Abstract
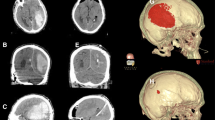
Stereotactic removal of intracerebral hematoma is a routine procedure for treating hypertensive intracerebral hemorrhage, but the complex sequence of operations limits its adoption. We explored the application of a novel surgical technique for the removal of spontaneous intracerebral hematomas. The surgical technique based on computed tomography (CT) images was used in hematoma projection and surgical planning. Markers placed on the scalp based on an Android smartphone app allowed the installation of a stereotactic head frame to facilitate the selection of the best trajectory to the hematoma center for removing the hematoma. Forty-two patients with spontaneous intracerebral hemorrhage were included in the study, including 33 cases of supratentorial hemorrhage, 5 cases of cerebellum hemorrhage, and 4 cases of brain stem hemorrhage. The surgical technique combined with the stereotactic head frame helped the tip of the drainage tube achieve the desired position. The median surgical time was 45 (range 25–75) min. The actual head frame operating time was 10 (range 5–15) min. Target alignment performed by the surgical technique was accurate to ≤ 10.0 mm in all 42 cases. No patient experienced postoperative rebleeding. In 33 cases of supratentorial intracerebral hemorrhage, an average evacuation rate of 77.5% was achieved at postoperative 3.1 ± 1.4 days, and 29 (87.9%) cases had a residual hematoma of < 15 ml. The novel surgical technique helped to quickly and effortlessly localize hematomas and achieve satisfactory hematoma removal. Clinical application of the stereotactic head frame was feasible for intracerebral hemorrhage in various locations.






Similar content being viewed by others
References
Backlund EO, von Holst H (1978) Controlled subtotal evacuation of intracerebral haematomas by stereotactic technique. Surg Neurol 9:99–101
Brown RA, Roberts TS, Osborn AG (1979) A stereotactic head frame for use with CT body scanners. Investig Radiol 14:300–304
Brown RA, Roberts TS, Osborn AG (1980) Stereotaxic frame and computer software for CT-directed neurosurgical localization. Investig Radiol 15:308–312
Cho DY, Chen CC, Chang CS, Lee WY, Melain T (2006) Endoscopic surgery for spontaneous basal ganglia hemorrhage: comparing endoscopic surgery, stereotactic aspiration, and craniotomy in noncomatose patients. Surg Neurol 65:547–555 discussion 555-546
Eftekhar B (2016) App-assisted external ventricular drain insertion. J Neurosurg 125:754–758
Fam MD, Hanley D, Stadnik A, Zeineddine HA, Girard R, Jesselson M, Cao Y, Money L, McBee N, Bistran-Hall AJ, Mould WA, Lane K, Camarata PJ, Zuccarello M, Awad IA (2017) Surgical performance in minimally invasive surgery plus recombinant tissue plasminogen activator for intracerebral hemorrhage evacuation phase III clinical trial. Neurosurgery 81:860–866
Fiorella D, Arthur A, Bain M, Mocco J (2016) Minimally invasive surgery for intracerebral hemorrhage: rationale, review of existing data and emerging technologies. Stroke 18:34
Fried HI, Nathan BR, Rowe AS, Zabramski JM, Andaluz N, Bhimraj A, Guanci MM, Seder DB, Singh JM (2016) The insertion and management of external ventricular drains: an evidence-based consensus statement : a statement for healthcare professionals from the Neurocritical Care Society. Neurocrit Care 24:61–81
Catherine OJ, Minh N, Gregory AR, Emma N, Tahiya A, Degu A, Foad A, et al. GBD 2016 Stroke Collaborators (2019) Global, regional, and national burden of stroke, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016. The Lancet Neurology 18:439–458
Hanley DF, Thompson RE, Muschelli J, Rosenblum M, McBee N, Lane K, Bistran-Hall AJ, Mayo SW, Keyl P, Gandhi D, Morgan TC, Ullman N, Mould WA, Carhuapoma JR, Kase C, Ziai W, Thompson CB, Yenokyan G, Huang E, Broaddus WC, Graham RS, Aldrich EF, Dodd R, Wijman C, Caron JL, Huang J, Camarata P, Mendelow AD, Gregson B, Janis S, Vespa P, Martin N, Awad I, Zuccarello M (2016) Safety and efficacy of minimally invasive surgery plus alteplase in intracerebral haemorrhage evacuation (MISTIE): a randomised, controlled, open-label, phase 2 trial. Lancet Neurol 15:1228–1237
Hanley DF, Thompson RE, Rosenblum M, Yenokyan G, Lane K, McBee N, Mayo Steven W, Bistran-Hall AJ, Gandhi D, Mould WA, Ullman N, Ali H, Carhuapoma JR, Kase CS, Lees KR, Dawson J, Wilson A, Betz JF, Sugar EA, Hao Y, Avadhani R, Caron JL, Harrigan MR, Carlson AP, Bulters D, LeDoux D, Huang J, Cobb C, Gupta G, Kitagawa R, Chicoine MR, Patel H, Dodd R, Camarata PJ, Wolfe S, Stadnik A, Money PL, Mitchell P, Sarabia R, Harnof S, Barzo P, Unterberg A, Teitelbaum JS, Wang W, Anderson CS, Mendelow AD, Gregson B, Janis S, Vespa P, Ziai W, Zuccarello M, Awad IA (2019) Efficacy and safety of minimally invasive surgery with thrombolysis in intracerebral haemorrhage evacuation (MISTIE III): a randomised, controlled, open-label, blinded endpoint phase 3 trial. Lancet 393:1021–1032
