Abstract
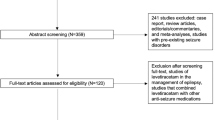
The use of prophylactic anticonvulsants among patients with subarachnoid hemorrhage (SAH) is controversial. We sought to assess the effectiveness of different durations of prophylactic antiepileptic drug (AED) use among SAH patients. We searched the MEDLINE, Embase, Cochrane, and ClinicalTrials.gov databases until March 1, 2020. Randomized controlled trials or observational studies comparing different durations or different drugs were selected. The primary outcome was poor clinical outcomes. The secondary outcome was in-hospital seizure. Bayesian network meta-analysis was also performed to indirectly compare the effectiveness of different prophylaxes. A total of 5 papers were included. Three studies with a total of 959 patients were included in the analysis of the primary outcome; the results showed that long-term exposure to prophylactic AEDs (more than 3 days) led to poor clinical outcomes (OR 1.55; 95% CI 1.01–2.39; p = 0.045). Four studies with 1024 patients were included in the analysis of the secondary outcome; the results showed no association between the duration of prophylactic AED use and the occurrence of in-hospital seizures (OR 0.62; 95% CI 0.18–2.15; p = 0.447). In the network meta-analysis, no significant difference was found among the four different prophylaxes. Our findings suggested that, when compared with the short-term use, the long-term use of prophylactic AEDs in SAH patients has a similar effect on in-hospital seizure prevention but is associated with poor clinical outcomes. However, these findings were based on a small number of available studies with obvious heterogeneity in study design and different prescription regimens. Further well-designed studies are warranted to elucidate these questions.








Similar content being viewed by others
Data availability
All data is available online.
References
Connolly ES Jr, Rabinstein AA, Carhuapoma JR, Derdeyn CP, Dion J, Higashida RT, Hoh BL, Kirkness CJ, Naidech AM, Ogilvy CS, Patel AB, Thompson BG, Vespa P (2012) Guidelines for the management of aneurysmal subarachnoid hemorrhage: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 43:1711–1737. https://doi.org/10.1161/STR.0b013e3182587839
Huttunen J, Lindgren A, Kurki MI, Huttunen T, Frösen J, Koivisto T, von Und Zu Fraunberg M, Immonen A, Jääskeläinen JE, Kälviäinen R (2017) Epilepsy-associated long-term mortality after aneurysmal subarachnoid hemorrhage. Neurology 89:263–268. https://doi.org/10.1212/wnl.0000000000004113
Panczykowski D, Pease M, Zhao Y, Weiner G, Ares W, Crago E, Jankowitz B, Ducruet AF (2016) Prophylactic antiepileptics and seizure incidence following subarachnoid hemorrhage: a propensity score-matched analysis. Stroke 47:1754–1760. https://doi.org/10.1161/strokeaha.116.013766
Naidech AM, Kreiter KT, Janjua N, Ostapkovich N, Parra A, Commichau C, Connolly ES, Mayer SA, Fitzsimmons BF (2005) Phenytoin exposure is associated with functional and cognitive disability after subarachnoid hemorrhage. Stroke 36:583–587. https://doi.org/10.1161/01.STR.0000141936.36596.1e
Moher D, Liberati A, Tetzlaff J, Altman DG (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ (Clinical research ed) 339:b2535. https://doi.org/10.1136/bmj.b2535
Higgins JP, Thompson SG (2002) Quantifying heterogeneity in a meta-analysis. Stat Med 21:1539–1558. https://doi.org/10.1002/sim.1186
Chumnanvej S, Dunn IF, Kim DH (2007) Three-day phenytoin prophylaxis is adequate after subarachnoid hemorrhage. Neurosurgery 60:99–102; discussion 102-103. https://doi.org/10.1227/01.Neu.0000249207.66225.D9
Human T, Diringer MN, Allen M, Zipfel GJ, Chicoine M, Dacey R, Dhar R (2018) A randomized trial of brief versus extended seizure prophylaxis after aneurysmal subarachnoid hemorrhage. Neurocrit Care 28:169–174. https://doi.org/10.1007/s12028-017-0440-5
