Abstract
Introduction
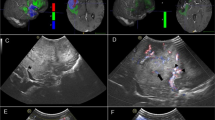
Linear array intraoperative ultrasound (lioUS) is an emerging technology for intracranial use. We evaluated sensitivity and specificity of lioUS to detect residual tumor in patients harboring a glioblastoma.
Methods
After near total resection in 20 patients, residual tumor detection using lioUS, conventional intraoperative ultrasound (cioUS), and gadopentetic-diethylenetriamine penta-acetic acid (Gd-DTPA)-enhanced intraoperative MRI (iMRI) were compared. Sensitivity and specificity were calculated based on 68 navigated biopsies. Receiver operator characteristic (ROC) curves and correlation with histopathological findings of each imaging modality were calculated. Additionally, results were evaluated in the subgroup of recurrent disease (23 biopsies in 8 patients).
Results
Sensitivity of lioUS (76 %) was significantly higher compared with iMRI (55 %) and cioUS (24 %). Specificity of lioUS (58 %) was significantly lower than in cioUS (96 %), while there was no significant difference to iMRI (74 %). All imaging modalities correlated significantly with histopathological findings. In the subgroup of recurrent disease, sensitivity and specificity decreased in all modalities. However, cioUS showed significant lower values than iMRI and lioUS. In ROC curves, lioUS showed a higher area und the curve (AUC) in comparison with iMRI and cioUS. We found similar results in the subgroup of recurrent disease.
Conclusion
Tumor detection using a lioUS is significantly superior to cioUS. Overall test performance in lioUS is comparable with results of iMRI. While, the latter has a higher specificity and a significantly lower sensitivity in comparison with lioUS.




Similar content being viewed by others
References
Bozinov O, Burkhardt JK (2012) Intra-operative computed-tomography-like real-time three-dimensional ultrasound in neurosurgery. World Neurosurg 78(1–2):5–7. doi:10.1016/j.wneu.2012.05.025
Bozinov O, Burkhardt JK, Woernle CM, Hagel V, Ulrich NH, Krayenbuhl N, Bertalanffy H (2012) Intra-operative high frequency ultrasound improves surgery of intramedullary cavernous malformations. Neurosurg Rev 35((2):269–275. doi:10.1007/s10143-011-0364-z, discussion 275
Chandler WF, Knake JE, McGillicuddy JE, Lillehei KO, Silver TM (1982) Intraoperative use of real-time ultrasonography in neurosurgery. J Neurosurg 57(2):157–163. doi:10.3171/jns.1982.57.2.0157
Coburger J, Engelke J, Scheuerle A, Thal DR, Hlavac M, Wirtz CR, Konig R (2014) Tumor detection with 5-aminolevulinic acid fluorescence and Gd-DTPA-enhanced intraoperative MRI at the border of contrast-enhancing lesions: a prospective study based on histopathological assessment. Neurosurg Focus 36(2):E3. doi:10.3171/2013.11.FOCUS13463
Coburger J, König RW, Scheuerle A, Engelke J, Hlavac M, Thal DR, Wirtz CR (2014) Navigated high frequency ultrasound: description of technique and first clinical comparison with conventional intracranial ultrasound. World Neurosurg
Doyle TE, Factor RE, Ellefson CL, Sorensen KM, Ambrose BJ, Goodrich JB, Hart VP, Jensen SC, Patel H, Neumayer LA (2011) High-frequency ultrasound for intraoperative margin assessments in breast conservation surgery: a feasibility study. BMC Cancer 11:444. doi:10.1186/1471-2407-11-444
Gerganov VM, Samii A, Akbarian A, Stieglitz L, Samii M, Fahlbusch R (2009) Reliability of intraoperative high-resolution 2D ultrasound as an alternative to high-field strength MR imaging for tumor resection control: a prospective comparative study. J Neurosurg 111(3):512–519
Gronningsaeter A, Kleven A, Ommedal S, Aarseth TE, Lie T, Lindseth F, Lango T, Unsgard G (2000) SonoWand, an ultrasound-based neuronavigation system. Neurosurgery 47(6):1373–1379, discussion 1379–1380
Hanley JA, McNeil BJ (1982) The meaning and use of the area under a receiver operating characteristic (ROC) curve. Radiology 143(1):29–36. doi:10.1148/radiology.143.1.7063747
