Abstract
The authors critically analyzed a large series of patients with hemifacial spasm (HFS) and who underwent microvascular decompression (MVD) under a prospective protocol. We describe several “lessons learned” that are required for achieving successful surgery and proper postoperative management. The purpose of this study is to report on our experience during the previous 10 years with this procedure and we also discuss various related topics. From April 1997 to June 2009, over 1,200 consecutive patients underwent MVD for HFS. Among them, 1,174 patients who underwent MVD for HFS with a minimum 1 year follow-up were enrolled in the study. The median follow-up period was 3.5 years (range, 1-9.3 years). Based on the operative and medical records, the intraoperative findings and the postoperative outcomes were obtained and then analyzed. At the 1-year follow-up examination, 1,105 (94.1%) patients of the total 1,174 patients exhibited a “cured” state, and 69 (5.9%) patients had residual spasms. In all the patients, the major postoperative complications included transient hearing loss in 31 (2.6%), permanent hearing loss in 13 (1.1%), transient facial weakness in 86 (7.3%), permanent facial weakness in 9 (0.7%), cerebrospinal fluid leak in three (0.25%) and cerebellar infarction or hemorrhage in two (0.17%). There were no operative deaths. Microvascular decompression is a very effective, safe modality of treatment for hemifacial spasm. MVD is not sophisticated surgery, but having a basic understanding of the surgical procedures is required to achieve successful surgery.



Similar content being viewed by others
References
Auger RG, Whisnant JP (1990) Hemifacial spasm in Rochester and Olmsted County, Minnesota, 1960 to 1984. Arch Neurol 47:1233–1234
Barker FG 2nd, Jannetta PJ, Bissonette DJ, Shields PT, Larkins MV, Jho HD (1995) Microvascular decompression for hemifacial spasm. J Neurosurg 82:201–210
Digre K, Corbett JJ (1988) Hemifacial spasm: differential diagnosis, mechanism, and treatment. Adv Neurol 49:151–176
Fukushima T (1995) Microvascular decompression for hemifacial spasm: results in 2890 cases. In: Carter LP, Spetzler RF (eds) Neurovascular surgery. McGraw Hill, New York, pp 1133–1145
Furukawa K, Sakoh M, Kumon Y, Teraoka M, Ohta S, Ohue S, Hatoh N, Ohnishi T (2003) Delayed facial palsy after microvascular decompression for hemifacial spasm due to reactivation of varicella-zoster virus. No Shinkei Geka 31:899–902
Gardner JW (1966) Crosstalk. The paradoxical transmission of a nerve impulse. Arch Neurol 14:149–156
Gardner JW, Sava GA (1962) Hemifacial spasm: a reversible pathophysiologic state. J Neurosurg 19:240–247
Hitotsumatsu T, Matsushima T, Inoue T (2003) Microvascular decompression for treatment of trigeminal neuralgia, hemifacial spasm, and glossopharyngeal neuralgia: three surgical approach variations: technical note. Neurosurgery 53:1436–1441, discussion 1442–1433
Jannetta PJ (1970) Microsurgical exploration and decompression of the facial nerve in hemifacial spasm. Curr Top Surg Res 2:217–220
Jannetta PJ (1975) The cause of hemifacial spasm: definitive microsurgical treatment at the brainstem in 31 patients. Trans Sect Otolaryngol Am Acad Ophthalmol Otolaryngol 80:319–322
Jannetta PJ, Resnick D (1996) Cranial rhizopathies. In: Youmans JR (ed) Neurological surgery: a comprehensive guide to the diagnosis and management of neurosurgical problems. vol 5, 4th edn. Saunders, Philadelphia, pp 3563–3574
Jannetta PJ, Abbasy M, Maroon JC, Ramos FM, Albin MS (1977) Etiology and definitive microsurgical treatment of hemifacial spasm. Operative techniques and results in 47 patients. J Neurosurg 47:321–328
