Abstract
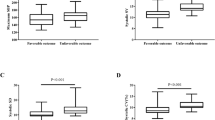
Few studies focused on the intraoperative blood pressure in Moyamoya disease (MMD) patients. We aimed to clarify whether or not it relates to early cerebral infarction after revascularization. We reviewed a retrospective cohort of Moyamoya disease from 2011 to 2018 in Beijing Tiantan Hospital, and patients with radiologically confirmed early postoperative infarction were included in the analysis. Controls were matched based on age, sex, and revascularization modality at a ratio of 1:5. Perioperative clinical factors and intraoperative blood pressure data were collected and analyzed. A total of 52 patients out of 1497 revascularization surgeries (3.5%) who experienced CT or MRI confirmed early postoperatively cerebral infarction, aged 38.46 ± 11.70; 26 were male (50.0%). Average real variability (ARV)-systolic blood pressure (SBP) (OR 3.29, p = 0.003), ARV-diastolic blood pressure (DBP) (OR 4.10, p = 0.005), ARV-mean arterial pressure (MAP) (OR 4.08, p = 0.004), and the maximum drops of DBP (OR 1.08, p = 0.003) and MAP (OR 1.06, p = 0.004) were associated with early postoperative infarction. In patients who experienced massive cerebral infarction, the maximum drops of DBP (OR 1.11, p = 0.004) and MAP (OR 1.11, p = 0.003) are independent risk factors, whereas ARVs of SBP (OR 3.90, p < 0.001), DBP (OR 4.69, p = 0.008), and MAP (OR 4.72, p = 0.003) are significantly associated with regional infarction. High variance of intraoperative blood pressure and drastic blood pressure decline are independent risk factors for postoperative infarction in MMD patients who underwent revascularization surgery. Maintaining stable intraoperative blood pressure is suggested to prevent early postoperative cerebral infarction in MMD patients.

Similar content being viewed by others
References
Antonucci MU, Burns TC, Pulling TM, Rosenberg J, Marks MP, Steinberg GK, Zaharchuk G (2016) Acute preoperative infarcts and poor cerebrovascular reserve are independent risk factors for severe ischemic complications following direct extracranial-intracranial bypass for Moyamoya disease. AJNR Am J Neuroradiol 37:228–235. https://doi.org/10.3174/ajnr.A4535
Bao X-Y, Duan L, Li D-S, Yang W-Z, Sun W-J, Zhang Z-S, Zong R, Han C (2012) Clinical features, surgical treatment and long-term outcome in adult patients with Moyamoya disease in China. Cerebrovasc Dis 34:305–313. https://doi.org/10.1159/000343225
Bijker JB, Persoon S, Peelen LM, Moons KGM, Kalkman CJ, Kappelle LJ, van Klei WA (2012) Intraoperative hypotension and perioperative ischemic stroke after general surgery: a nested case-control study. Anesthesiology 116:658–664. https://doi.org/10.1097/ALN.0b013e3182472320
Cho W-S, Kim JE, Kim CH, Ban SP, Kang H-S, Son Y-J, Bang JS, Sohn C-H, Paeng JC, Oh CW (2014) Long-term outcomes after combined revascularization surgery in adult moyamoya disease. Stroke 45:3025–3031. https://doi.org/10.1161/STROKEAHA.114.005624
Deng X, Gao F, Zhang D, Zhang Y, Wang R, Wang S, Cao Y, Zhao Y, Pan Y, Liu X, Zhang Q, Zhao J (2018) Direct versus indirect bypasses for adult ischemic-type moyamoya disease: a propensity score-matched analysis. J Neurosurg 128:1785–1791. https://doi.org/10.3171/2017.2.JNS162405
Fujimura M, Inoue T, Shimizu H, Saito A, Mugikura S, Tominaga T (2012) Efficacy of prophylactic blood pressure lowering according to a standardized postoperative management protocol to prevent symptomatic cerebral hyperperfusion after direct revascularization surgery for moyamoya disease. Cerebrovasc Dis 33:436–445. https://doi.org/10.1159/000336765
Fujimura M, Tominaga T (2015) Current status of revascularization surgery for Moyamoya disease: special consideration for its “internal carotid-external carotid (IC-EC) conversion” as the physiological reorganization system. Tohoku J Exp Med 236:45–53. https://doi.org/10.1620/tjem.236.45
Funaki T, Takahashi JC, Takagi Y, Kikuchi T, Yoshida K, Mitsuhara T, Kataoka H, Okada T, Fushimi Y, Miyamoto S (2015) Unstable moyamoya disease: clinical features and impact on perioperative ischemic complications. J Neurosurg 122:400–407. https://doi.org/10.3171/2014.10.JNS14231