Koenig RW, Schmidt TE, Heinen CP, Wirtz CR, Kretschmer T, Antoniadis G, Pedro MT (2011) Intraoperative high-resolution ultrasound: a new technique in the management of peripheral nerve disorders. J Neurosurg 114(2):514–521
Krekel NM, Zonderhuis BM, Schreurs HW, Cardozo AM, Rijna H, van der Veen H, Muller S, Poortman P, de Widt L, de Roos WK, Bosch AM, van Taets AAH, Bergers E, van der Linden MH, de DeLange Klerk ES, Winters HA, Meijer S, van den Tol PM (2011) Ultrasound-guided breast-sparing surgery to improve cosmetic outcomes and quality of life. A prospective multicentre randomised controlled clinical trial comparing ultrasound-guided surgery to traditional palpation-guided surgery (COBALT trial). BMC Surg 11:8. doi:10.1186/1471-2482-11-8
Kubben PL, Wesseling P, Lammens M, Schijns OE, Ter Laak-Poort MP, van Overbeeke JJ, van Santbrink H (2012) Correlation between contrast enhancement on intraoperative magnetic resonance imaging and histopathology in glioblastoma. Surg Neurol Int 3:158
Lacroix M, Abi-Said D, Fourney DR, Gokaslan ZL, Shi W, DeMonte F, Lang FF, McCutcheon IE, Hassenbusch SJ, Holland E, Hess K, Michael C, Miller D, Sawaya R (2001) A multivariate analysis of 416 patients with glioblastoma multiforme: prognosis, extent of resection, and survival. J Neurosurg 95(2):190–198. doi:10.3171/jns.2001.95.2.0190
Louis DN, Ohgaki H, Wiestler OD, Cavenee WK, Burger PC, Jouvet A, Scheithauer BW, Kleihues P (2007) The 2007 WHO Classification of Tumours of the Central Nervous System. Acta Neuropathol 114(2):97–109
Marko NF, Weil RJ, Schroeder JL, Lang FF, Suki D, Sawaya RE et al (2014) Extent of resection of glioblastoma revisited: personalized survival modeling facilitates more accurate survival prediction and supports a maximum-safe-resection approach to surgery. J Clin Oncol: Off J Am Soc Clin Oncol 32(8):774–782. doi:10.1200/jco.2013.51.8886
Marko NF, Weil RJ, Schroeder JL, Lang FF, Suki D, Sawaya RE (2014) Extent of resection of glioblastoma revisited: personalized survival modeling facilitates more accurate survival prediction and supports a maximum-safe-resection approach to surgery. J Clin Oncol. doi:10.1200/jco.2013.51.8886
Moiyadi A, Shetty P, Mahajan A, Udare A, Sridhar E (2013) Usefulness of three-dimensional navigable intraoperative ultrasound in resection of brain tumors with a special emphasis on malignant gliomas. Acta Neurochir 155(12):2217–2225. doi:10.1007/s00701-013-1881-z
Moran CM, Pye SD, Ellis W, Janeczko A, Morris KD, McNeilly AS, Fraser HM (2011) A comparison of the imaging performance of high resolution ultrasound scanners for preclinical imaging. Ultrasound Med Biol 37(3):493–501. doi:10.1016/j.ultrasmedbio.2010.11.010
Rasmussen IA Jr, Lindseth F, Rygh OM, Berntsen EM, Selbekk T, Xu J, Nagelhus Hernes TA, Harg E, Haberg A, Unsgaard G (2007) Functional neuronavigation combined with intra-operative 3D ultrasound: initial experiences during surgical resections close to eloquent brain areas and future directions in automatic brain shift compensation of preoperative data. Acta Neurochir 149(4):365–378
Renovanz M, Hickmann AK, Henkel C, Nadji-Ohl M, Hopf NJ (2014) Navigated versus non-navigated intraoperative ultrasound: is there any impact on the extent of resection of high-grade gliomas? A retrospective clinical analysis. J Neurol Surg A Cent Eur Neurosurg. doi:10.1055/s-0033-1356486
Rygh OM, Selbekk T, Torp SH, Lydersen S, Hernes TA, Unsgaard G (2008) Comparison of navigated 3D ultrasound findings with histopathology in subsequent phases of glioblastoma resection. Acta Neurochir 150(10):1033–1041, discussion 1042
Sanai N, Polley MY, McDermott MW, Parsa AT, Berger MS (2011) An extent of resection threshold for newly diagnosed glioblastomas. J Neurosurg 115(1):3–8. doi:10.3171/2011.2.jns10998
Selbekk T, Jakola AS, Solheim O, Johansen TF, Lindseth F, Reinertsen I, Unsgard G (2013) Ultrasound imaging in neurosurgery: approaches to minimize surgically induced image artefacts for improved resection control. Acta Neurochirurgica
