Abstract
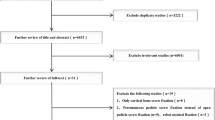
Lateral mass screw (LMS) fixation for the treatment of subaxial cervical spine instability or deformity has been traditionally associated with few neurovascular complications. However, cervical pedicle screw (CPS) fixation has recently increased in popularity, especially with navigation assistance, because of the higher pullout strength of the pedicle screws. To their knowledge, the authors conducted the first meta-analysis comparing the complication rates during and/or after CPS and LMS placement for different pathologies causing cervical spine instability. A systematic literature search of PubMed and Embase from inception to January 12, 2021 was performed to identify studies reporting CPS and/or LMS-related complications. Complications were categorized into intraoperative and early postoperative (within 30 days of surgery) and late postoperative (after 30 days from surgery) complications. All studies that met the prespecified inclusion criteria were pooled and cumulatively analyzed. A total of 24 studies were conducted during the time frame of the search and comprising 1768 participants and 8636 subaxially placed screws met the inclusion criteria. The CPS group experienced significantly more postoperative C5 palsy (odds ratio [OR] = 3.48, 95% confidence interval [CI] = 1.27–9.53, p < 0.05). Otherwise, there were no significant differences between the LMS and CPS groups. There were no significant differences between the CPS and LMS groups in terms of neurovascular procedure-related complications other than significantly more C5 palsy in the CPS group.


Similar content being viewed by others
Data availability
The results of this study are available upon request.
Code availability
The code of this study is available upon request.
References
Yoshihara H, Passias PG, Errico TJ (2013) Screw-related complications in the subaxial cervical spine with the use of lateral mass versus cervical pedicle screws: a systematic review. J Neurosurg Spine 19:614–623. https://doi.org/10.3171/2013.8.Spine13136
Hey HWD, Zhuo WH, Tan YHJ, Tan JH (2020) Accuracy of freehand pedicle screws versus lateral mass screws in the subaxial cervical spine. Spine Deform 8:1049–1058. https://doi.org/10.1007/s43390-020-00119-z
Roy-Camille R, Saillant G, Laville C, Benazet JP (1992) Treatment of lower cervical spinal injuries—C3 to C7. Spine (Phila Pa 1976) 17:S442-446. https://doi.org/10.1097/00007632-199210001-00017
Ishikawa Y, Kanemura T, Yoshida G, Ito Z, Muramoto A, Ohno S (2010) Clinical accuracy of three-dimensional fluoroscopy-based computer-assisted cervical pedicle screw placement: a retrospective comparative study of conventional versus computer-assisted cervical pedicle screw placement. J Neurosurg Spine 13:606–611. https://doi.org/10.3171/2010.5.Spine09993
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, Clarke M, Devereaux PJ, Kleijnen J, Moher D (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med 6:e1000100. https://doi.org/10.1371/journal.pmed.1000100
Downs SH, Black N (1998) The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. J Epidemiol Community Health 52:377–384. https://doi.org/10.1136/jech.52.6.377
Hooper P, Jutai JW, Strong G, Russell-Minda E (2008) Age-related macular degeneration and low-vision rehabilitation: a systematic review. Can J Ophthalmol 43:180–187. https://doi.org/10.3129/i08-001
Deeks JJ, Higgins JP, Altman DG, Group on behalf of the CSM (2019) Analysing data and undertaking meta analyses. In: Cochrane Handbook for Systematic Reviews of Interventions. John Wiley & Sons, Ltd, pp 241–284
Higgins JP, Thompson SG, Deeks JJ, Altman DG (2003) Measuring inconsistency in meta-analyses. BMJ 327:557–560. https://doi.org/10.1136/bmj.327.7414.557
DerSimonian R, Laird N (2015) Meta-analysis in clinical trials revisited. Contemp Clin Trials 45:139–145. https://doi.org/10.1016/j.cct.2015.09.002
Börm W, König RW, Hübner F, Richter HP (2003) First clinical experiences with a new cervical fixation device — technical report. Zentralbl Neurochir 64:123–127. https://doi.org/10.1055/s-2003-41883
Du W, Zhang P, Shen Y, Zhang YZ, Ding WY, Ren LX (2014) Enlarged laminectomy and lateral mass screw fixation for multilevel cervical degenerative myelopathy associated with kyphosis. Spine J 14:57–64. https://doi.org/10.1016/j.spinee.2013.06.017
