Abstract
Background
Residual tumor size after primary surgery is the most important prognostic factor in advanced ovarian cancer. We conducted a retrospective study in Japanese women to evaluate the association of various residual disease diameters and histological subtypes with overall survival (OS) in patients with residual disease ≥1 cm.
Methods
Demographic and clinicopathological data were obtained from the Tokai Ovarian Tumor Study Group; 294 patients with International Federation of Gynecology and Obstetrics stage III and IV epithelial ovarian carcinoma who had undergone primary debulking surgery between 1986 and 2007 and had ≥1 cm residual tumor were identified. A Cox proportional hazards model was used to assess the association of prognostic factors with OS.
Results
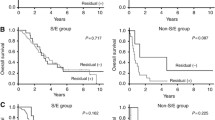
Non-serous advanced ovarian cancer was associated with a significant increase in the risk of death. For serous ovarian cancer, residual tumor size was not an independent prognostic factor [multivariate hazard ratio (HR) = 1.63, 95% confidence interval (CI) = 0.96–2.79 (2–5 cm); HR = 1.25, 95% CI = 0.72–2.17 (>5 cm); trend P = 0.480], whereas taxane-based chemotherapy was associated with a better prognosis (HR = 0.66, 95% CI = 0.44–0.99, P = 0.046). For non-serous ovarian cancer, in contrast, residual tumor size was associated with an increased risk of death [multivariate HR = 0.87, 95% CI = 0.36–2.14 (2–5 cm); HR = 2.21, 95% CI = 0.96–5.08 (>5 cm); trend P = 0.067], whereas taxane-based chemotherapy was not a prognostic factor [HR = 0.70, 95% CI = 0.29–1.65, P = 0.409 (taxane-based)].
Conclusions
Although primary maximal cytoreduction is essential to improving OS in advanced ovarian cancer, our findings suggest the management of patients with suboptimal residual tumor should take into account differences between histological subtypes.



Similar content being viewed by others
References
Tamakoshi K, Kondo T, Yatsuya H et al (2001) Trends in the mortality (1950–1997) and incidence (1975–1993) of malignant ovarian neoplasm among Japanese women: analyses by age, time, and birth cohort. Gynecol Oncol 83:64–71
Statistics and Information Department MoH, Labour and Welfare, Japan (2007) Vital Statistics. 2007 [cited; Available from: http://www.mhlw.go.jp/toukei/saikin/index.html]
Japan Society of Gynecologic Oncology (2007) Ovarian cancer treatment guidelines 2007. Kanehara & Co. Ltd, Tokyo
Network NCC (2009) Ovarian Cancer Guideline (V.2.2009). 2009 [cited 2009 August, 7]; Available from: http://www.nccn.org/professionals/physician_gls/PDF/ovarian.pdf
Covens AL (2000) A critique of surgical cytoreduction in advanced ovarian cancer. Gynecol Oncol 78:269–274
Dauplat J, Le Bouedec G, Pomel C et al (2000) Cytoreductive surgery for advanced stages of ovarian cancer. Semin Surg Oncol 19:42–48
Curtin JP, Malik R, Venkatraman ES et al (1997) Stage IV ovarian cancer: impact of surgical debulking. Gynecol Oncol 64:9–12
Akahira JI, Yoshikawa H, Shimizu Y et al (2001) Prognostic factors of stage IV epithelial ovarian cancer: a multicenter retrospective study. Gynecol Oncol 81:398–403
Chi DS, Liao JB, Leon LF et al (2001) Identification of prognostic factors in advanced epithelial ovarian carcinoma. Gynecol Oncol 82:532–537
Winter WE III, Maxwell GL, Tian C et al (2007) Prognostic factors for stage III epithelial ovarian cancer: a Gynecologic Oncology Group Study. J Clin Oncol 25:3621–3627
Omura GA, Brady MF, Homesley HD et al (1991) Long-term follow-up and prognostic factor analysis in advanced ovarian carcinoma: the Gynecologic Oncology Group experience. J Clin Oncol 9:1138–1150
Makar AP, Baekelandt M, Trope CG et al (1995) The prognostic significance of residual disease, FIGO substage, tumor histology, and grade in patients with FIGO stage III ovarian cancer. Gynecol Oncol 56:175–180
Brun JL, Feyler A, Chene G et al (2000) Long-term results and prognostic factors in patients with epithelial ovarian cancer. Gynecol Oncol 78:21–27
Winter WE 3rd, Maxwell GL, Tian C et al (2008) Tumor residual after surgical cytoreduction in prediction of clinical outcome in stage IV epithelial ovarian cancer: a Gynecologic Oncology Group Study. J Clin Oncol 26:83–89
Bristow RE, Montz FJ, Lagasse LD et al (1999) Survival impact of surgical cytoreduction in stage IV epithelial ovarian cancer. Gynecol Oncol 72:278–287
Hoskins WJ, McGuire WP, Brady MF et al (1994) The effect of diameter of largest residual disease on survival after primary cytoreductive surgery in patients with suboptimal residual epithelial ovarian carcinoma. Am J Obstet Gynecol 170:974–979 discussion 9-80
Hess V, A’Hern R, Nasiri N et al (2004) Mucinous epithelial ovarian cancer: a separate entity requiring specific treatment. J Clin Oncol 22:1040–1044
Pectasides D, Fountzilas G, Aravantinos G et al (2006) Advanced stage clear-cell epithelial ovarian cancer: the Hellenic Cooperative Oncology Group experience. Gynecol Oncol 102:285–291
Shimada M, Kigawa J, Ohishi Y et al (2009) Clinicopathological characteristics of mucinous adenocarcinoma of the ovary. Gynecol Oncol 113:331–334
Wimberger P, Lehmann N, Kimmig R et al (2006) Impact of age on outcome in patients with advanced ovarian cancer treated within a prospectively randomized phase III study of the Arbeitsgemeinschaft Gynaekologische Onkologie Ovarian Cancer Study Group (AGO-OVAR). Gynecol Oncol 100:300–307
Prefontaine M, Gelfand AT, Donovan JT et al (1994) Reproducibility of tumor measurements in ovarian cancer: a study of interobserver variability. Gynecol Oncol 55:87–90
Acknowledgments
The authors are grateful to the staff of the Department of Obstetrics and Gynecology, Nagoya University Hospital and affiliated hospitals. We are also grateful to Dr. Keitaro Matsuo, Dr. Hideo Tanaka, and colleagues of the Division of Epidemiology and Prevention, Aichi Cancer Center Research Institute, for their support with statistical analysis.
Conflict of interest
The authors declare that they have no conflicts of interest to disclose.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Hosono, S., Kajiyama, H., Mizuno, K. et al. Comparison between serous and non-serous ovarian cancer as a prognostic factor in advanced epithelial ovarian carcinoma after primary debulking surgery. Int J Clin Oncol 16, 524–532 (2011). https://doi.org/10.1007/s10147-011-0223-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10147-011-0223-5