Futier E, Lefrant J-Y, Guinot P-G, Godet T, Lorne E, Cuvillon P, Bertran S, Leone M, Pastene B, Piriou V, Molliex S, Albanese J, Julia J-M, Tavernier B, Imhoff E, Bazin J-E, Constantin J-M, Pereira B, Jaber S, INPRESS Study Group (2017) Effect of individualized vs standard blood pressure management strategies on postoperative organ dysfunction among high-risk patients undergoing major surgery: a randomized clinical trial. JAMA 318:1346–1357. https://doi.org/10.1001/jama.2017.14172
Guzman R, Lee M, Achrol A, Bell-Stephens T, Kelly M, Do HM, Marks MP, Steinberg GK (2009) Clinical outcome after 450 revascularization procedures for moyamoya disease. Clinical article. J Neurosurg 111:927–935. https://doi.org/10.3171/2009.4.JNS081649
Houkin K, Kuroda S, Ishikawa T, Abe H (2000) Neovascularization (angiogenesis) after revascularization in moyamoya disease. Which technique is most useful for moyamoya disease? Acta Neurochir 142:269–276
Jung YJ, Ahn JS, Kwon DH, Kwun BD (2011) Ischemic complications occurring in the contralateral hemisphere after surgical treatment of adults with moyamoya disease. J Korean Neurosurg Soc 50:492–496. https://doi.org/10.3340/jkns.2011.50.6.492
Kashiwazaki D, Akioka N, Kuwayama N, Houkin K, Czabanka M, Vajkoczy P, Kuroda S (2017) Berlin grading system can stratify the onset and predict perioperative complications in adult moyamoya disease. Neurosurgery 81:986–991. https://doi.org/10.1093/neuros/nyx140
Kazumata K, Ito M, Tokairin K, Ito Y, Houkin K, Nakayama N, Kuroda S, Ishikawa T, Kamiyama H (2014) The frequency of postoperative stroke in moyamoya disease following combined revascularization: a single-university series and systematic review. J Neurosurg 121:432–440. https://doi.org/10.3171/2014.1.JNS13946
Khan N, Achrol AS, Guzman R, Burns TC, Dodd R, Bell-Stephens T, Steinberg GK (2012) Sex differences in clinical presentation and treatment outcomes in Moyamoya disease. Neurosurgery 71:587–593– discussion 593. https://doi.org/10.1227/NEU.0b013e3182600b3c
Kim JS (2016) Moyamoya disease: epidemiology, clinical features, and diagnosis. J Stroke 18:2–11. https://doi.org/10.5853/jos.2015.01627
Kim S-H, Choi J-U, Yang K-H, Kim T-G, Kim D-S (2005) Risk factors for postoperative ischemic complications in patients with moyamoya disease. J Neurosurg 103:433–438. https://doi.org/10.3171/ped.2005.103.5.0433
Kim T, Oh CW, Bang JS, Kim JE, Cho W-S (2016) Moyamoya disease: treatment and outcomes. J Stroke 18:21–30. https://doi.org/10.5853/jos.2015.01739
Kim T, Oh CW, Kwon O-K, Hwang G, Kim JE, Kang H-S, Cho W-S, Bang JS (2016) Stroke prevention by direct revascularization for patients with adult-onset moyamoya disease presenting with ischemia. J Neurosurg 124:1788–1793. https://doi.org/10.3171/2015.6.JNS151105
Kraemer M, Sassen J, Karakaya R, Schwitalla JC, Graf J, Albrecht P, Hartung H-P, Diehl RR, Berlit P, Laumer R, Diesner F (2018) Moyamoya angiopathy: early postoperative course within 3 months after STA-MCA-bypass surgery in Europe-a retrospective analysis of 64 procedures. J Neurol 265:2370–2378. https://doi.org/10.1007/s00415-018-8997-2
Likosky DS, CAS M, Caplan LR, Baribeau YR, Morton JR, Weintraub RM, Hartman GS, Hernandez F, Braff SP, Charlesworth DC, Malenka DJ, Ross CS, O’Connor GT, Northern New England Cardiovascular Disease Study Group (2003) Determination of etiologic mechanisms of strokes secondary to coronary artery bypass graft surgery. Stroke 34:2830–2834. https://doi.org/10.1161/01.STR.0000098650.12386.B3
Limburg M, Wijdicks EF, Li H (1998) Ischemic stroke after surgical procedures: clinical features, neuroimaging, and risk factors. Neurology 50:895–901
Liu X-J, Zhang D, Wang S, Zhao Y-L, Teo M, Wang R, Cao Y, Ye X, Kang S, Zhao J-Z (2015) Clinical features and long-term outcomes of moyamoya disease: a single-center experience with 528 cases in China. J Neurosurg 122:392–399. https://doi.org/10.3171/2014.10.JNS132369
Macyszyn L, Attiah M, Ma TS, Ali Z, Faught R, Hossain A, Man K, Patel H, Sobota R, Zager EL, Stein SC (2017) Direct versus indirect revascularization procedures for moyamoya disease: a comparative effectiveness study. J Neurosurg 126:1523–1529. https://doi.org/10.3171/2015.8.JNS15504
Mascha EJ, Yang D, Weiss S, Sessler DI (2015) Intraoperative mean arterial pressure variability and 30-day mortality in patients having noncardiac surgery. Anesthesiology 123:79–91. https://doi.org/10.1097/ALN.0000000000000686
