Abstract
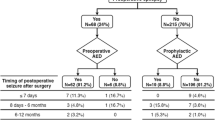
This retrospective study explored the risk factors for the occurrence of seizures in the pre- and postoperative period in patients undergoing supratentorial meningiomas surgery to investigate those who are likely to benefit from prophylactic antiepileptic drugs (AEDs). We reviewed the medical records of 778 supratentorial meningiomas patients who were operated at our institution between 2011 and 2012. A total of 100 (12.9%) patients experienced preoperative seizures; 41 patients (5.3%) experienced postoperative in-hospital seizures, and 91 (13.5%, n = 673) patients experienced postoperative seizures after discharge. Multivariate analysis revealed that motor cortex involvement (odds ratio [OR] 3.243, P < 0.001) and peritumoral edema ≥ 1 cm (OR 3.936, P < 0.001) were significant risk factors of preoperative seizures. Whereas presenting with headache (OR 0.259, P < 0.001) and age ≥ 55 years at surgery (OR 0.514, P = 0.009) showed decreased incidence of preoperative seizures. The involvement of motor cortex (OR 3.290, P = 0.003), postoperative Karnofsky Performance Scale (KPS) ≤ 70 (OR 5.389, P < 0.001), preoperative seizure (OR 4.003, P < 0.001), and occurrence of any medical/surgical complication (OR 3.925, P = 0.001) were significant risk factors for postoperative in-hospital seizures. Postoperative seizures after discharge were associated with tumor maximal diameter ≥ 3.5 cm (OR 1.903, P = 0.022), preoperative seizures (OR 4.350, P < 0.001), postoperative in-hospital seizures (OR 6.385, P < 0.001), and tumor recurrence/progression (OR 7.642, P < 0.001). The probability of seizure freedom in the 5-year follow-up was roughly 59% among patients with preoperative seizures, and 87% among patients without preoperative seizures. Cox regression analysis showed that tumor recurrence/progression (relative risk 2.987, 95% CI 1.517, 5.879, P = 0.002) was the only predictor of postoperative seizures in patients without a history of preoperative epilepsy. The use of postoperative prophylactic antiepileptic drug (AED) did not reduce the incidence of seizures in our analysis. Understanding the risk factors for seizures might help clinicians to predict their occurrence and develop effective anti-epileptic treatment strategies. Further prospective randomized controlled trials are needed to determine the risk factors for seizures and the efficacy of AED prophylaxis.


Similar content being viewed by others
References
Baumgarten P, Sarlak M, Baumgarten G, Marquardt G, Seifert V, Strzelczyk A, Rosenow F, Freiman TM (2018) Focused review on seizures caused by meningiomas. Epilepsy Behav 88:146–151. https://doi.org/10.1016/j.yebeh.2018.09.002
Beghi E, Carpio A, Forsgren L, Hesdorffer D, Malmgren K, Sander J, Tomson T, Hauser W (2010) Recommendation for a definition of acute symptomatic seizure. Epilepsia 51:671–675
Buckingham S, Campbell S, Haas B, Montana V, Robel S, Ogunrinu T, Sontheimer H (2011) Glutamate release by primary brain tumors induces epileptic activity. Nat Med 17:1269–1274
Chaichana K, Pendleton C, Zaidi H, Olivi A, Weingart J, Gallia G, Lim M, Brem H, Quiñones-Hinojosa A (2013) Seizure control for patients undergoing meningioma surgery. World Neurosurg 79:515–524
Chen WC, Magill ST, Englot DJ, Baal JD, Wagle S, Rick JW, McDermott MW (2017) Factors associated with pre- and postoperative seizures in 1033 patients undergoing supratentorial meningioma resection. Neurosurgery 81:297–306. https://doi.org/10.1093/neuros/nyx001
Claus E, Bondy M, Schildkraut J, Wiemels J, Wrensch M, Black P (2005) Epidemiology of intracranial meningioma. Neurosurgery 57:1088–1095; discussion 1088-1095
Englot DJ, Magill ST, Han SJ, Chang EF, Berger MS, McDermott MW (2016) Seizures in supratentorial meningioma: a systematic review and meta-analysis. J Neurosurg 124:1552–1561. https://doi.org/10.3171/2015.4.jns142742
Glantz M, Cole B, Forsyth P, Recht L, Wen P, Chamberlain M, Grossman S, Cairncross J (2000) Practice parameter: anticonvulsant prophylaxis in patients with newly diagnosed brain tumors. Report of the quality standards Subcommittee of the American Academy of neurology. Neurology 54:1886–1893
Hasseleid B, Meling T, Rønning P, Scheie D, Helseth E (2012) Surgery for convexity meningioma: Simpson grade I resection as the goal: clinical article. J Neurosurg 117:999–1006
Islim AI, Ali A, Bagchi A, Ahmad MU, Mills SJ, Chavredakis E, Brodbelt AR, Jenkinson MD (2018) Postoperative seizures in meningioma patients: improving patient selection for antiepileptic drug therapy. J Neuro-Oncol 140:123–134. https://doi.org/10.1007/s11060-018-2941-2