Kalkanis SN, Eskandar EN, Carter BS, Barker FG 2nd (2003) Microvascular decompression surgery in the United States, 1996 to 2000: mortality rates, morbidity rates, and the effects of hospital and surgeon volumes. Neurosurgery 52:1251–1261, discussion 1261–1252
Kondo A (1997) Follow-up results of microvascular decompression in trigeminal neuralgia and hemifacial spasm. Neurosurgery 40:46–51, discussion 51–42
Kong DS, Park K, Shin BG, Lee JA, Eum DO (2007) Prognostic value of lateral spread response (LSR) in the intraoperative monitoring of facial EMG during microvascular decompression for hemifacial spasm. J Neurosurg 106:384–387
Kurokawa Y, Maeda Y, Toyooka T, Inaba K (2004) Microvascular decompression for hemifacial spasm caused by the vertebral artery: a simple and effective transposition method using surgical glue. Surg Neurol 61:398–403
Kuroki A, Itagaki S, Nagai O (1991) Delayed facial palsy after microvascular decompression for hemifacial spasm. Facial Nerve Res 11:147–150
Kwak HJ, Kim JH, Lee JK et al (2001) Results of microvascular decompression in hemifacial spasm. J Korean Neurosurg Soc 30:501–508
Lovely TJ, Getch CC, Jannetta PJ (1998) Delayed facial weakness after microvascular decompression of cranial nerve VII. Surg Neurol 50:449–452
Lunsford L, Niranjan A, Konziolka D (2007) Surgical management options for trigeminal neuralgia. J Korean Neurosurg Soc 41:359–366
Magnan J, Caces F, Locatelli P, Chays A (1997) Hemifacial spasm: endoscopic vascular decompression. Otolaryngol Head Neck Surg 117:308–314
McLaughlin MR, Jannetta PJ, Clyde BL, Subach BR, Comey CH, Resnick DK (1999) Microvascular decompression of cranial nerves: lessons learned after 4400 operations. J Neurosurg 90:1–8
Moller AR, Jannetta PJ (1985) Microvascular decompression in hemifacial spasm intraoperative electrophysiological observations. Neurosurgery 16:612–618
Moller AR, Jannetta PJ (1987) Monitoring facial EMG responses during microvascular decompression operations for hemifacial spasm. J Neurosurg 66:681–685
Park JS, Kong DS, Lee JA, Park K (2007) Intraoperative management to prevent cerebrospinal fluid leakage after microvascular decompression: dural closure with a “plugging muscle” method. Neurosurg Rev 30:139–142
Park JS, Kong DS, Lee JA, Park K (2008) Hemifacial spasm: neurovascular compressive patterns and surgical significance. Acta Neurochir (Wien) 150:235–241
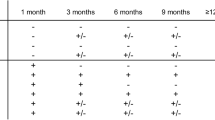
Park JS, Kong DS, Lee JA, Park K (2008) Chronologic analysis of symptomatic change following microvascular decompression for hemifacial spasm: value for predicting midterm outcome. Neurosurg Rev 31:413–418, discussion 418–419
Rhee DJ, Kong DS, Park K, Lee JA (2006) Frequency and prognosis of delayed facial palsy after microvascular decompression for hemifacial spasm. Acta Neurochir (Wien) 148:839–843, discussion 843
Samii M, Gunther T, Iaconetta G, Muehling M, Vorkapic P, Samii A (2002) Microvascular decompression to treat hemifacial spasm: long-term results for a consecutive series of 143 patients. Neurosurgery 50:712–718, discussion 718–719
Sindou M, Howeidy T, Acevedo G (2002) Anatomical observations during microvascular decompression for idiopathic trigeminal neuralgia (with correlations between topography of pain and site of the neurovascular conflict): prospective study in a series of 579 patients. Acta Neurochir (Wien) 144:1–13
Sindou M, Keravel Y, Moller A (1997) Hemifacial spasm. A multidisciplinary approach. Springer, Wien
Sindou MP (2005) Microvascular decompression for primary hemifacial spasm. Importance of intraoperative neurophysiological monitoring. Acta Neurochir (Wien) 147:1019–1026
Author information
Authors and Affiliations
Corresponding author
Additional information
Disclaimer
None of the authors has any financial interest in the subject under discussion in this paper.