Hemphill JC, Greenberg SM, Anderson CS, Becker K, Bendok BR, Cushman M, Fung GL, Goldstein JN, Macdonald RL, Mitchell PH, Scott PA, Selim MH, Woo D, American Heart Association Stroke Council, Council on Cardiovascular, Stroke Nursing, Council on Clinical Cardiology (2015) Guidelines for the management of spontaneous intracerebral hemorrhage: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 46:2032–2060. https://doi.org/10.1161/STR.0000000000000069
Hinson HE, Melnychuk E, Muschelli J, Hanley DF, Awad IA, Ziai WC (2012) Drainage efficiency with dual versus single catheters in severe intraventricular hemorrhage. Neurocrit Care 16:399–405
Kothari RU, Brott T, Broderick JP, Barsan WG, Sauerbeck LR, Zuccarello M, Khoury J (1996) The ABCs of measuring intracerebral hemorrhage volumes. Stroke 27:1304–1305
Krishnamurthi RV, Feigin V, Forouzanfar MH, Mensah GA, Connor M, Bennett DA, Moran AE, Sacco RL, Anderson LM, Truelsen T, O'Donnell M, Venketasubramanian N, Barker-Collo S, Lawes CM, Wang W, Shinohara Y, Witt E, Ezzati M, Naghavi M, Murray C (2013) Global and regional burden of first-ever ischaemic and haemorrhagic stroke during 1990-2010: findings from the Global Burden of Disease Study 2010. Lancet Global Health 1:e259–e281
Kwoh YS, Hou J, Jonckheere EA, Hayati S (1988) A robot with improved absolute positioning accuracy for CT guided stereotactic brain surgery. IEEE Trans Biomed Eng 35:153
Li Y, Yang R, Li Z, Tian B, Zhang X, Wang J, Zheng L, Wang B, Li L (2017) Urokinase vs tissue-type plasminogen activator for thrombolytic evacuation of spontaneous intracerebral hemorrhage in basal ganglia. Front Neurol 8:371
Maciunas RJ,Galloway RL, Latimer JW (1994) The application accuracy of stereotactic frames. Neurosurgery 35:682–694
Mendelow AD, Gregson BA, Rowan EN, Murray GD, Gholkar A, Mitchell PM (2013) Early surgery versus initial conservative treatment in patients with spontaneous supratentorial lobar intracerebral haematomas (STICH II): a randomised trial. Lancet 382:397–408
Roberts DW, Strohbehn JW, Hatch JF, Murray W, Kettenberger H (1986) A frameless stereotaxic integration of computerized tomographic imaging and the operating microscope. J Neurosurg 65:545–549
Scaggiante J, Zhang X, Mocco J, Kellner CP (2018) Minimally invasive surgery for intracerebral hemorrhage. Stroke 49:2612–2620
Spicer MA, Apuzzo ML (2003) Virtual reality surgery: neurosurgery and the contemporary landscape. Neurosurgery 52:489–497 discussion 496-487
Thiex R, Rohde V, Rohde I, Mayfrank L, Zeki Z, Thron A, Gilsbach JM, Uhl E (2004) Frame-based and frameless stereotactic hematoma puncture and subsequent fibrinolytic therapy for the treatment of spontaneous intracerebral hemorrhage. J Neurol 251:1443–1450
Wang Wen-Zhi, Jiang B, Hong-Mei L, Di L, Lu C-Z, Ya-Du Z, Sander JW (2009) Minimally invasive craniopuncture therapy vs. conservative treatment for spontaneous intracerebral hemorrhage: results from a randomized clinical trial in China. Int J Stroke 4:11–16
Zhou H, Zhang Y, Liu L, Huang Y, Tang Y, Su J, Hua W, Han X, Xue J, Dong Q (2011) Minimally invasive stereotactic puncture and thrombolysis therapy improves long-term outcome after acute intracerebral hemorrhage. J Neurol 258:661–669
Zhou M, Wang H, Zeng X, Yin P, Zhu J, Chen W, Li X, Wang L, Wang L, Liu Y, Liu J, Zhang M, Qi J, Yu S, Afshin A, Gakidou E, Glenn S, Krish VS, Miller-Petrie MK, Mountjoy-Venning WC, Mullany EC, Redford SB, Liu H, Naghavi M, Hay SI, Wang L, Murray CJL, Liang X (2019) Mortality, morbidity, and risk factors in China and its provinces, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet (London) 394:1145–1158
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest concerning the materials or methods used in this study or the findings specified in this paper. The authors have applied for a patent for the device described in this publication (Authorized by National Intellectual Property Administration, PRC; Patent number: ZL 2017 2 0695409.9).
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Liu, Yq., Song, Zh., Liu, Cy. et al. A novel surgical technique for spontaneous intracerebral hematoma evacuation. Neurosurg Rev 44, 925–934 (2021). https://doi.org/10.1007/s10143-020-01252-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10143-020-01252-z