Abstract
Objective: Image quality in high-field intraoperative MRI (iMRI) is often influenced negatively by susceptibility artifacts. While routine sequences are rather robust, advanced imaging such as diffusion-weighted imaging (DWI) is very sensitive to susceptibility resulting in insufficient imaging data. This study aims to analyze intraoperatively acquired DWI to identify the main factors for susceptibility, to compare results with postoperative images and to identify technical aspects for improvement of intraoperative DWI.
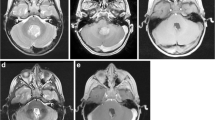
Methods: 100 patients with intraaxial lesions operated in a high-field iMRI were analyzed retrospectively for the quality of intraoperative DWI in comparison to the postoperative scan. General quality of the MR scan, individual diffusion restrictions, artifacts, and their causes were analyzed.
Results: Inclusion criteria were met in 78 patients, 124 diffusion restrictions were included in the comparative analysis. PPV and NPV for the detection of DWI changes intraoperatively were 0.94 and 0.56, respectively (SEN 0.94; SPE 0.56). Image quality was rated significantly (p < 0.0001) worse intraoperatively compared to the postoperative MRI. The main reasons for reduced image quality intraoperatively were air (64%) and artificial material (e.g., compress) (38%) in the resection cavity, as well as positioning of patient’s head outside the MR’s isocenter 37%. Analysis of surgical approaches showed that frontal craniotomies have the highest risk of limited image quality (40%), whereat better results (15% limited image quality) were seen for all other approaches (p = 0.059).
Conclusion: Intraoperative DWI showed reliable results in this analysis. However, image-quality was limited severely in many cases leading to uncertainty in the interpretation. Susceptibility-causing factors might be prevented in many cases, if the surgical team is aware of them. The most important factors are good filling of the resection cavity with irrigation fluid, not placing artificial materials in the resection cavity and adequate positioning of patient’s head according to the MR isocenter.





Similar content being viewed by others
References
Roder C, Breitkopf M, Bisdas S, Freitas RS, Dimostheni A, Ebinger M, Wolff M, Tatagiba M, Schuhmann MU (2016) Beneficial impact of high-field intraoperative magnetic resonance imaging on the efficacy of pediatric low-grade glioma surgery. Neurosurg Focus 40(3):E13. https://doi.org/10.3171/2015.11.focus15530
Roder C, Bisdas S, Ebner FH, Honegger J, Naegele T, Ernemann U, Tatagiba M (2014) Maximizing the extent of resection and survival benefit of patients in glioblastoma surgery: High-field iMRI versus conventional and 5-ALA-assisted surgery. Eur J Surg Oncol 40(3):297–304
Coburger J, Wirtz CR (2018) Fluorescence guided surgery by 5-ALA and intraoperative MRI in high grade glioma: a systematic review. J Neuro-Oncol 141:533–546. https://doi.org/10.1007/s11060-018-03052-4
Kuhnt D, Bauer MHA, Becker A, Merhof D, Zolal A, Richter M, Grummich P, Ganslandt O, Buchfelder M, Nimsky C (2012) Intraoperative visualization of fiber tracking based reconstruction of language pathways in glioma surgery. Neurosurgery 70(4):911–919; discussion 919-920. https://doi.org/10.1227/NEU.0b013e318237a807
Roder C, Bender B, Ritz R, Honegger J, Feigl G, Naegele T, Tatagiba MS, Ernemann U, Bisdas S (2013) Intraoperative visualization of residual tumor: the role of perfusion-weighted imaging in a high-field intraoperative magnetic resonance scanner. Neurosurgery 72:ons151–ons158
Roder C, Skardelly M, Ramina KF, Beschorner R, Honneger J, Nägele T, Tatagiba MS, Ernemann U, Bisdas S (2013) Spectroscopy imaging in intraoperative MR suite: tissue characterization and optimization of tumor resection. Int J Comput Assist Radiol Surg 9:551–559. https://doi.org/10.1007/s11548-013-0952-1
Nimsky C (2011) Intraoperative acquisition of fMRI and DTI. Neurosurg Clin N Am 22(2):269–277, ix. https://doi.org/10.1016/j.nec.2010.11.005
Roder C, Charyasz-Leks E, Breitkopf M, Decker K, Ernemann U, Klose U, Tatagiba M, Bisdas S (2016) Resting-state functional MRI in an intraoperative MRI setting: proof of feasibility and correlation to clinical outcome of patients. J Neurosurg:1–9. https://doi.org/10.3171/2015.7.jns15617
Masuda Y, Akutsu H, Ishikawa E, Matsuda M, Masumoto T, Hiyama T, Yamamoto T, Kohzuki H, Takano S, Matsumura A (2018) Evaluation of the extent of resection and detection of ischemic lesions with intraoperative MRI in glioma surgery: is intraoperative MRI superior to early postoperative MRI? J Neurosurg:1–8. https://doi.org/10.3171/2018.3.JNS172516
Smith JS, Cha S, Mayo MC, McDermott MW, Parsa AT, Chang SM, Dillon WP, Berger MS (2005) Serial diffusion-weighted magnetic resonance imaging in cases of glioma: distinguishing tumor recurrence from postresection injury. J Neurosurg 103(3):428–438. https://doi.org/10.3171/jns.2005.103.3.0428
Pala A, Brand C, Kapapa T, Hlavac M, Konig R, Schmitz B, Wirtz CR, Coburger J (2016) The value of intraoperative and early postoperative magnetic resonance imaging in low-grade glioma surgery: a retrospective study. World Neurosurg 93:191–197. https://doi.org/10.1016/j.wneu.2016.04.120
Stienen MN, Fierstra J, Pangalu A, Regli L, Bozinov O (2019) The Zurich checklist for safety in the intraoperative magnetic resonance imaging suite: technical note. Oper Neurosurg (Hagerstown) 16(6):756–765. https://doi.org/10.1093/ons/opy205
Reber PJ, Wong EC, Buxton RB, Frank LR (1998) Correction of off resonance-related distortion in echo-planar imaging using EPI-based field maps. Magn Reson Med 39(2):328–330
Andersson JL, Skare S, Ashburner J (2003) How to correct susceptibility distortions in spin-echo echo-planar images: application to diffusion tensor imaging. Neuroimage 20(2):870–888. https://doi.org/10.1016/s1053-8119(03)00336-7
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval and informed consent
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. As to the retrospective character of this analysis no specific formal consent was obtained.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Roder, C., Haas, P., Tatagiba, M. et al. Technical limitations and pitfalls of diffusion-weighted imaging in intraoperative high-field MRI. Neurosurg Rev 44, 327–334 (2021). https://doi.org/10.1007/s10143-019-01206-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10143-019-01206-0