Miettinen OS (1985) Theoretical Epidemiology: Principles of Occurrence Research in Medicine. Wiley & Sons, New York
Miyamoto S, Yoshimoto T, Hashimoto N, Okada Y, Tsuji I, Tominaga T, Nakagawara J, Takahashi JC, JAM Trial Investigators (2014) Effects of extracranial-intracranial bypass for patients with hemorrhagic moyamoya disease: results of the Japan Adult Moyamoya Trial. Stroke 45:1415–1421. https://doi.org/10.1161/STROKEAHA.113.004386
Park S-E, Kim J-S, Park EK, Shim K-W, Kim D-S (2018) Direct versus indirect revascularization in the treatment of moyamoya disease. J Neurosurg 129:480–489. https://doi.org/10.3171/2017.5.JNS17353
Research Committee on the Pathology and Treatment of Spontaneous Occlusion of the Circle of Willis, Health Labour Sciences Research Grant for Research on Measures for Infractable Diseases (2012) Guidelines for diagnosis and treatment of moyamoya disease (spontaneous occlusion of the circle of Willis). Neurol Med Chir (Tokyo) 52:245–266
Sato K, Shirane R, Yoshimoto T (1997) Perioperative factors related to the development of ischemic complications in patients with moyamoya disease. Childs Nerv Syst 13:68–72. https://doi.org/10.1007/s003810050044
Scott RM, Smith ER (2009) Moyamoya disease and moyamoya syndrome. N Engl J Med 360:1226–1237. https://doi.org/10.1056/NEJMra0804622
Starke RM, Komotar RJ, Connolly ES (2009) Optimal surgical treatment for moyamoya disease in adults: direct versus indirect bypass. Neurosurg Focus 26:E8. https://doi.org/10.3171/2009.01.FOCUS08309
Sun LY, Wijeysundera DN, Tait GA, Beattie WS (2015) Association of intraoperative hypotension with acute kidney injury after elective noncardiac surgery. Anesthesiology 123:515–523. https://doi.org/10.1097/ALN.0000000000000765
Šidák Z (1967) Rectangular confidence regions for the means of multivariate normal distributions. J Am Stat Assoc 62:626–633. https://doi.org/10.1080/01621459.1967.10482935
van Wermeskerken GK, Lardenoye JW, Hill SE, Grocott HP, Phillips-Bute B, Smith PK, Reves JG, Newman MF (2000) Intraoperative physiologic variables and outcome in cardiac surgery: part II. Neurologic outcome. Ann Thorac Surg 69:1077–1083
Walsh M, Devereaux PJ, Garg AX, Kurz A, Turan A, Rodseth RN, Cywinski J, Thabane L, Sessler DI (2013) Relationship between intraoperative mean arterial pressure and clinical outcomes after noncardiac surgery: toward an empirical definition of hypotension. Anesthesiology 119:507–515. https://doi.org/10.1097/ALN.0b013e3182a10e26
Wesselink EM, Kappen TH, Torn HM, Slooter AJC, van Klei WA (2018) Intraoperative hypotension and the risk of postoperative adverse outcomes: a systematic review. Br J Anaesth 121:706–721. https://doi.org/10.1016/j.bja.2018.04.036
Yin H, Liu X, Zhang D, Zhang Y, Wang R, Zhao M, Zhao J (2018) A novel staging system to evaluate cerebral hypoperfusion in patients with moyamoya disease. Stroke 49:2837–2843. https://doi.org/10.1161/STROKEAHA.118.022628
Zhai X, Mao L, Wang H, Zhang X, Hang C, Wu W, Jia Y, Liu L (2018) Risk factors associated with neurologic deterioration after combined direct and indirect revascularization in patients with moyamoya disease on the East Coast of China. World Neurosurg 118:e92–e98. https://doi.org/10.1016/j.wneu.2018.06.125
Zhao M, Deng X, Zhang D, Wang S, Zhang Y, Wang R, Zhao J (2018) Risk factors for and outcomes of postoperative complications in adult patients with moyamoya disease. J Neurosurg 20:1–12. https://doi.org/10.3171/2017.10.JNS171749
Funding
This study was funded by Beijing Municipal Administration of Hospitals’ Mission Plan (SML2015050) and the Program of the National Natural Science Foundation of China (81701137).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
The study was performed according to the guidelines of the Helsinki Declaration and was approved by the ethics committee of Beijing Tiantan Hospital.
Informed consent
Written informed consent was obtained from all patients included.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Li, J., Zhao, Y., Zhao, M. et al. High variance of intraoperative blood pressure predicts early cerebral infarction after revascularization surgery in patients with Moyamoya disease. Neurosurg Rev 43, 759–769 (2020). https://doi.org/10.1007/s10143-019-01118-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10143-019-01118-z