Murphy-Human T, Welch E, Zipfel G, Diringer MN, Dhar R (2011) Comparison of short-duration levetiracetam with extended-course phenytoin for seizure prophylaxis after subarachnoid hemorrhage. World neurosurgery 75:269–274. https://doi.org/10.1016/j.wneu.2010.09.002
Karamchandani RR, Fletcher JJ, Pandey AS, Rajajee V (2014) Incidence of delayed seizures, delayed cerebral ischemia and poor outcome with the use of levetiracetam versus phenytoin after aneurysmal subarachnoid hemorrhage. Journal of clinical neuroscience : official journal of the Neurosurgical Society of Australasia 21:1507–1513. https://doi.org/10.1016/j.jocn.2014.03.009
Kodankandath TV, Farooq S, Wazni W, Cox JA, Southwood C, Rozansky G, Johnson V, Lynch JR (2017) Seizure prophylaxis in the immediate post-hemorrhagic period in patients with aneurysmal subarachnoid hemorrhage. Journal of vascular and interventional neurology 9:1–4
Zafar SF, Postma EN, Biswal S, Boyle EJ, Bechek S, O'Connor K, Shenoy A, Kim J, Shafi MS, Patel AB, Rosenthal ES, Westover MB (2018) Effect of epileptiform abnormality burden on neurologic outcome and antiepileptic drug management after subarachnoid hemorrhage. Clinical neurophysiology : official journal of the International Federation of Clinical Neurophysiology 129:2219–2227. https://doi.org/10.1016/j.clinph.2018.08.015
Marigold R, Günther A, Tiwari D, Kwan J (2013) Antiepileptic drugs for the primary and secondary prevention of seizures after subarachnoid haemorrhage. The Cochrane database of systematic reviews 2013:Cd008710. doi:https://doi.org/10.1002/14651858.CD008710.pub2
Rosengart AJ, Huo JD, Tolentino J, Novakovic RL, Frank JI, Goldenberg FD, Macdonald RL (2007) Outcome in patients with subarachnoid hemorrhage treated with antiepileptic drugs. J Neurosurg 107:253–260. https://doi.org/10.3171/jns-07/08/0253
Shah D, Husain AM (2009) Utility of levetiracetam in patients with subarachnoid hemorrhage. Seizure 18:676–679. https://doi.org/10.1016/j.seizure.2009.09.003
Barker-Haliski ML, Löscher W, White HS, Galanopoulou AS (2017) Neuroinflammation in epileptogenesis: insights and translational perspectives from new models of epilepsy. Epilepsia 58(Suppl 3):39–47. https://doi.org/10.1111/epi.13785
Yoon SJ, Joo JY, Kim YB, Hong CK, Chung J (2015) Effects of prophylactic antiepileptic drugs on clinical outcomes in patients with a good clinical grade suffering from aneurysmal subarachnoid hemorrhage. Journal of cerebrovascular and endovascular neurosurgery 17:166–172. https://doi.org/10.7461/jcen.2015.17.3.166
Byrne JV, Boardman P, Ioannidis I, Adcock J, Traill Z (2003) Seizures after aneurysmal subarachnoid hemorrhage treated with coil embolization. Neurosurgery 52:545–552. https://doi.org/10.1227/01.neu.0000047672.25068.4a
Huttunen J, Kurki MI, von Und Zu Fraunberg M, Koivisto T, Ronkainen A, Rinne J, Jääskeläinen JE, Kälviäinen R, Immonen A (2015) Epilepsy after aneurysmal subarachnoid hemorrhage: a population-based, long-term follow-up study. Neurology 84:2229–2237. https://doi.org/10.1212/wnl.0000000000001643
Olafsson E, Gudmundsson G, Hauser WA (2000) Risk of epilepsy in long-term survivors of surgery for aneurysmal subarachnoid hemorrhage: a population-based study in Iceland. Epilepsia 41:1201–1205. https://doi.org/10.1111/j.1528-1157.2000.tb00326.x
Code availability
Not applicable.
Author information
Authors and Affiliations
Contributions
Dr. Hu was the guarantor of the review.
Project design: Chen, Xia, and Hu; data collection: Chen, Xia, and Cai; manuscript drafting: Chen, Xia, and Cai; statistical analysis: Chen, Xia, and Cai; manuscript revision: Chen, Xia, Cai, Li, Ma, Hu, and You; supervision: Chen, Hu, and You
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Ethics approval
Not required.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Chen, Y., Xia, F., Cai, C. et al. Duration and choices of prophylactic anticonvulsants in subarachnoid hemorrhage: a systematic review and meta-analysis. Neurosurg Rev 44, 2459–2467 (2021). https://doi.org/10.1007/s10143-020-01466-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10143-020-01466-1