Jacoby A, Gamble C, Doughty J, Marson A, Chadwick D (2007) Quality of life outcomes of immediate or delayed treatment of early epilepsy and single seizures. Neurology 68:1188–1196
Komotar R, Raper D, Starke R, Iorgulescu J, Gutin P (2011) Prophylactic antiepileptic drug therapy in patients undergoing supratentorial meningioma resection: a systematic analysis of efficacy. J Neurosurg 115:483–490
Krumholz A (2009) Driving issues in epilepsy: past, present, and future. Epilepsy Curr 9:31–35
Louis DN, Perry A, Reifenberger G, von Deimling A, Figarella-Branger D, Cavenee WK, Ohgaki H, Wiestler OD, Kleihues P, Ellison DW (2016) The 2016 World Health Organization classification of tumors of the central nervous system: a summary. Acta Neuropathol 131:803–820. https://doi.org/10.1007/s00401-016-1545-1
Neal A, Morokoff A, O'Brien T, Kwan P (2016) Postoperative seizure control in patients with tumor-associated epilepsy. Epilepsia 57:1779–1788
Ostrom Q, Gittleman H, Fulop J, Liu M, Blanda R, Kromer C, Wolinsky Y, Kruchko C, Barnholtz-Sloan J (2015) CBTRUS statistical report: primary brain and central nervous system tumors diagnosed in the United States in 2008-2012. Neuro-Oncology 17(Suppl 4):iv1–iv62
Oushy S, Sillau SH, Ney DE, Damek DM, Youssef AS, Lillehei KO, Ormond DR (2018) New-onset seizure during and after brain tumor excision: a risk assessment analysis. J Neurosurg 128:1713–1718. https://doi.org/10.3171/2017.2.JNS162315
Pulman J, Greenhalgh J, Marson A (2013) Antiepileptic drugs as prophylaxis for post-craniotomy seizures. Cochrane Database Syst Rev:CD007286
Sayegh E, Fakurnejad S, Oh T, Bloch O, Parsa A (2014) Anticonvulsant prophylaxis for brain tumor surgery: determining the current best available evidence. J Neurosurg 121:1139–1147
Schoenegger K, Oberndorfer S, Wuschitz B, Struhal W, Hainfellner J, Prayer D, Heinzl H, Lahrmann H, Marosi C, Grisold W (2009) Peritumoral edema on MRI at initial diagnosis: an independent prognostic factor for glioblastoma? Eur J Neurol 16:874–878
Skardelly M, Rother C, Noell S, Behling F, Wuttke TV, Schittenhelm J, Bisdas S, Meisner C, Rona S, Tabatabai G, Roser F, Tatagiba MS (2017) Risk factors of preoperative and early postoperative seizures in patients with meningioma: a retrospective single-center cohort study. World Neurosurg 97:538–546. https://doi.org/10.1016/j.wneu.2016.10.062
Sughrue M, Kane A, Shangari G, Rutkowski M, McDermott M, Berger M, Parsa A (2010) The relevance of Simpson grade I and II resection in modern neurosurgical treatment of World Health Organization grade I meningiomas. J Neurosurg 113:1029–1035
Sughrue M, Rutkowski M, Chang E, Shangari G, Kane A, McDermott M, Berger M, Parsa A (2011) Postoperative seizures following the resection of convexity meningiomas: are prophylactic anticonvulsants indicated? Clinical article J Neurosurg 114:705–709
van Breemen MSM, Wilms EB, Vecht CJ (2007) Epilepsy in patients with brain tumours: epidemiology, mechanisms, and management. The Lancet Neurology 6:421–430. https://doi.org/10.1016/s1474-4422(07)70103-5
Wirsching H-G, Morel C, Gmür C, Neidert MC, Baumann CR, Valavanis A, Rushing EJ, Krayenbühl N, Weller M (2016) Predicting outcome of epilepsy after meningioma resection. Neuro-Oncology 18:1002–1010. https://doi.org/10.1093/neuonc/nov303
Wu A, Trinh V, Suki D, Graham S, Forman A, Weinberg J, McCutcheon I, Prabhu S, Heimberger A, Sawaya R, Wang X, Qiao W, Hess K, Lang F (2013) A prospective randomized trial of perioperative seizure prophylaxis in patients with intraparenchymal brain tumors. J Neurosurg 118:873–883
Xue H, Sveinsson O, Bartek J Jr, Forander P, Skyrman S, Kihlstrom L, Shafiei R, Mathiesen T, Tomson T (2018) Long-term control and predictors of seizures in intracranial meningioma surgery: a population-based study. Acta Neurochir 160:589–596. https://doi.org/10.1007/s00701-017-3434-3
Yamasaki F, Yoshioka H, Hama S, Sugiyama K, Arita K, Kurisu K (2000) Recurrence of meningiomas. Cancer 89:1102–1110
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. For this retrospective study, formal consent was not required.
Informed consent
Informed consent was obtained from all individual participants who were included in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Li, X., Wang, C., Lin, Z. et al. Risk factors and control of seizures in 778 Chinese patients undergoing initial resection of supratentorial meningiomas. Neurosurg Rev 43, 597–608 (2020). https://doi.org/10.1007/s10143-019-01085-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10143-019-01085-5