El-Ghandour NMF, Soliman MAR, Ezzat AAM, Mohsen A, Zein-Elabedin M (2020) The safety and efficacy of anterior versus posterior decompression surgery in degenerative cervical myelopathy: a prospective randomized trial. J Neurosurg Spine:1–9. https://doi.org/10.3171/2020.2.Spine191272
Elmallawany M, Kandel H, Soliman MAR, Tareef TA, Atallah A, Elsaid A, Elmahdy W (2020) The safety and efficacy of cervical laminectomy and fusion versus cervical laminoplasty surgery in degenerative cervical myelopathy: a prospective randomized trial. Open Access Maced J Med Sci 8:807–814. https://doi.org/10.3889/oamjms.2020.4841
Fehlings MG, Cooper PR, Errico TJ (1994) Posterior plates in the management of cervical instability: long-term results in 44 patients. J Neurosurg 81:341–349. https://doi.org/10.3171/jns.1994.81.3.0341
Inoue S, Moriyama T, Tachibana T, Okada F, Maruo K, Horinouchi Y, Yoshiya S (2014) Risk factors for intraoperative lateral mass fracture of lateral mass screw fixation in the subaxial cervical spine. J Neurosurg Spine 20:11–17. https://doi.org/10.3171/2013.9.Spine121055
Katonis P, Papadakis SA, Galanakos S, Paskou D, Bano A, Sapkas G, Hadjipavlou AG (2011) Lateral mass screw complications: analysis of 1662 screws. J Spinal Disord Tech 24:415–420. https://doi.org/10.1097/BSD.0b013e3182024c06
Kim HS, Suk KS, Moon SH, Lee HM, Kang KC, Lee SH, Kim JS (2015) Safety evaluation of freehand lateral mass screw fixation in the subaxial cervical spine: evaluation of 1256 screws. Spine (Phila Pa 1976) 40:2–5. https://doi.org/10.1097/brs.0000000000000667
Liu K, Shi J, Jia L, Yuan W (2013) Surgical technique: hemilaminectomy and unilateral lateral mass fixation for cervical ossification of the posterior longitudinal ligament. Clin Orthop Relat Res 471:2219–2224. https://doi.org/10.1007/s11999-013-2889-7
Pateder DB, Carbone JJ (2006) Lateral mass screw fixation for cervical spine trauma: associated complications and efficacy in maintaining alignment. Spine J 6:40–43. https://doi.org/10.1016/j.spinee.2005.04.010
Sekhon LH (2005) Posterior cervical lateral mass screw fixation: analysis of 1026 consecutive screws in 143 patients. J Spinal Disord Tech 18:297–303. https://doi.org/10.1097/01.bsd.0000166640.23448.09
Su N, Fei Q, Wang BQ, Kang N, Zhang QM, Tang HH, Li D, Li JJ, Yang Y (2019) Comparison of clinical outcomes of expansive open-door laminoplasty with unilateral or bilateral fixation and fusion for treating cervical spondylotic myelopathy: a multi-center prospective study. BMC Surg 19:116. https://doi.org/10.1186/s12893-019-0583-8
Wilson B, Curtis E, Hirshman B, Oygar A, Chen K, Gabel BC, Vaida F, Allison DW, Ciacci JD (2017) Lateral mass screw stimulation thresholds in posterior cervical instrumentation surgery: a predictor of medial deviation. J Neurosurg Spine 26:346–352. https://doi.org/10.3171/2016.8.Spine16580
Zhang D, Gao X, Jiang J, Kong F, Shen Y, Ding W, Hao X, Cui H (2017) Safe placement of lateral mass screw in the subaxial cervical spine: a case series. Int Orthop 41:781–788. https://doi.org/10.1007/s00264-017-3423-4
He F, He B, Zhang CQ, Wang B, Huang H, Zhao XL (2009) Multi-slice spiral CT 3-dimensional reconstruction technique to treat multi-segmental degenerative spinal stenosis with traumatic instability of lower cervical spine. Chin J Traumatol 12:22–30
Kaneyama S, Sugawara T, Sumi M (2015) Safe and accurate midcervical pedicle screw insertion procedure with the patient-specific screw guide template system. Spine (Phila Pa 1976) 40:E341-348. https://doi.org/10.1097/brs.0000000000000772
Kim HB, Lee MK, Lee YS, Sohn JY, Jung SK, Park JH (2017) An assessment of the medial angle of inserted subaxial cervical pedicle screw during surgery: practical use of preoperative CT scanning and intraoperative X-rays. Neurol Med Chir (Tokyo) 57:159–165. https://doi.org/10.2176/nmc.oa.2016-0161
Lee S, Seo J, Lee MK, Jeon SR, Roh SW, Rhim SC, Park JH (2017) Widening of the safe trajectory range during subaxial cervical pedicle screw placement: advantages of a curved pedicle probe and laterally located starting point without creating a funnel-shaped hole. J Neurosurg Spine 27:150–157. https://doi.org/10.3171/2016.12.Spine16738
Liu Y, Hu JH, Yu KY (2009) Pedicle screw fixation for cervical spine instability: clinical efficacy and safety analysis. Chin Med J (Engl) 122:1985–1989
