amplicon sequencing analyses with the Illumina HiSeq2500 sequencer.
Funding
This work was supported by the Grants-in-Aid for Scientific Research from the Japan Society for the Promotion of Science; Grant numbers 22590516 and 19390359, by the subsidy of expenses of the Minister of Economy, Trade and Industry, Japan for small business support, and by a Research Grant from the Japanese Ministry of Education, Culture, Sports, Science and Technology to the RIKEN Center for Life Science Technologies.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest directly relevant to the content of this article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
About this article
Cite this article
Igarashi, T., Shimizu, K., Usui, K. et al. Significance of RAS mutations in pulmonary metastases of patients with colorectal cancer. Int J Clin Oncol 25, 641–650 (2020). https://doi.org/10.1007/s10147-019-01582-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10147-019-01582-z