Comments
Takanori Fukushima, Raleigh, North Carolina, USA
Dr. Seung-Jae Hyun and his co-authors presented a large Korean series of patients with hemifacial spasm. Hemifacial spasm is a very annoying and distressing disorder of one side of the face with repetitive tonic and clonic involuntary spasm or twitching. The facial disorder has a much higher incidence among Orientals, Chinese, Korean, and Japanese people due to the fact that most oriental people have anthropological features of brachycephaly (round or flat head); whereas Caucasian people have more frequency of trigeminal neuralgia because of their dolichocephalic head. Dr. Hyun’s article is well written with meticulous analysis of the clinical presentation and operative results in 1,174 cases. Essentially, their results are somewhat similar to my previous paper on 2,890 cases with hemifacial spasm published in 1995. My series demonstrated 5% of incomplete results or late recurrence. The majority of these unfavorable outcomes were due to complex vertebral artery compression or adhesion of the shredded Teflon tape with the facial nerve. I noted significant adhesion of all processes such as Teflon, Ivalon, or nylon sponges in between the facial nerve and offending vessel in recurrent hemifacial spasm cases operated elsewhere. In my experience, I am confident that microvascular decompression is not the insertion of processes in between the nerve and vessels but transposition and repositioning of the offending vessels is the key element of this surgical technique. I wish to emphasize that any insertion procedure with any processes will result in 5–10% of persistent spasm or result in later recurrences.
Marc Sindou, Lyon, France
This is a very large series with excellent results, from a well-recognized neurosurgical team. In our opinion, the authors’ grading system of severity of spasms deserves to be used by the neurosurgical community. It should help to quantify the patient’s disability, evaluate the post-op effect in a same patient, and allow comparison of results between series. We also appreciate the authors’ classification of neurovascular patterns. It should help surgeons to be prepared for safer surgery and also to codify more accurately the operative records for clinical studies.
We do agree that intraoperative monitoring of BAEP is a wise precaution, at least at the beginning of experience until learning curve has improved and stabilizes. This teaches that the approach should be infra-flocular to reach the ventro-caudal Root Exit Zone of the facial nerve, without stretching the VIIth–VIIIth nerve complex. We do not think that intraoperative EMG monitoring of Lateral Spread Responses is that much of practical interest, due to lack of reliability. That said, this method set up by A. Moller was brilliant to demonstrate the role of the hyperactivity of the facial motor nucleus in the pathophysiology of the disease. Besides, we agree with the relatively high occurrence of a delayed facial palsy after MVD. Although reversible in most cases, this eventuality should be mentioned in the informed consent that the patient must sign. We also agree on the high incidence of delayed cure, and that patient should not be offered a re-operation before 1 year, at least in the eventuality of persistence of spasms after surgery. In our series of 180 patients, we observed a delayed cure of 3 months on average in 36% of the patients and of 3 years (!) in three of them.
Finally, the authors have to be acknowledged for bringing their extensive and deeply analyzed experience to the neurosurgical community.
Toshio Matsushima, Saga, Japan
This is a paper on the large number of surgical cases of hemifacial spasm and the authors showed very good surgical results. Their results were due to good knowledge of the anatomy, sufficient intraoperative monitoring, and a large number of experiences in a short time. I found it very interesting that they obtained the good results only with the interposing technique. One of the debating subjects is how to decompress the offending large vertebral artery. About this point, I wish they had explained more clearly to readers. I am also interested in their four cases with the offending vein. During surgery, we often see a vein crossing the exit zone of the facial nerve even in cases with the offending arteries. The vein is usually adherent to the neural tissue of the pons. Therefore, I am wondering how the vein was compressing the REZ in the four cases and how they judged the vein was an offending vessel. I hope they continue their clinical studies and clarify the points I brought up here.
The submitted manuscript does not contain information about medical devices or drugs.
No funds were received in support of this work. No benefits in any form have been or will be received from a commercial party related directly or indirectly to the subject of this manuscript.
Rights and permissions
About this article
Cite this article
Hyun, SJ., Kong, DS. & Park, K. Microvascular decompression for treating hemifacial spasm: lessons learned from a prospective study of 1,174 operations. Neurosurg Rev 33, 325–334 (2010). https://doi.org/10.1007/s10143-010-0254-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10143-010-0254-9