Mahesh B, Upendra B, Vijay S, Arun K, Srinivasa R (2017) Perforations and angulations of 324 cervical medial cortical pedicle screws: a possible guide to avoid lateral perforations with use of pedicle screws in lower cervical spine. Spine J 17:457–465. https://doi.org/10.1016/j.spinee.2016.11.011
Park JH, Jeon SR, Roh SW, Kim JH, Rhim SC (2014) The safety and accuracy of freehand pedicle screw placement in the subaxial cervical spine: a series of 45 consecutive patients. Spine (Phila Pa 1976) 39:280–285. https://doi.org/10.1097/brs.0000000000000133
Wang Y, Xie J, Yang Z, Zhao Z, Zhang Y, Li T, Liu L (2013) Computed tomography assessment of lateral pedicle wall perforation by free-hand subaxial cervical pedicle screw placement. Arch Orthop Trauma Surg 133:901–909. https://doi.org/10.1007/s00402-013-1752-3
Zhang HL, Zhou DS, Jiang ZS (2011) Analysis of accuracy of computer-assisted navigation in cervical pedicle screw installation. Orthop Surg 3:52–56. https://doi.org/10.1111/j.1757-7861.2010.00110.x
Papanastassiou I, Anderson R, Barber N, Conover C, Castellvi AE (2011) Effects of preoperative education on spinal surgery patients. SAS J 5:120–124. https://doi.org/10.1016/j.esas.2011.06.003
Nakashima H, Imagama S, Yukawa Y, Kanemura T, Kamiya M, Yanase M, Ito K, Machino M, Yoshida G, Ishikawa Y, Matsuyama Y, Hamajima N, Ishiguro N, Kato F (2012) Multivariate analysis of C-5 palsy incidence after cervical posterior fusion with instrumentation. J Neurosurg Spine 17:103–110. https://doi.org/10.3171/2012.4.Spine11255
Houten JK, Buksbaum JR, Collins MJ (2020) Patterns of neurological deficits and recovery of postoperative C5 nerve palsy. J Neurosurg Spine:1–9. https://doi.org/10.3171/2020.5.Spine20514
Badiee RK, Mayer R, Pennicooke B, Chou D, Mummaneni PV, Tan LA (2020) Complications following posterior cervical decompression and fusion: a review of incidence, risk factors, and prevention strategies. J Spine Surg 6:323–333. https://doi.org/10.21037/jss.2019.11.01
Chen Y, Chen D, Wang X, Guo Y, He Z (2007) C5 palsy after laminectomy and posterior cervical fixation for ossification of posterior longitudinal ligament. J Spinal Disord Tech 20:533–535. https://doi.org/10.1097/BSD.0b013e318042b655
Acknowledgements
The authors thank Junyu Nie MA for statistical assistance, Paul H. Dressel BFA for formatting the figures, and Debra J. Zimmer for editorial assistance.
Author information
Authors and Affiliations
Contributions
Conception and design: Mullin, Soliman
Acquisition of data: All authors
Interpretation of data: Soliman
Drafting the manuscript: Soliman
Critically revising the manuscript: All authors
Reviewed submitted version of manuscript: All authors
Statistical analysis: Khan, Salem
Study supervision: Mullin
Corresponding author
Ethics declarations
Ethics approval and consent to participate
At the time of hospital admission, informed consent for patient information to be published was provided by each patient or a legally authorized representative. No individual patient data were collected, so patient consent was not required.
Consent for publication
No individual patient data were collected, so patient consent was not required.
Conflict of interest
Dr. Khan received a research grant from the Scoliosis Research Society to study scoliosis in Chiari patients.
Dr. Mullin is involved with clinical research for Cerapedics. He receives research funding from AOSpine North America (AOSNA) and the Research Committee Award #87639; and from Medtronic External Research Program Health Professionals, ERP ID#2020-12271
Dr. Pollina is involved with surgical training for Medtronic, serves as a consultant for and receives royalties from ATEC Spine, and owns stock in Fusion Robotics.
All other authors have no personal, financial, or institutional interest in the materials or devices described in this manuscript.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Soliman, M.A.R., Khan, S., Ruggiero, N. et al. Complications associated with subaxial placement of pedicle screws versus lateral mass screws in the cervical spine: systematic review and meta-analysis comprising 1768 patients and 8636 screws. Neurosurg Rev 45, 1941–1950 (2022). https://doi.org/10.1007/s10143-022-01750-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10143-022-01750-2