Serra C, Stauffer A, Actor B, Burkhardt JK, Ulrich NH, Bernays RL, Bozinov O (2012) Intraoperative high frequency ultrasound in intracerebral high-grade tumors. Ultraschall Med 33(7):E306–E312. doi:10.1055/s-0032-1325369, Stuttgart, Germany : 1980
Solheim O, Selbekk T, Jakola A, Unsgård G (2010) Ultrasound-guided operations in unselected high-grade gliomas—overall results, impact of image quality and patient selection. Acta Neurochir 152(11):1873–1886. doi:10.1007/s00701-010-0731-5
Stummer W, Pichlmeier U, Meinel T, Wiestler OD, Zanella F, Reulen H-J (2006) Fluorescence-guided surgery with 5-aminolevulinic acid for resection of malignant glioma: a randomised controlled multicentre phase III trial. Lancet Oncol 7(5):392–401. doi:10.1016/s1470-2045(06)70665-9
Tirakotai W, Miller D, Heinze S, Benes L, Bertalanffy H, Sure U (2006) A novel platform for image-guided ultrasound. Neurosurgery 58(4):710–718, discussion 710–718. d
Ulrich NH, Burkhardt JK, Serra C, Bernays RL, Bozinov O (2012) Resection of pediatric intracerebral tumors with the aid of intraoperative real-time 3-D ultrasound. Childs Nerv Syst 28(1):101–109. doi:10.1007/s00381-011-1571-1
Unsgard G, Solheim O, Lindseth F, Selbekk T (2011) Intra-operative imaging with 3D ultrasound in neurosurgery. Acta Neurochir Suppl 109:181–186
Conflict of interest
The Department of Neurosurgery was provided with a software plug-in and the hardware to integrate ioUS in the neuronavigation software for scientific use by Brainlab AG (Feldkirchen, Germany). RK has worked as a medical consultant for Brainlab AG (Feldkirchen, Germany). DRT received consultancies from Simon-Kucher and Partners (Germany), Covance Laboratories (UK), and GE-Healthcare (UK), received a speaker honorarium from GE-Healthcare (UK) and collaborated with Novartis Pharma Basel (Switzerland).
Author information
Authors and Affiliations
Corresponding author
Additional information
Comments
Marian Neidert, Oliver Bozinov, Zurich, Switzerland
Coburger and colleagues present a prospective non-randomized single-center study (class IV) on the usefulness of intraoperative linear array ultrasound (lioUS) in glioblastoma surgery. In this study, lioUS was compared (first time) to high field ioMRI and to conventional ioUS. The authors conclude that lioUS is superior to cioUS in glioblastoma surgery and comparable with ioMRI (lioUS has a better sensitivity, but worse specificity).
Intraoperative ultrasound (ioUS) is often considered an “old” technology introduced in the 1960s that was not used frequently in neurosurgical practice over a long period of time due to suboptimal image quality. However, in recent years, ioUS had a comeback mainly because of technical improvements (reduced probe size allowing intracavital scanning, improved resolution with high-frequency probes, the option of 3D imaging and the option of linking ioUS to neuronavigation). Most importantly, ioUS offers true repetetive real time information, which is not the case with pure neuronavigation or in a delayed way with ioMRI or ioCT.
Regarding glioblastoma surgery, good evidence supports not only the idea of the extent of resection and the volume of residual disease but also new focal-neurological deficits following resection have a strong impact on patient outcome. As ioUS helps to differentiate between tumor and healthy brain tissue, ioUS can help in the balancing act of achieving a maximum resection while providing safety. Hence, the data provided in this manuscript are valuable to the neurosurgical community.
Rights and permissions
About this article
Cite this article
Coburger, J., Scheuerle, A., Kapapa, T. et al. Sensitivity and specificity of linear array intraoperative ultrasound in glioblastoma surgery: a comparative study with high field intraoperative MRI and conventional sector array ultrasound. Neurosurg Rev 38, 499–509 (2015). https://doi.org/10.1007/s10143-015-0627-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10143-015-0627-1